Abstract
We report a very rare case of cervical compressive myelopathy by an anomalous bilateral vertebral artery (VA) entering the spinal canal at the C1 level and compressing the spinal cord. A 70-year-old woman had been suffering from progressive gait disturbance. Magnetic resonance imaging revealed that a bilateral VA at the V4 segment had abnormal courses and caused compression to the high cervical cord. VA repositioning was performed by anchoring a suture between the artery and around the arachnoid membrane and dentate ligament, and then, microvascular decompression using a Teflon sponge was done between the VA and the spinal cord. The weakness in the patient improved in the lower extremity after the operation. Anomalous VA could be one of the rare causes of cervical compressive myelopathy. Additionally, an anchoring suture and microvascular decompression around the VA could be a sufficient and safe method to indirectly decompress the spinal canal.
Though a vertebral artery (VA) anomaly is rare, Tokuda et al.10) have reported that in a series of 300 VA angiograms, 2.3% had VA anomalies. Mostly cases are asymptomatic, but a few cases have been reported with cervical pain, occipital pain, and myelopathy.
Here, we report a rare case of cervical compressive myelopathy by an anomalous bilateral VA entering the spinal canal at the C1 level. VAs on both sides deeply indented into the spinal cord and resulted in symptomatic myelopathy. The surgical treatment of this rare case is discussed in the case report.
A 70-year-old woman, recently diagnosed with hypertension, presented with symptoms of gradually progressive gait disturbance and weakness in lower extremities for about 8 months. When she was admitted, she could not go up a flight of stairs alone. Neurologic examination revealed grade III paraparesis of both upper and lower extremities. Sensory examination was intact to pain, touch, temperature and proprioception. The long tract signs were positive on both sides such as hyperreflexia, toe sign and the Hoffmann sign.
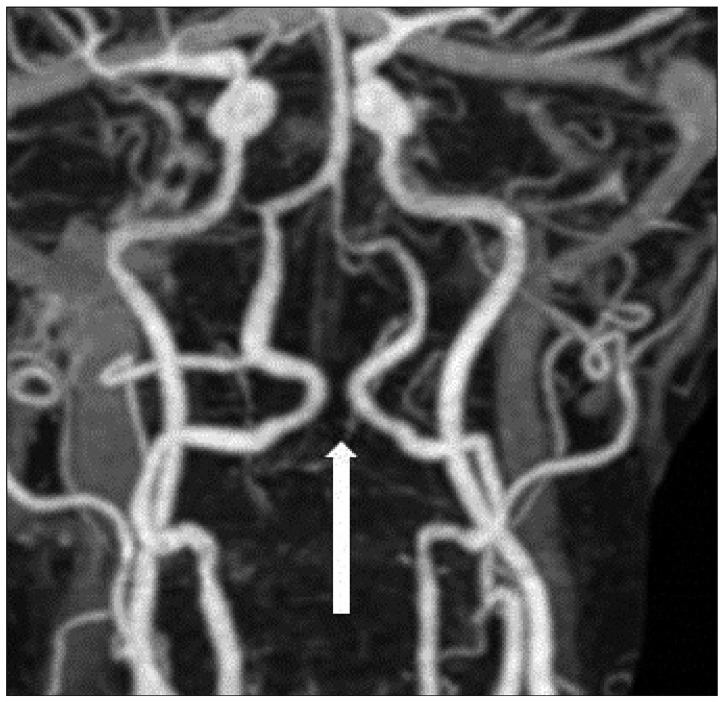
MRI revealed large flow voids in the region of the craniovertebral junction that resulted in compression of the cord (Fig. 1). Computed tomography (CT) angiography revealed bilateral vertebral arteries looped medially, like having the appearance of kissing each other on the dorsal surface and deeply indented into the cord substance (Fig. 2). There were no other bone or soft tissue anomalies in the region.
A midline suboccipital craniotomy with C1 laminotomy and C2 partial laminectomy for preserving paraspinal muscle of C2 was performed. Dura was incised from foramen magnum to C2 level. Both vertebral arteries were showed tortuous, looped medially each other on the posterolateral surface of the cord, and spinal cord was compressed by them. First, right side arachnoid membrane around VA was dissected and excised dentate ligament to release VA from spinal cord. And then anchoring suture from VA to the arachnoid membrane and dentate ligament was made using 6-0 nylon. And then Teflon sponge was inserted to the space between VA and the spinal cord for microvascular decompression. Same procedure was performed to left VA and enough decompression was achieved. At the end of the operation we repaired occipital bone flap & C1 lamina.
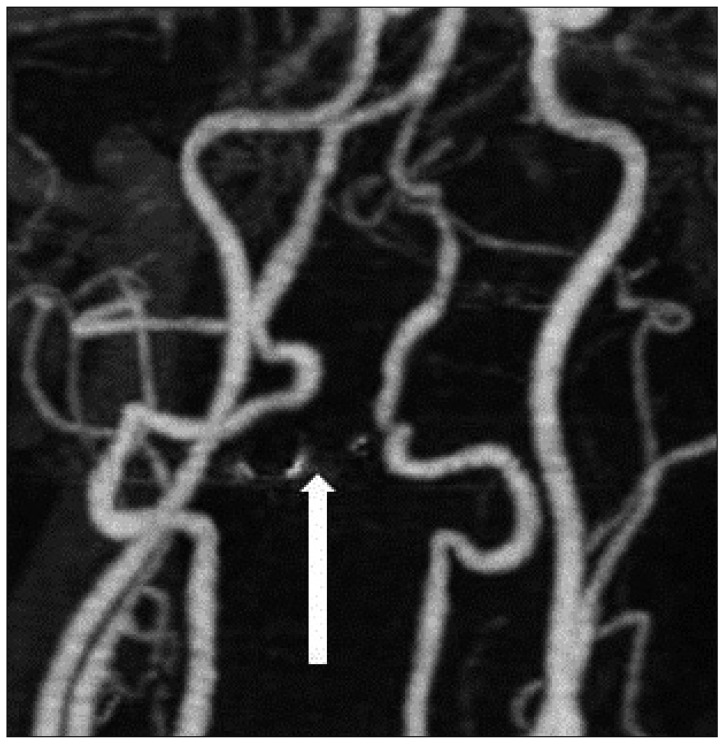
A postoperative CT angiography was immediately obtained and it showed that the bilateral.
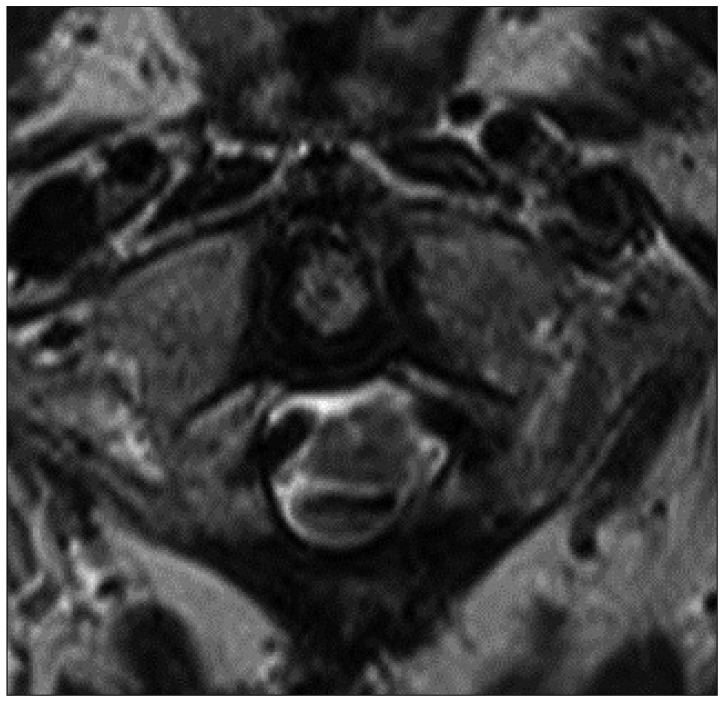
