Abstract
Isolated tuberculosis of the coccyx is extremely rare. A 35-year-old man presented with a 3-month history of coccygeal and gluteal pain. Computed tomography and magnetic resonance imaging revealed osseous destruction and a large enhancing mass involving the coccyx with anterior and posterior extension. Pathologic examination of the surgical specimen revealed necrosis, chronic granulomatous inflammation, and multinucleated giant cells consistent with tuberculosis. This case highlights the importance of considering tuberculosis as a diagnosis even though unusual sites are involved.
A spinal infection with tuberculosis may be associated with a pulmonary infection, which occurs in less than 1% of patients with tuberculosis or, more rarely, the condition may be encountered in the absence of a pulmonary infection8). The most common locations for spinal tuberculosis, whether primary or secondary to a pulmonary tuberculosis, are the lower thoracic and lumbar spine. On the other hand, infection of the lumbosacral junction by tuberculosis is quite rare, and occurs in only 1 to 2% of all cases of spinal tuberculosis, moreover, isolated sacrococcygeal or coccygeal tuberculosis is much rarer10). As far as the authors' knowledge, there is only one reported isolated coccygeal tuberculosis5). As uncommon presentations can be a cause of delay and error in diagnosis and management, we report a unique case of isolated tuberculosis of the coccyx.
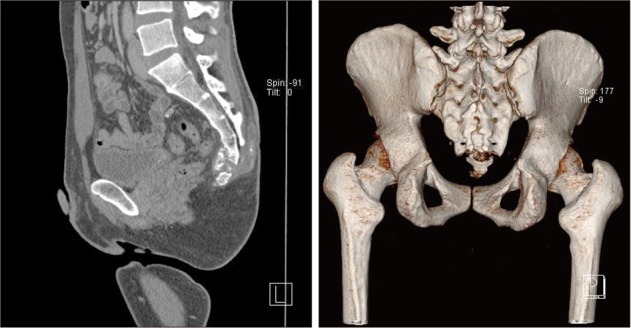
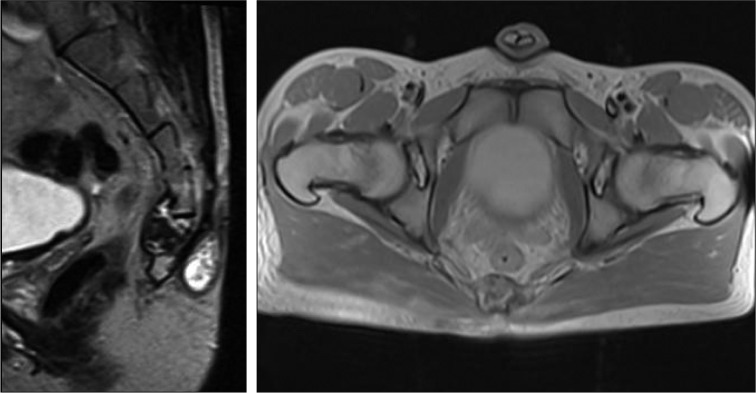
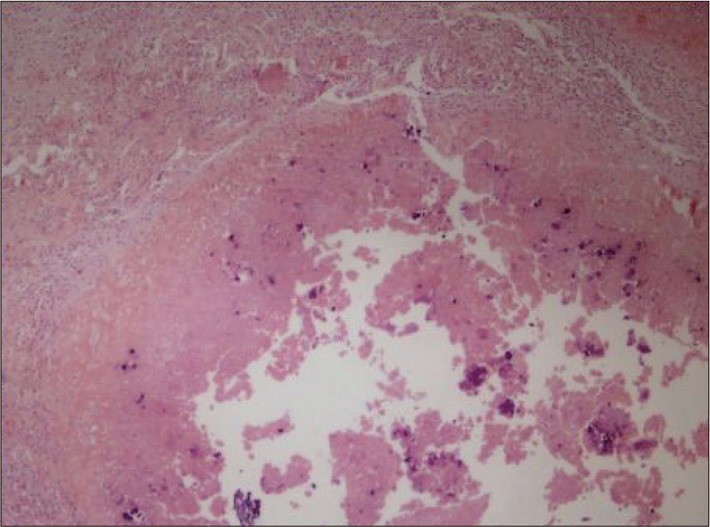
A 35-year-old man presented with a three month history of coccygeal and gluteal pain. Furthermore, the pain was associated with numbness in the same region and difficulty walking. The pain had been gradual in onset and was worse on sitting and walking. There was no bowel or bladder incontinence. He reported no recent weight loss, reduced appetite, cough, or night sweats, and his respiratory, cardiovascular, and abdominal system examinations were normal. No paresthesia or muscle weakness was evident in the legs, which he was able to straighten and raise his legs. However, mild perianal and perineal anesthesia were present. The Mantoux test and radiographs of the chest were negative, and hematological studies, including erythrocyte sedimentation rate and C-reactive protein were normal. A computed tomography (CT) scan of the lumbosacral spine revealed lytic destruction of the coccyx with sporadic calcification (Fig. 1). Magnetic resonance images (MRI) of the lumbosacral spine depicted a coccygeal mass involving the anterior and posterior extension (Fig. 2). Under a preliminary diagnosis of a primary bone tumor or metastasis, radionuclide bone scintigraphy (99m TC MDP) and positron emission tomography-CT were performed, but both failed to depict any lesion in addition to the lesion in the coccygeal area. A CT-guided biopsy of the sacral lesion was performed, and the patient was given anxiolytic and analgesic injection before and during the procedure. After infiltrating the skin and soft tissues with 2% lidocaine, a 14-gauge biopsy needle was advanced into the lesion and soft tissue and involved bone were aspirated. The solid material aspirated was dark brown in appearance and was forwarded for cytologic and microbiological examinations. The pathologic examination revealed caseating granulomas containing multinucleated giant cells (Fig. 3). Acid-fast bacilli cultures were positive for tuberculosis. The patient was given anti-tuberculosis treatment for 9 months based on four drugs (isoniazid, rifampin, pyrazimide, and ethambutol), which is the standard anti-tubercular regimen used at our institute. Patient made a rapid pain relief under this regimen and was asymptomatic at his last follow-up at 9 months.
