Abstract
A 10-year-old female patient presented with a rapidly growing nodular mass lesion on her right frontal area. On skull radiography and computed tomography (CT) imaging, this mass had a well-demarcated punch-out lesion with a transdiploic, exophytic soft tissue mass nodule on the frontal scalp. Magnetic resonance (MR) imaging revealed the presence of a 1.5×1.2×1 cm sized calvarial lesion. This lesion was hypointense on T1 and heterogenous hyperintense on T2 weighted MR images, and exhibited heterogeneous enhancement of the soft tissue filling the punch-out lesion after intravenous administration of gadolinium. En block removal of the tumor with resection of the rim of the normal bone was performed. The pathological diagnosis was intravascular papillary endothelial hyperplasia (IPEH). After surgery, no recurrence was found for 8 months. IPEH is a rare and benign reactive lesion usually found in thrombosed subcutaneous blood vessels. Involvement of skull bone is rare. In this article, we present a case of IPEH involving the calvarium, in a 10-year-old woman.
Intravascular papillary endothelial hyperplasia (IPEH) is a benign, non-specific, vascular lesion consisting of reactive proliferation of the endothelial cells that arise in organizing thrombus16). IPEH is most commonly located in the skin or subcutaneous tissue, where it exhibits a benign clinical course, but has also occurred in many locations across the body. Intracranial occurrences of IPEH are rare. Due to its rarity, IPEH is often misdiagnosed radiologically7). On CT imaging, there is little differentiating IPEH from eosinophilic granuloma and other skull tumors, but gadolinium-enhanced MRI scans are useful in demonstrating the extremely vascular and hyperdense nature of IPEH4,10). However, there are no specific radiological features that characterize IPEH; hence, it is usually diagnosed after being treated surgically as another mass lesion, unless there is initially a high index of suspicion of the tumor.
We present the characteristic clinical, radiological, and pathological findings in a case of IPEH involving the calvarium.
A 10-year-old female patient, who was otherwise healthy, presented with a palpable mass on her right frontal skull, which had been present for 1 month. She had no history of head trauma or other medical illnesses. On physical examination, we observed a firm, painful, fixed mass of about 1.5 cm in diameter involving the right frontal bone. A routine skull X-ray showed a 1.2 cm sized punch-out lesion on the right frontal bone, without bone expansion or sclerosis (Fig. 1A). Computed tomography demonstrated a well-demarcated punch-out lesion with a transdiploic, exophytic soft tissue mass on the frontal scalp. The lesion had a central soft tissue component without brain invasion (Fig. 1B). Magnetic resonance (MR) imaging disclosed the presence of a 1.3×1.2×1 cm nodular mass (Fig. 2). This mass lesion was hypointense on T1 and heterogeneous hyperintense on T2 weighted MR images, and exhibited inhomogeneous enhancement of the soft tissue filling the punch-out lesion after intravenous administration of gadolinium.
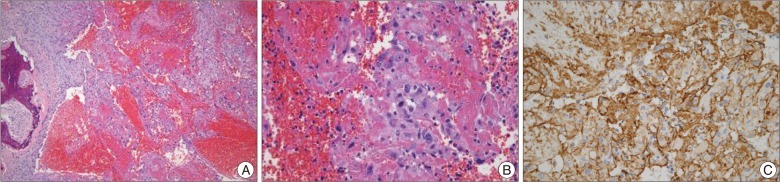
The skull lesion was completely removed, along with a wide margin, and a cranioplasty was performed. Gross examination of the specimen revealed a friable, brown colored lesion in the bone. Microscopic examination revealed some proliferation of epithelioid cells with hemorrhage and fibrin clots (Fig. 3A). In the center of the lesion, there were vague papillary configurations of epithelioid cells admixed with hemorrhage and fibrious materials. The epithelioid cells had slightly irregular nuclei with a vesicular chromatin pattern, and occasional distinctive nucleoli (Fig. 3B). In addition, there were a few mitotic figures. The peripheral portion showed some immature fibroblastic proliferations with inflammatory reactions. There was also focally metaplastic bone formation. This epithelial cells are positive for CD31 (Fig. 3C) and vimentin, a weekly positive for CD34 and CK, and negative for D2-40, EMA, LCA, S-100, HMB-45, CD21, CD68, CD3 and CD20. Histological findings were consistent with IPEH. The postoperative course was uneventful. At 8 months postoperatively, the patient was well and free of any symptoms or recurrence.
