Abstract
A 65-year-old man who had lateral cervical disc herniation underwent cervical posterior laminoforaminotomy at C5-6 and C6-7 level right side. During the operation, there was no serious surgical bleeding event. After operation, he complained persistent right shoulder pain and neck pain. Repeated magnetic resonance image (MRI) showed diffuse cervical epidural hematoma (EDH) extending from C5 to T1 level right side and spinal cord compression at C5-6-7 level. He underwent exploration. There was active bleeding at muscular layer. Muscular active bleeding was controlled and intramuscular hematoma was removed. The patient's symptom was reduced after second operation. Symptomatic postoperative spinal EDH requiring reoperation is rare. Meticulous bleeding control is important before wound closure. In addition, if patient presents persistent or aggravated pain after operation, rapid evaluation using MRI and second look operation is needed as soon as possible.
Cervical posterior laminoforaminotomy using microendoscopic tubular retractor system (METRx) is microsurgical technique useful for treatment of cervical lateral soft disc herniation or osteophytic spur8,12,15,16,18). Its surgical technique is simple and requires minimal instruments. Incision is small and normal posterior cervical anatomy is sacrificed minimally, thus cervical stability can be preserved well5,6,15). Moreover, due to relatively low complication rate, this surgical technique has gained popularity. Among complications, despite minimal blood loss, possibility of postoperative cervical epidural hematoma (EDH) is extremely rare. The authors report a case of cervical EDH after cervical posterior laminoforaminotomy and consider its causes.
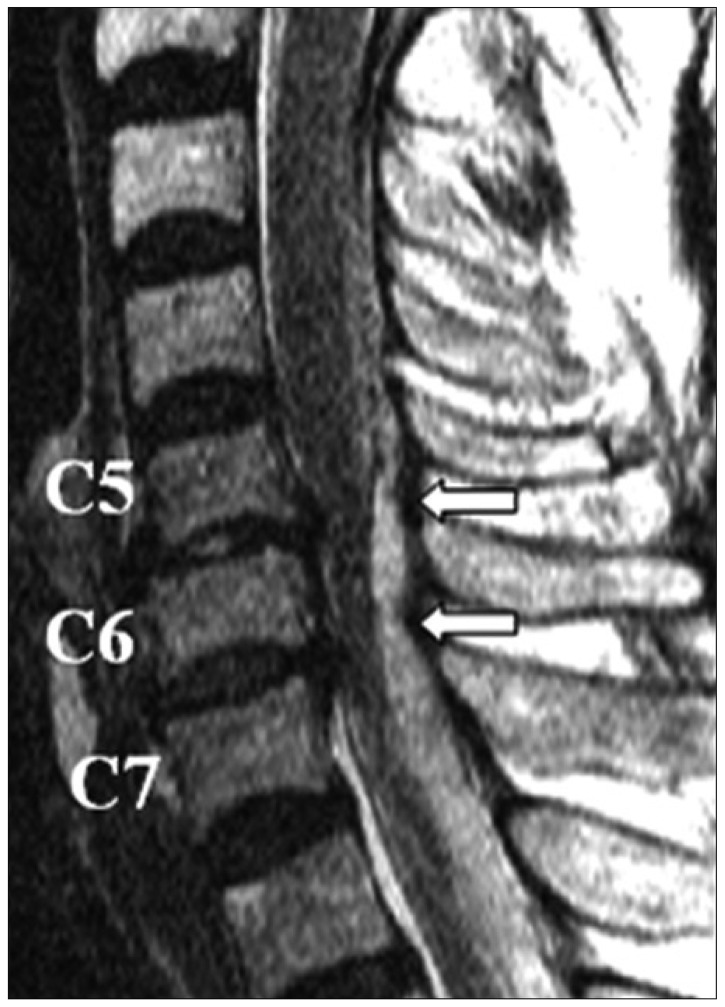
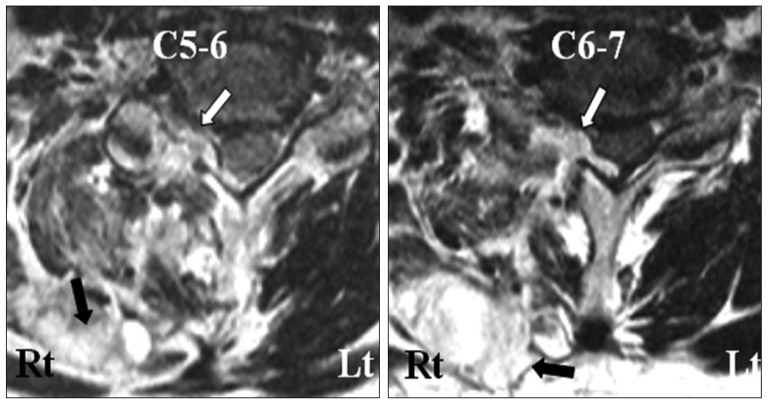
A 65-year-old man presented with neck pain and right arm pain radiated from shoulder to finger tip 4 weeks ago. Nonoperative supportive treatment including medication, physiotherapy, and injection did not relieve the patient's symptom. The patient could not extend his neck because of severe neck and shoulder pain. On neurologic examination, his right elbow flexion and extension were grade IV- and Spurling sign was elicited on his right arm. MRI showed disc herniation and foraminal stenosis at C5-6 and C6-7 right side (Fig. 1, 2). He underwent cervical posterior laminoforaminotomy at C5-6 and C6-7 right side. At operation, there was severe foraminal stenosis, and we confirmed decompression of nerve root successfully. There was no serious bleeding. After operation, he complained persistent right shoulder and arm pain. Repeated MRI showed cervical EDH extending from C5 to T2 right side and spinal cord compression at C5-6-7 due to EDH, also intramuscular and subcutaneous hematoma were seen (Fig. 3, 4). He underwent exploration. We extended skin incision more widely and carefully dissected muscle. There was active bleeding at muscular layer and small amount of oozed bleeding at epidural space. Muscular active bleeding was controlled and intramuscular hematoma was removed. Wide laminectomies including further medial facetectomy at C5-6 and C6-7 level were performed. The hematoma in muscular layer and EDH compressing the cervical cord were carefully removed by suction and irrigation. There was minimal oozed epidural bleeding. Meticulous hemostasis was performed, and we assured that there was no another bleeding. We closed operation wound as usual manner with drain insertion. Patient's symptom was improved after hematoma evacuation. After postoperative 6 months, he presented with slight tingling sense of right finger tip.
Lateral cervical disc herniation which causes brachialgia and neurologic symptoms was first reported in 194313). Since then, cervical posterior laminoforaminotomy for treatment of lateral cervical disc herniation was developed by many surgeons and brought with good results. The best candidate is the patient who presented with purely radicular symptoms due to lateral foraminal disc herniation or osteophyte7,8,12,15,16,18). This minimally invasive surgical technique decreases operation time, postoperative pain, blood loss and muscle injury. Also, this technique preserves cervical motion, does not cause instability nor need for internal or external bracing, and eliminates risk of swallowing or voice-related complications4,5). Therefore, it has been widely used and it can be performed by using microendoscopic and full-endoscopic techniques successfully1,12).
Many studies about cervical posterior laminoforaminotomy reported with good result and no serious complications. According to the literatures, complication rate of cervical posterior laminoforaminotomy was reported about 0% to 10.1%3-5,7,8,15,16). Complications were wound infection, wound separation, transient neurologic deterioration, dural laceration and cerebrospinal fistula etc. There was no postoperative cervical EDH.