VAs were separated from each other without interruption in blood flow at the C1 level (Fig. 3). She could walk and go up a flight of stairs at the one month follow-up and the symptoms of the patient gradually improved over 2 years of the postoperative period. Six months after the operation, the MRI showed the full recovery of the spinal cord contour and the laterally transposed VA (Fig. 4).
A driving aberrant VA course is a clinical problem sometimes at the time of surgery such as ACDF or posterior C1-2 fixation. However, ectatic and anomalous vertebral arterial loops resulting in cord compression have been identified only rarely1,2,4-9,11). From literature review, the authors found isolated 14 cases of symptomatic cord compression due to anomalous VA. While two patients had evidence of myelopathy, rest of the cases had symptoms that could be related to nerve root compression and manifested as neck pain, arm pain or torticollis1,2,4-9,11).
The pathophysiology of this phenomenon is unclear. Continuous pulsations of the large arteries over long period might be apparently the cause of compressive myelopathy.
Hasegawa et al.3) proposed a hammering effect to the spinal cord by the arterial pulsation of the anomalous VA based on arteriosclerosis. As in the previous reports, we also suggest that intermittent stimulation of the spinal cord by the anormalous vertebral artery was responsible for the cervical myelopathy in our case. MRI, CT angiography and/or cerebral angiography are the investigations of choice to diagnose such patients.
Treatment options for patients with anomalous VA with root or cord compression include vessel transposition, duroplasty, detachment of roots from the vertebral arteries or the placement of inert material between the vessel and the cord. One of them is microvascular decompression. Since Jannetta4) introduced this microvascular decompressive technique, it has been used to treat disorders such as hemifacial spasm and trigeminal neuralgia. Most commonly, prosthesis such as muscle graft or sponge is inserted into the space between the responsible vessel and the affected nerve or brainstem region to transpose the responsible vessel and resolve the pulsatile pressure on the nerve fiber. Following bilateral vasculopexy, the cervicomedullary junction was relieved of compression resulting in lasting relief of the symptoms of the patient.
In the present case, VA at V4 segment entered the spinal canal and formed a kissing loop on the dorsal surface of the cord. Anomalous course of VA resulted in cervical compressive myelopathy.
The patient underwent surgery of vertebral artery repositioning by anchoring suture between artery and around arachnoid membrane and dentate ligament and microvascular decompression using insertion of Teflon to the space between vertebral artery and the spinal cord. After surgery, clinical symptom and radiologic follow-up such as CT angiography and MRI were both satisfactorily improved.
Anomalous vertebral artery could be one of the rare causes for cervical compressive myelopathy. Even though it is rare, we should include vertebral artery anomaly in the differential diagnosis of upper cervical lesions presenting with cervical myelopathy. Additionally, an anchoring suture and microvascular decompression around the VA could be a sufficient and safe method to indirectly decompress the spinal canal.
References
1. Furumoto T, Nagase J, Takahashi K, Itabashi T, Iai H, Ishige N. Cervical myelopathy caused by the anomalous vertebral artery. A case report. Spine (Phila Pa 1976). 1996; 21:2280–2283. PMID: 8902976.
2. Goel A, Shah A. Trigeminal neuralgia in the presence of ectatic basilar artery and basilar invagination : treatment by foramen magnum decompression. J Neurosurg. 2009; 111:1220–1222. PMID: 19558301.