Intravascular papillary endothelial hyperplasia was first described in 1923 by Masson8). IPEH was considered a form of endothelial proliferation, and was usually located in the skin or subcutis of the neck and extremities. Although there is ongoing discussion as to the pathogenesis of IPEH, today most authors consider this lesion to be an unusual form of thrombus organization with exuberant proliferation5,6,18). The tumor-like growth may be induced by disturbed local hemodynamics that induce progression of thrombus formation and the subsequent development and growth of IPEH4).
IPEH can be divided into three different categories : the pure form that occurs within a dilated vascular space, which is most frequently located in the finger, head and neck or in the region between the elbows and hands; the mixed form that appears as a focal change in a hemangioma, vascular malformation, or pyogenic granuloma; and the undetermined form, belonging to neither of the first two categories, which has an extravascular origin6,12,14).
Extracranial IPEH usually presents as a slow-growing nodule that may be tender and somewhat painful. The age at manifestation varies widely, and there seems to be a slight female predominance in patients. At surgery, IPEH tends to bleed and often gives the impression of an organized hematoma. Complete resection seems to be curative. Deleterious courses of extracranial IPEH have not been reported.
Although IPEH most commonly occurs in skin and subcutaneous soft tissue, it has been reported in a variety of locations, including the liver, uterus, and gastrointestinal tract2,6). It appears, however, to have a predilection for the head and hands3). Intracalvalial IPEH is exceedingly rare.
Various skull lesions may radiologically mimic the appearance of IPEH. There were no specific radiological features of IPEH, where similar radiological findings can also be seen in other lesions such as eosinophilic granuloma, aneurysmal bone cyst, medullary fibrosarcoma, hemangioma, and metastatic tumors from the thyroid or kidney. Most skull tumors share certain MRI characteristics, such as hypointensity on T1-weighted images, hyperintensity on T2-weighted images, and some degree of contrast enhancement. Thus, the final diagnosis requires careful histological examination. Immunohistochemistry is essential for the establishment of the vascular nature of IPEH.
Histologically, the lesion consists of an intravascular proliferation of numerous papillae that are composed of a core of connective tissue and an endothelial surface. The endothelial cells may have a soft, round body. However, also having features of malignancy, such as nuclear pleomorphism, it often presents mitotic figures, necrosis, multiple layers of endothelial cells, and infiltrating growth into adjacent structures. The majority of these lesions are intimately associated with thrombotic material1,13,17). Immunohistochemically, IPEH reacts with factor VIII, CD31, CD34, corresponding to the endothelial cells being the proliferative component3,11,14,15). Epithelial membrane antigen, present in most meningioma, is absent in IPEH.
Vimentin has been previously reported to be positive in the stroma of these tumors as it was in our case. Taken together the histology and immunohistochemistry support the diagnosis of a benign tumor.
IPEH has known to act aggressively, in that it generally recurs when incompletely resected2,9). Therefore, the mainstay of therapy for intracranial IPEH has been, where possible, complete surgical resection. Complete resection was possible in the present case because of the small size and favorable location of the mass. Radiation therapy was not considered appropriate. The postoperative courses detected no metastasis or overt malignant behavior. Sometimes, complete surgical excision is not feasible. Adjuvant radiotherapy or chemotherapy for incompletely resected or multiple intracranial lesions has been associated with both lesion stabilization and short-term regression2,7,14). Given the small number of cases reported, it is difficult to draw any conclusions based on the efficacy of adjuvant therapy. We believe that total excision of the IPEH should be done before the mass reaches a size that might make complete removal impossible or cause other complications.
IPEH of the skull is a rare benign tumor located on the skull. Due to its rarity, IPEH is often misdiagnosed radiologically. Thus, final diagnosis requires a careful histological examination. These lesions may grow rapidly and reach an enormous size, and generally recur if incompletely resected. Therefore, we recommend that IPEH of the skull should be treated by complete resection with a wide margin to prevent a recurrence.
References
1. Albrecht S, Kahn HJ. Immunohistochemistry of intravascular papillary endothelial hyperplasia. J Cutan Pathol. 1990; 17:16–21. PMID: 2319035.