Symptomatic postoperative spinal EDH requiring reoperation after overall spinal surgery is rare complication. Incidence is reported about 0.1 to 3%2,10,11,14,17). In case of cervical posterior laminoforaminotomy, symptomatic postoperative cervical EDH requiring reoperation had not been reported yet as far as we know. Despite very low incidence, it is important to diagnose postoperative cervical EDH as soon as possible. Rapid diagnosis and immediate hematoma evacuation can reduce neurologic deficit and result in greater neurological recovery. If treatment is delayed, postoperative cervical EDH can lead to catastrophic complications. In one study, revision surgery performed within 10 hours of symptom onset resolved all of patient's symptoms11). Another study reported that greater neurological recovery occurred when interval from symptom onset to surgery was short9). In this study, patient taken to surgery within 12 hours had better neurological outcomes than patients whose surgery was delayed beyond 12 hours. In addition to interval from symptom onset to surgery, severity of preoperative neurologic deficits correlated with surgical outcome14).
There are some studies about risk factors of postoperative spinal EDH. One study reported that multilevel procedure and coagulopathy were risk factors of postoperative spinal EDH6). In another study, in their 9 patients, preexisting medical history postulated to increase postoperative spinal EDH were found in four patients, each of patients had multiple myeloma, end stage renal disease, liver cirrhosis and deep vein thrombosis with coumadization17). The other study reported that pre-operative risk factors of postoperative spinal EDH include age more than 60 years old, use of pre-operative non-steroidal anti-inflammatories and Rh-positive blood type group2). They also reported that intraoperative risk factors were involvement of more than five operative levels, haemoglobin <10 g/dL and blood loss >1 L, and postoperative risk factor was international normalized ratio >2.0 within first 48 hours. In our case, the patient was more than 60-year-old and Rh-positive blood type group.
Many surgeons believe that cervical EDH is originated from epidural venous plexus. It is helpful to use Valsalva maneuver to confirm additional epidural venous bleeding. However, there are another bleeding focuses. Bone bleeding, especially prepared fusion bed, and muscle bleeding can cause trouble. In our case, there was no serious bleeding before closure. However, postoperative MRI showed large intramuscular hematoma and cervical EDH. In exploration, there was active arterial bleeding in muscle layer. In our case, even though METRx may split paraspinal neck muscles including splenius capitus muscle, semispinalis capitus muscle and semispinalis cervicis muscle, there could be some dead space along the tubular insertion site and muscle-bone detachment site after the surgical procedures. Generally, postoperative hematoma can be placed at these spaces and hemorrhage stops if there is no further empty space. However, high pressure bleeding such as active arterial bleeding can enlarge the empty space and separate epidural space. Therefore, the epidural hematoma can be extended widely and it will cause the patient's symptoms. Thoracic epidural space is more prominent than cervical epidural space. Thus, we assume that the cervical epidural hematoma was extended to the thoracic epidural space in our case. Many surgeons think that drains are helpful to reduce postoperative spinal EDH, but it is controversial2,6).
Some authors reported about cause of postoperative spinal EDH. In one case about delayed postoperative cervical EDH after postoperative day 9, patient who underwent cervical laminectomy suddenly felt neck and shoulder pain while straining to defecation, and tetraplegia developed11). In exploration, there was arterial bleeding from muscle wall. They reported that hypertension, ingestion of anticoagulant agents, straining, sneezing, lifting, and vascular anomaly could predispose patients to postoperative spinal EDH. They recommended to advise patients to avoid strenuous activity after operation for a while. In another case about cervicothoracic EDH after anterior cervical surgery, authors thought that the cause was coughing during wake up from general anesthesia10).
Postoperative cervical EDH after cervical posterior laminoforaminotomy is extremely rare. However, active muscle bleeding can cause the epidural hematoma with mass effect through the small incision tract. Therefore, meticulous bleeding control is important before wound closure. In addition, if patient presents persistent or aggravated pain after operation, rapid evaluation using MRI and second look operation is needed as soon as possible.
References
1. Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy : results of a new technique in 100 cases. J Neurosurg. 2001; 95(1 Suppl):51–57. PMID: 11453432.

