Abstract
A 55-year-old female patient presented with lower back pain and neurogenic intermittent claudication and underwent L3-L4 posterolateral fusion. To prepare the bone fusion bed, the transverse process of L3 and L4 was decorticated with a drill. On the 9th post-operative day, the patient complained of a sudden onset of severe abdominal pain and distension. Abdominal computed tomography revealed retroperitoneal hematoma in the right psoas muscle and iatrogenic right L3 transverse process fracture. Lumbar spinal angiography showed the delayed hematoma due to rupture of the 2nd lumbar artery pseudoaneurysm and coil embolization was done at the ruptured lumbar artery pseudoaneusyrm. Since then, the patient's postoperative progress proceeded normally with recovery of the hemodynamic parameters.
Iatrogenic injury of the lumbar arteries after spinal surgery is a rare complication5-9). It may result in the formation of a pseudoaneurysm and consequent acute or delayed retroperitoneal hemorrhage. Because pseudoaneurysm develops gradually from a focal arterial wall disruption, it may go unnoticed by the surgeon. However, this condition may lead to a sudden and massive retroperitoneal hemorrhage and hypovolemic shock. We recently treated a patient who showed a large retroperitoneal hematoma caused by pseudoaneurysm that arose nine days after posterolateral fusion (PLF).
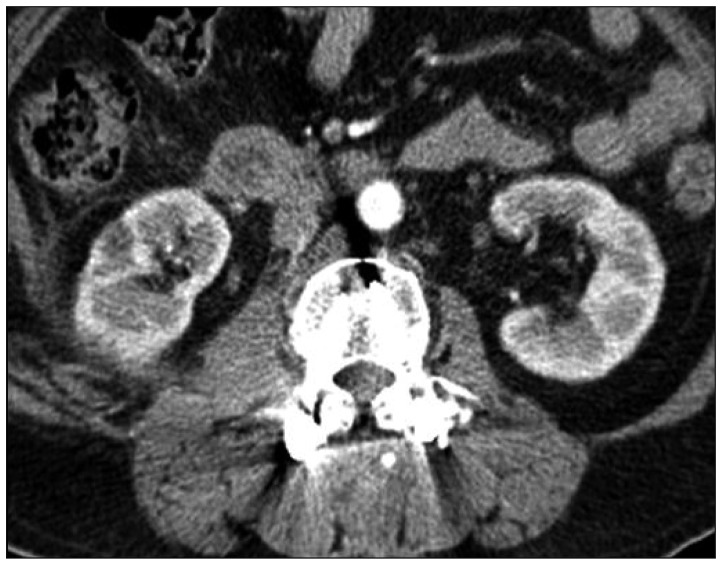
A 55-year-old female patient with lower back pain and neurogenic intermittent claudication, who previously underwent L4-L5 PLF due to spinal stenosis, was presented to our hospital. She experienced small thalamic infarction 5 years ago, and since then, she started antiplatelet and antihypertensive medications. Lumbar spine magnetic resonance image revealed L3-L4 spinal stenosis due to adjacent segment degeneration. Hence, the patient underwent L3-L4 PLF. To prepare the bone fusion bed, the transverse process of L3 and L4 was decorticated with a drill. There was minimal bleeding during the surgery, and post-operative complaints only include mild back pain. However, on the 9th post-operative day, the patient complained of a sudden onset of severe abdominal pain and distension. Moreover, the patient was hemodynamically unstable (8.5 g/dL hemoglobin concentration; 90/60 mm Hg blood pressure; and 120/minute pulse rate). A late abdominal complication was suspected, and an emergency computed tomography (CT) scan of the abdomen with contrast enhancement was performed. This investigation revealed retroperitoneal hematoma in the right psoas muscle (Fig. 1A) and iatrogenic right L3 transverse process fracture (Fig. 1B). The patient was resuscitated with blood transfusion, intravenous fluids for hypovolemic shock and an interventional radiologist was urgently consulted. Lumbar spinal angiography showed the delayed hematoma due to rupture of the 2nd lumbar artery pseudoaneurysm (Fig. 2A) and coil embolization was done at the ruptured lumbar artery (Fig. 2B). After we confirmed the successful embolization through the final angiogram, the patient was sent to the ward. Since then, the patient's postoperative progress proceeded normally with recovery of the hemodynamic parameters. Two weeks after the embolization, follow-up abdominal CT showed the decreased retroperitoneal hematoma (Fig. 3).