2. Avellino AM, Grant GA, Harris AB, Wallace SK, Shaw CM. Recurrent intracranial Masson's vegetant intravascular hemangioendothelioma. Case report and review of the literature. J Neurosurg. 1999; 91:308–312. PMID: 10433320.

3. Baylor JE, Antonelli PJ, Rojiani A, Mancuso AA. Facial palsy from Masson's vegetant intravascular hemangioendothelioma. Ear Nose Throat J. 1998; 77:408–410. 415–417. PMID: 9615522.

4. Cagli S, Oktar N, Dalbasti T, Işlekel S, Demirtaş E, Ozdamar N. Intravascular papillary endothelial hyperplasia of the central nervous system--four case reports. Neurol Med Chir (Tokyo). 2004; 44:302–310. PMID: 15253546.

5. Clearkin KP, Enzinger FM. Intravascular papillary endothelial hyperplasia. Arch Pathol Lab Med. 1976; 100:441–444. PMID: 947306.
6. Hashimoto H, Daimaru Y, Enjoji M. Intravascular papillary endothelial hyperplasia. A clinicopathologic study of 91 cases. Am J Dermatopathol. 1983; 5:539–546. PMID: 6666836.

7. Kristof RA, Van Roost D, Wolf HK, Schramm J. Intravascular papillary endothelial hyperplasia of the sellar region. Report of three cases and review of the literature. J Neurosurg. 1997; 86:558–563. PMID: 9046317.

8. Masson P. Hemangioendothelioma vegetant intravasculaire. Bull Soc Anat (Paris). 1923; 93:517–523.
9. Nagib MG, Sung JH, Seljeskog EL. Neurocutaneous Masson's vegetant intravascular hemangioendothelioma. Neurosurgery. 1982; 11:800–803. PMID: 7162575.

10. Ohshima T, Ogura K, Nakayashiki N, Tachibana E. Intravascular papillary endothelial hyperplasia at the superior orbital fissure : report of a case successfully treated with gamma knife radiosurgery. Surg Neurol. 2005; 64:266–269. discussion 269. PMID: 16099263.

11. Patt S, Kaden B, Stoltenburg-Didinger G. Intravascular papillary endothelial hyperplasia at the fissura orbitalis superior : a case report. Clin Neuropathol. 1992; 11:128–130. PMID: 1611724.
12. Pins MR, Rosenthal DI, Springfield DS, Rosenberg AE. Florid extravascular papillary endothelial hyperplasia (Masson's pseudoangiosarcoma) presenting as a soft-tissue sarcoma. Arch Pathol Lab Med. 1993; 117:259–263. PMID: 8442671.
13. Salyer WR, Salyer DC. Intravascular angiomatosis: development and distinction from angiosarcoma. Cancer. 1975; 36:995–1001. PMID: 1237350.

14. Sickler GK, Langford LA. Intracranial tumor-forming papillary endothelial hyperplasia--a case report. Clin Neuropathol. 1990; 9:125–128. PMID: 2364591.
15. Stoffman MR, Kim JH. Masson's vegetant hemangioendothelioma : case report and literature review. J Neurooncol. 2003; 61:17–22. PMID: 12587791.
16. Tosios K, Koutlas IG, Papanicolaou SI. Intravascular papillary endothelial hyperplasia of the oral soft tissues : report of 18 cases and review of the literature. J Oral Maxillofac Surg. 1994; 52:1263–1268. PMID: 7965329.

17. Wehbé MA, Otto NR. Intravascular papillary endothelial hyperplasia in the hand. J Hand Surg Am. 1986; 11:275–279. PMID: 3958464.

18. Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma : a vascular tumor often mistaken for a carcinoma. Cancer. 1982; 50:970–981. PMID: 7093931.