Tuberculosis still remains one of the most pressing health problem in developing world, and tuberculosis of the spine occurs by hematogenous spread of infection from a pulmonary or extra-pulmonary site; pulmonary infection is detected in around 50% of cases of spinal tuberculosis8). Spinal tuberculosis is mainly due to hematogenous spread of mycobacteria from primary foci in the lung and or genitourinary tract. It is widely believed that the paravertebral venous plexus of Batson provides a primary pathway for the dissemination of tuberculous bacilli into the vertebral column, although it is also possible that lymphatic drainage of the pleura or kidney may involve the para-aortic lymph nodes and secondarily involve vertebrae1,4). After reaching a vertebra, mycobacteria infect the anterior portion of the body near the intervertebral disc, and may subsequently reach the cortex, destroy the intervertebral disc, and fragment the adjacent vertebral body. However, the reasons for the low incidence of lumbosacral or sacrococcygeal tuberculosis have not been exactly elucidated. The sacrum is an uncommon site for tuberculosis involving the spine. In a review of 107 patients of tuberculous spondylitis by Lifeso et al.6), no patient had lumbosacral and sacrococcygeal involvement. Clinical manifestations of sacral tuberculosis depend primarily on patient age. Young individuals tend to present with discharging sinuses and abscesses, whereas backache is a dominant clinical feature in adults. Because the sacral nerve roots are protected by bone, the incidence of neurological symptoms is relatively low7). Our patient with isolated involvement of the coccyx is probably the second described in the literature. Kumar et al.5) reported isolated coccygeal tuberculosis for the first time. But, in that case, there was a sinus overlying sacrococcygeal junction. MRI is the most sensitive diagnostic radiologic imaging, and the radiological spectrum of spinal tuberculosis has been well reported in the literature9,10). However, the sparsity of reports on sacral tuberculosis continues to be a source of diagnostic delays and errors, which is in part due to the lack of specific symptoms and the fact that pathologies in the sacral region can easily be missed if a non-sensitive imaging method is used because of the large number of overlying soft tissue shadows. Tuberculosis of the lumbosacral spine may also exhibit an uncommon presentation, where conventional simple radiographs do not reveal any obvious osseous lesion but MR images show the presence of an extradural granuloma or of peridural fibrosis compressing the spinal cord. Nevertheless, the enhancement of epidural soft tissue by gadolinium contrast-enhanced MRI suggests the possibility of an infection or tumor3). Plain radiographs are extremely insensitive, and do not detect vertebral involvement until at-least 50% of a vertebra is destroyed2). Similarly, bone scans are notably prone to miss this disease. In the described case, he presented with 3-month duration of coccygeal and gluteal pain. Considering the patient's clinical and radiological features, pyogenic osteomyelitis, tuberculosis, neoplasm such as chordoma or osteogenic sarcoma were included in the differential diagnosis. As tuberculosis lesions may be mistaken for other infectious diseases or neoplasms, fresh tissue should be obtained for culture and biopsy. Diagnosis by culture usually takes a longer time, whereas diagnosis can be established rapidly by histopathologic analysis of tissues obtained by percutaneous biopsy. In such cases, anti-tubercular treatment can be expected to achieve complete cure. It is imperative that such presentations of tuberculosis should be borne in mind because this ensures that correct diagnosis can be made promptly and appropriately.
References
1. Ahmadi J, Bajaj A, Destian S, Segall HD, Zee CS. Spinal tuberculosis: atypical observations at MR imaging. Radiology. 1993; 189:489–493. PMID: 8210378.