A few authors reported iatrogenic lumbar artery pseudoaneurysm as a consequence of spinal surgery4-8). Moreover, there were some reports about lumbar artery pseudoaneurysm after trauma1-3,11). However, there were few reports about lumbar artery pseudoaneurysm after PLF. In 1953, Watkins12) first introduced posterolateral intertransverse fusion and the indications for the use of this technique have been broadened to include degenerative disc disease and low back pain. Nowadays, this technique is supplemented by the provision of a transpedicular fixation device and is widely used in lumbosacral spinal surgery. Preparation of the bone fusion bed, which is the most important step in PLF, was done through decortications of the transverse process by drilling. In the present case, the fracture of the right L3 transverse process was connected, thus the injury of the lumbar artery may have occurred close to the transverse process during drilling. We believe that this iatrogenic arterial wall injury was responsible for the formation of the lumbar artery pseudoaneurysm with the consequent delayed retroperitoneal hemorrhage.
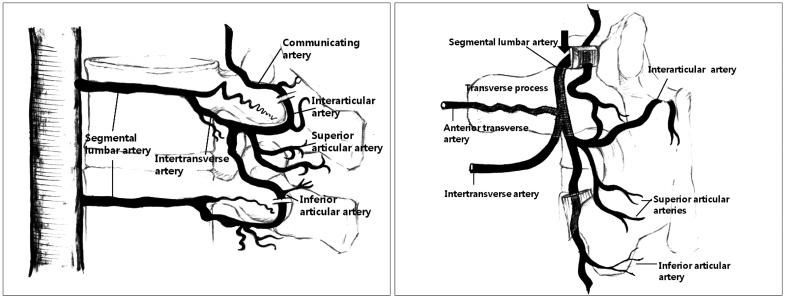
The lumbar arteries of L1 to L4 are small paired vessels that originate from the dorsal aspect of the abdominal aorta at the level of the transverse processes. The lower lumbar arteries can occasionally originate from a common trunk near the midline of the posterior aorta (Fig. 4A). These vessels run laterally along the bodies of the lumbar vertebrae and divide into anterior and posterior branches at the medial border of the psoas muscle and anterior of the transverse process1). In the present case, we thought that the lumbar artery was injured at the anterior of the transverse process (Fig. 4B). Lee et al.4) reported the case of a lumbar artery injury combined with a transverse process fracture after a fall. Thus if the patient showed retroperitoneal hemorrhage along with a transverse process fracture, the clinician should consider the possibility of a lumbar artery injury.
In case of retroperitoneal hemorrhage due to lumbar artery injury, endovascular embolization is effective in controlling hemorrhage as it avoids the risks associated with another anesthesia, surgical incision, and the locating and controlling the bleeding1,7,9,10). In our case, a transcatheter embolization has successfully stopped retroperitoneal hemorrhage due to rupture of lumbar artery pseudoaneurysm.
We described a case of lumbar artery pseudoaneurysm after PLF of the lumbar spine. Although PLF is a safe and widespread surgical technique, major complications are possible if proper attention is not given to the preparation of fusion bed such as drilling or decortication of a transverse process. Surgeons are therefore required to be extra careful during decortication to avoid complications.
References
1. Chan KT, Korivi N. Lumbar artery pseudoaneurysm in traumatic spinal cord injury : a case report. Arch Phys Med Rehabil. 2003; 84:455–457. PMID: 12638116.