2. Awad JN, Kebaish KM, Donigan J, Cohen DB, Kostuik JP. Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br. 2005; 87:1248–1252. PMID: 16129751.

3. Henderson CM, Hennessy RG, Shuey HM Jr, Shackelford EG. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy : a review of 846 consecutively operated cases. Neurosurgery. 1983; 13:504–512. PMID: 6316196.

4. Holly LT, Moftakhar P, Khoo LT, Wang JC, Shamie N. Minimally invasive 2-level posterior cervical foraminotomy : preliminary clinical results. J Spinal Disord Tech. 2007; 20:20–24. PMID: 17285047.
5. Korinth MC, Krüger A, Oertel MF, Gilsbach JM. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease : results in 292 patients with monoradiculopathy. Spine (Phila Pa 1976). 2006; 31:1207–1214. discussion 1215-1216. PMID: 16688033.

6. Kou J, Fischgrund J, Biddinger A, Herkowitz H. Risk factors for spinal epidural hematoma after spinal surgery. Spine (Phila Pa 1976). 2002; 27:1670–1673. PMID: 12163731.

7. Krupp W, Schattke H, Müke R. Clinical results of the foraminotomy as described by Frykholm for the treatment of lateral cervical disc herniation. Acta Neurochir (Wien). 1990; 107:22–29. PMID: 2096604.

8. Kumar GR, Maurice-Williams RS, Bradford R. Cervical foraminotomy : an effective treatment for cervical spondylotic radiculopathy. Br J Neurosurg. 1998; 12:563–568. PMID: 10070468.

9. Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma : relationship between surgical timing and neurological outcome. J Neurosurg. 1995; 83:1–7. PMID: 7782824.

10. Lee DY, Lee SH. Cervicothoracic spinal epidural hematoma after anterior cervical spinal surgery. J Korean Neurosurg Soc. 2010; 48:541–543. PMID: 21430984.

11. Neo M, Sakamoto T, Fujibayashi S, Nakamura T. Delayed postoperative spinal epidural hematoma causing tetraplegia. Case report. J Neurosurg Spine. 2006; 5:251–253. PMID: 16961087.
12. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes : a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008; 33:940–948. PMID: 18427313.

13. Semmes RE, Murphey F. The syndrome of unilateral rupture of the sixth cervical intervertebral disc. JAMA. 1943; 121:1209–1214.

14. Uribe J, Moza K, Jimenez O, Green B, Levi AD. Delayed postoperative spinal epidural hematomas. Spine J. 2003; 3:125–129. PMID: 14589226.

15. Williams RW. Microcervical foraminotomy. A surgical alternative for intractable radicular pain. Spine (Phila Pa 1976). 1983; 8:708–716. PMID: 6320471.

16. Witzmann A, Hejazi N, Krasznai L. Posterior cervical foraminotomy. A follow-up study of 67 surgically treated patients with compressive radiculopathy. Neurosurg Rev. 2000; 23:213–217. PMID: 11153550.

17. Yi S, Yoon do H, Kim KN, Kim SH, Shin HC. Postoperative spinal epidural hematoma : risk factor and clinical outcome. Yonsei Med J. 2006; 47:326–332. PMID: 16807981.

18. Zeidman SM, Ducker TB. Posterior cervical laminoforaminotomy for radiculopathy : review of 172 cases. Neurosurgery. 1993; 33:356–362. PMID: 8413864.

Fig. 1
Sagittal magnetic resonance image showing disc herniation at C5-6 and C6-7 level (white arrows).
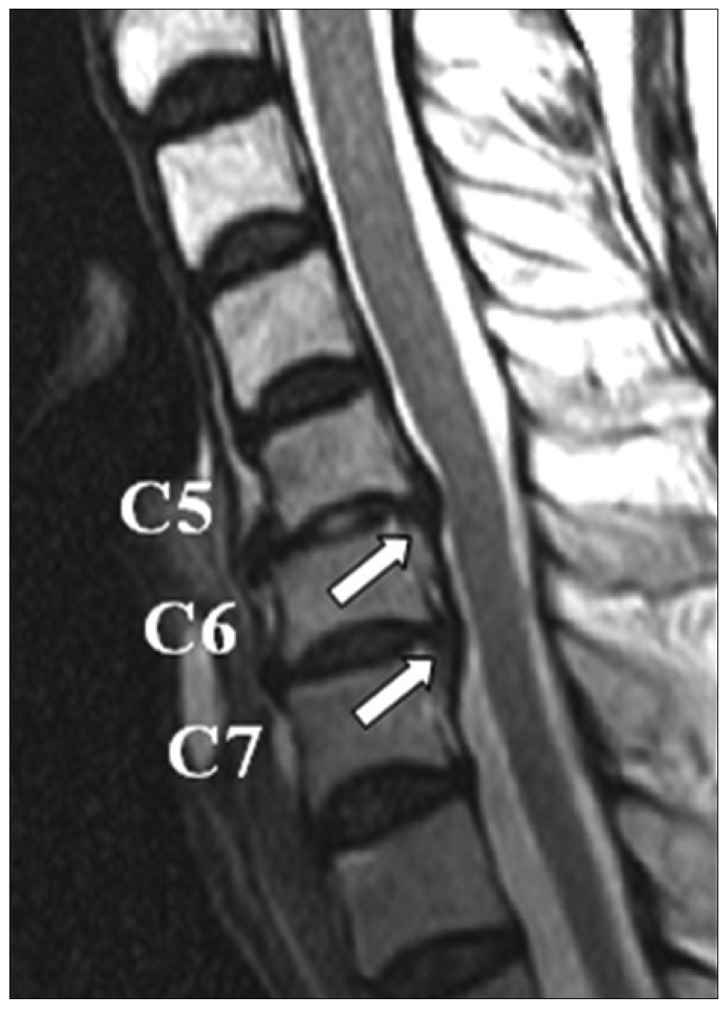
Fig. 2
Axial magnetic resonance image showing foraminal disc herniation right side at C5-6 and C6-7 level (white arrow).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download