3. Hasegawa T, Kubota T, Ito H, Yamamoto S. Symptomatic duplication of the vertebral artery. Surg Neurol. 1983; 20:244–248. PMID: 6879426.

4. Jannetta PJ. Observations on the etiology of trigeminal neuralgia, hemifacial spasm, acoustic nerve dysfunction and glossopharyngeal neuralgia. Definitive microsurgical treatment and results in 117 patients. Neurochirurgia (Stuttg). 1977; 20:145–154. PMID: 198692.

5. Satoh S, Yamamoto N, Kitagawa Y, Umemori T, Sasaki T, Iida T. Cervical cord compression by the anomalous vertebral artery presenting with neuralgic pain. Case report. J Neurosurg. 1993; 79:283–285. PMID: 8331414.

6. Suzuki S, Tsuchita H, Kurokawa Y, Kitami K, Sohma T, Takeda T. New method of MVD using a vascular tape for neurovascular compression involving the vertebrobasilar artery--report of two cases. Neurol Med Chir (Tokyo). 1990; 30:1020–1023. PMID: 1714048.

7. Takahashi T, Tominaga T, Hassan T, Yoshimoto T. Cervical cord compression with myelopathy caused by bilateral persistence of the first intersegmental arteries : case report. Neurosurgery. 2003; 53:234–237. discussion 237. PMID: 12823896.

8. Takahashi Y, Sugita S, Uchikado H, Miyagi T, Tokutomi T, Shigemori M. Cervical myelopathy due to compression by bilateral vertebral arteries--case report. Neurol Med Chir (Tokyo). 2001; 41:322–324. PMID: 11458746.

9. Takei H, Sagae M, Chiba K, Ogino T. The long-term follow-up of surgical treatment for cervical myelopathy with severe nape and upper arm pain caused by the anomalous vertebral artery : case report. Spine (Phila Pa 1976). 2008; 33:E611–E613. PMID: 18670330.
10. Tokuda K, Miyasaka K, Abe H, Abe S, Takei H, Sugimoto S, et al. Anomalous atlantoaxial portions of vertebral and posterior inferior cerebellar arteries. Neuroradiology. 1985; 27:410–413. PMID: 4058734.

11. Watanabe K, Hasegawa K, Takano K. Anomalous vertebral artery-induced cervical cord compression causing severe nape pain. Case report. J Neurosurg. 2001; 95(1 Suppl):146–149. PMID: 11453419.

Fig. 1
A : Preoperative MRI. Midsagittal T2-weighted image shows a signal void region (arrow) at the C1 level. B : Axial T2-weighted image shows the compression of the spinal cord in the bilateral posterolateral region.
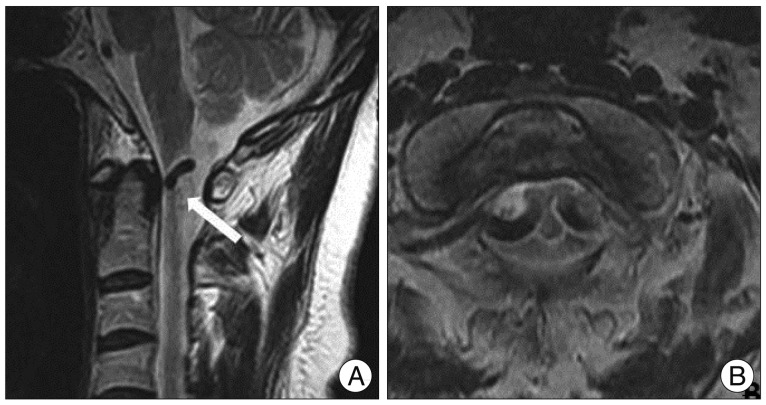
Fig. 2
Preoperative CT angiography shows a medially looped bilateral VA and has a kissing appearance at the C1 level.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download