2. Desai SS. Early diagnosis of spinal tuberculosis by MRI. J Bone Joint Surg Br. 1994; 76:863–869. PMID: 7983108.

3. Kim DW, Choi HJ, Kim HD, Song YJ. Atypical presentation of spinal tuberculosis misdiagnosed as metastatic spine tumor. J Korean Neurosurg Soc. 2006; 39:451–454.
4. Kim NH, Lee HM, Suh JS. Magnetic resonance imaging for the diagnosis of tuberculous spondylitis. Spine (Phila Pa 1976). 1994; 19:2451–2455. PMID: 7846600.

5. Kumar A, Varshney MK, Trikha V, Khan SA. Isolated tuberculosis of the coccyx. J Bone Joint Surg Br. 2006; 88:1388–1389. PMID: 17012433.

6. Lifeso RM, Weaver P, Harder EH. Tuberculous spondylitis in adults. J Bone Joint Surg Am. 1985; 67:1405–1413. PMID: 4077912.

7. Pun WK, Chow SP, Luk KD, Cheng CL, Hsu LC, Leong JC. Tuberculosis of the lumbosacral junction. Long-term follow-up of 26 cases. J Bone Joint Surg Br. 1990; 72:675–678. PMID: 2143192.

8. Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M. Modern management of spinal tuberculosis. Neurosurgery. 1995; 36:87–97. discussion 97-98. PMID: 7708173.

9. Weaver P, Lifeso RM. The radiological diagnosis of tuberculosis of the adult spine. Skeletal Radiol. 1984; 12:178–186. PMID: 6494935.

10. Wellons JC, Zomorodi AR, Villaviciencio AT, Woods CW, Lawson WT, Eastwood JD. Sacral tuberculosis: a case report and review of the literature. Surg Neurol. 2004; 61:136–139. discussion 139-141. PMID: 14751619.

Fig. 1
Computed tomography (CT) scans of the patient. CT scans of the patient reveal a lytic lesion involving coccyx.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download