Fig. 1
Routine skull X-ray showed 1.2 cm sized punch-out lesion in the right frontal bone without bone expansion or sclerosis (A). Computerized tomography demonstrates a well-demarcated punch-out lesion with transdiploic exophytic soft tissue mass in frontal scalp. The lesion shows a central soft tissue component without brain invasion (B).
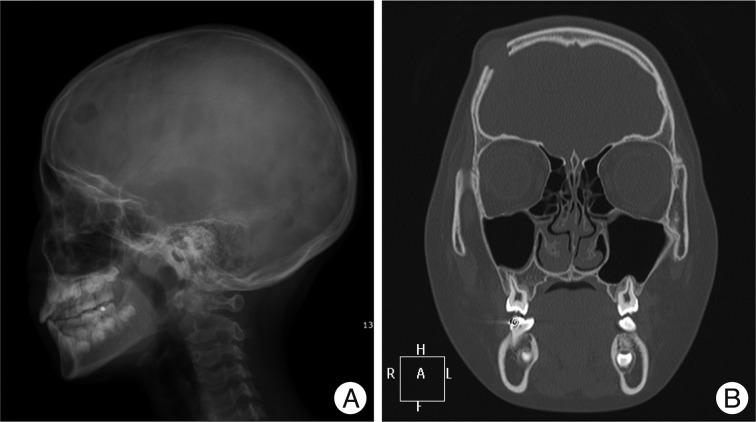
Fig. 2
Magnetic resonance (MR) image discloses the presence of a 1.3×1.2×1 cm nodular mass skull lesion. This mass lesion is hypointense on T1 (A) and inhomogenously hyperintense on T2-weighted MR image (B) and show inhomogenous enhancement of the soft tissue filling the punch-out lesion (C). Postoperative 1-month T1-weighted axial MR image showing no residual mass with frontal surgical defect (D).
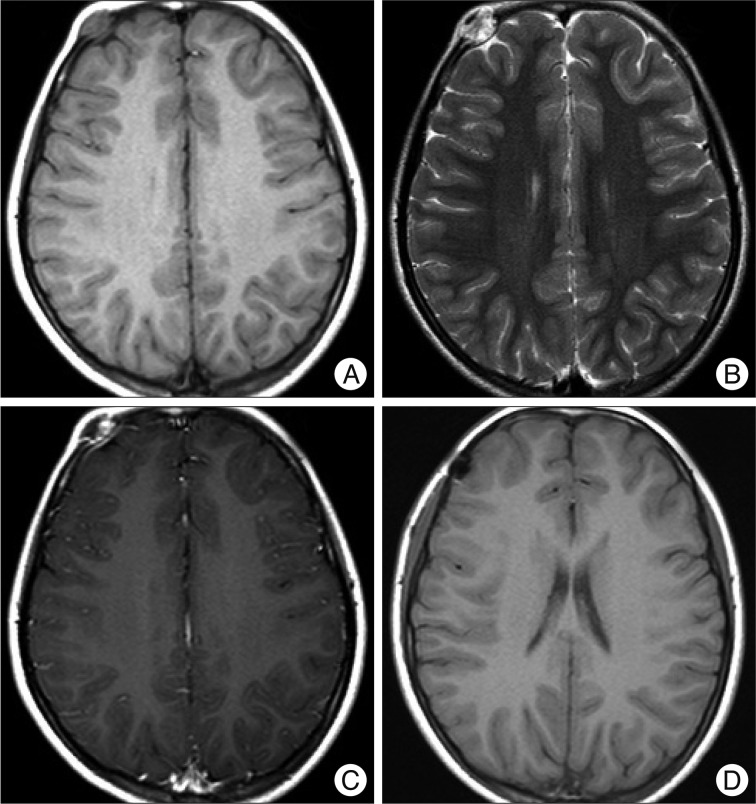
Fig. 3
Histologic sections reveals some vague papillary prolfierations of epithelioid cells with recent hemorrhage and fibrinous materials. The peripheral portions shows fibroblastic proferations with some metaplastic bone formation (H&E, ×40) (A). In high power view, there are vague papillary configurations of epitheloid endothelial cells with occasional distictive nucleoli and vesicular nuclei (H&E, ×40) (B). CD31 stain reveals positive reaction for tumor cells (C).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download