2. Domenicucci M, Ramieri A, Lenzi J, Fontana E, Martini S. Pseudo-aneurysm of a lumbar artery after flexion-distraction injury of the thoraco-lumbar spine and surgical realignment : rupture treated by endovascular embolization. Spine (Phila Pa 1976). 2008; 33:E81–E84. PMID: 18303450.
3. Hamid RS, ul HT, Chishti I, Azeemuddin M. Post traumatic avulsion of lumbar artery : a rare cause of retroperitoneal haemorrhage treated by glue embolization. J Pak Med Assoc. 2010; 60:487–489. PMID: 20527650.
4. Lee JS, Kim CW, Suh KT. Lumbar artery injury combined with a transverse process fracture of the lumbar spine presenting with hypovolemic shock after a fall : a case report. J Korean Orthop Assoc. 2008; 43:400–403.

5. Lee KH, Park JH, Chung JW, Han JK, Shin SJ, Kang HS. Vascular complications in lumbar spinal surgery : percutaneous endovascular treatment. Cardiovasc Intervent Radiol. 2000; 23:65–69. PMID: 10656911.

6. Lee WJ, Eun JP, Choi HY, Lee JC. Retroperitoneal hematoma secondary to terminal branch of segmental artery injury during intertransverse discectomy through paramedian muscle splitting approach. J Korean Neurosurg Soc. 2004; 36:246–248.
7. Nijenhuis RJ, Sluzewski M, van Rooij WJ. Iatrogenic lumbar pseudoaneurysm causing dural sac compression after spine surgery. J Neurosurg Spine. 2009; 10:585–586. PMID: 19558292.

8. Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, Tsolakis JA. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002; 24:189–195. PMID: 12217278.

9. Santillan A, Patsalides A, Gobin YP. Endovascular embolization of iatrogenic lumbar artery pseudoaneurysm following extreme lateral interbody fusion (XLIF). Vasc Endovascular Surg. 2010; 44:601–603. PMID: 20675335.

10. Sclafani SJ, Florence LO, Phillips TF, Scalea TM, Glanz S, Goldstein AS, et al. Lumbar arterial injury : radiologic diagnosis and management. Radiology. 1987; 165:709–714. PMID: 3685349.

11. Siablis D, Panagopoulos C, Karamessini M, Karnabatidis D, Margariti S, Tepetes K, et al. Delayed diagnosis of a false aneurysm after lumbar arterial injury : treatment with endovascular embolization : a case report. Spine (Phila Pa 1976). 2003; 28:E71–E73. PMID: 12590222.
12. Watkins MB. Posterolateral fusion of the lumbar and lumbosacral spine. J Bone Joint Surg Am. 1953; 35-A:1014–1018. PMID: 13108907.

Fig. 1
A : Abdominal enhanced computerized tomography (CT) image showing retroperitoneal hematoma (arrow) in the right psoas muscle around L3 vertebral body. B : CT bone setting image shows the fracture of right L3 transverse process (arrow).
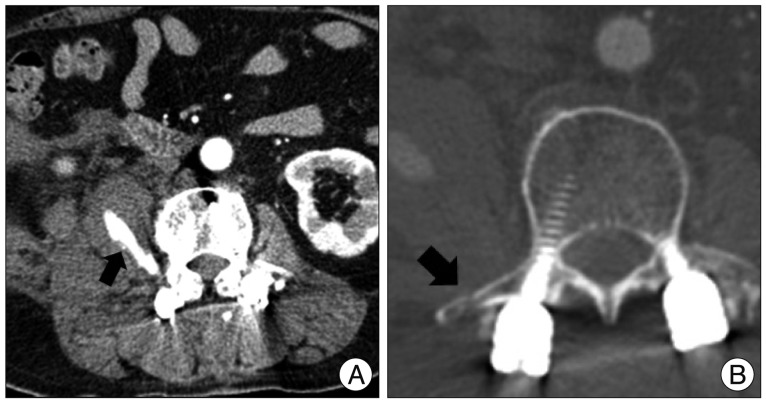
Fig. 2
A : Lumbar spinal angiography shows the delayed hematoma due to rupture of the 2nd lumbar artery pseudoaneurysm. B : Lumbar spinal angiography obtained after coil embolization shows no leakage of the contrast media.
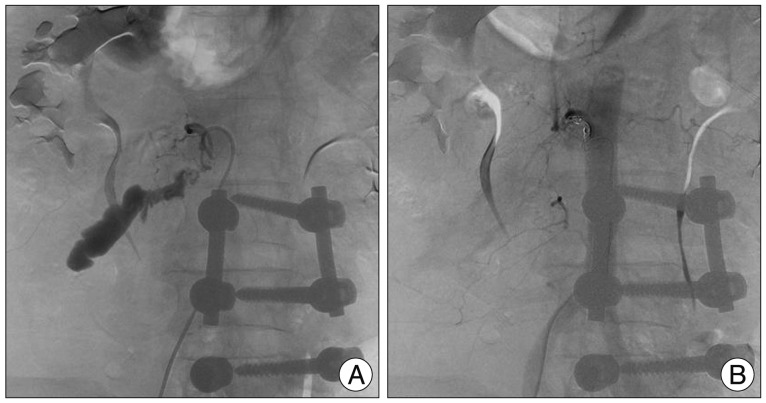
Fig. 4
The lower lumbar arteries can occasionally originate from a common trunk near the midline of the posterior aorta, and these vessels run laterally along the bodies of the lumbar vertebrae and divide into anterior and posterior branches at the medial border of the psoas muscle and anterior of the transverse process. Arrow shows the possible lumbar artery injury site.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download