Abstract
Objective
The objective of this study was to investigate the morphologic characteristics between the vertebral body and the regions of the cervical and thoracic spinal cords where each rootlets branch out.
Methods
Sixteen adult cadavers (12 males and 4 females) with a mean age of 57.9 (range of 33 to 70 years old) were used in this study. The anatomical relationship between the exit points of the nerve roots from the posterior root entry zone at each spinal cord segment and their corresponding relevant vertebral bodies were also analyzed.
Results
Vertical span of the posterior root entry zone between the upper and lower rootlet originating from each spinal segment ranged from 10-12 mm. The lengths of the rootlets from their point of origin at the spinal cord to their entrance into the intervertebral foramen were 5.9 mm at the third cervical nerve root and increased to 14.5 mm at the eighth cervical nerve root. At the lower segments of the nerve roots (T3 to T12), the posterior root entry zone of the relevant nerve roots had a corresponding anatomical relationship with the vertebral body that is two segments above. The posterior root entry zones of the sixth (94%) and seventh (81%) cervical nerve roots were located at a vertebral body a segment above from relevant
segment.
Two pairs of spinal nerve roots which allow motor and sensory neurons to exit and enter the spinal cord, projects from each segment of the spinal cord. The motor nervous system is located in the ventral or front side of the spinal cord and the sensory nervous system is located at the dorsal or back side of the spinal cord. Depending on the vertical location of the intervertebral foramen through which the nerves exit, the nerve root is named as cervical, thoracic, lumbar, or sacral nerve root. However, the most caudal part of the spinal cord only reaches the point between the first and the second lumbar vertebrae since the spinal vertebrae, which are bony structures, grow more rapidly than the spinal cord and nerverous system, during growth and development after birth. It is well known that the cervical and thoracic nervous segments of the spinal cord are located from one to two vertebral body segments above their corresponding relevant vertebrae5). However, some studies have only researched and mentioned those for the low cervical region5,6,10). Also, few studies have researched the anatomical relationship between the cervico-thoracic cord segments or the relevant nerve roots and the surrounding vertebral bodies. Accurate knowledge of these relationships will improve our pathological understanding of surgical complications and neurological disorders due to traumatic and other causes of spinal cord injuries.
The objective of this study was to investigate the anatomical relationship between the vertebral bodies and the nerve rootlets arrising from the cervical and thoracic spinal cord regions. The morphologic characteristics of the intradural rootlets located between their point of origin from the spinal cord and the intervertebral foramen were also evaluated. This study will provide anatomical details in order to understand spinal cord disease causation for accurate diagnosis when pathologic lesions occur in the spinal cord or vertebral body.
Sixteen adult cadavers (12 males and 4 females) with a mean age of 57.9 (range 33-70) were used in this study. The cadavers were fixed in a mixture of formalin, phenol, alcohol and glycerin. Posterior muscles of the cervical, thoracic and lumbar spine were removed while in the prone position. Total laminectomy was then performed to expose the dura of the spinal cord as well as the areas around where the nerve roots passed through the intervertebral foramen. The locations of the nerve roots were verified after the locations of each disc in the ventral portion of the cervical and thoracic regions were identified. The location of each corresponding vertebral body and disc in the dorsal portion were confirmed as shown in Fig. 1. The dorsal portion of the dura, which surrounds the spinal cord and nerve roots, was incised to expose the spinal cords and rootlets. A total of 32 specimens (from both the right and left sides of 16 cadavers) were available to investigate the following : 1) the number of rootlets in a nerve root, 2) the vertical lengths of the posterior root entry zones where the rootlets have originated from the spinal cord; 3) the length of the nerve root from the spinal cord to its entrance into the intervertebral foramen; 4) anatomical relationship between the exit point of the nerve root from the posterior root entry zone at each spinal segments and the relevant vertebral bodies.
Measurements were conducted using a standard meter and goniometer. Measured data were compared and analyzed first, according to laterality and then according to cervical or thoracic spine region. The SPSS software (Version 17.0, Chicago, IL, USA) was used to perform a t-test with the threshold p-value set at 0.05.
The exposed spinal cord had a cylindrical structure which was slightly flattened dorso-ventrally. The spinal cord had a structure which anterior-posterior length was longer than left-right length. The level of the relevant segments of the spinal cord, where the roots have originated, could not be differentiated and identified by just looking at the spinal cord but were identified by tracing the course of the nerve roots in a retrograde fashion. The relevant nervous segments were identified at the posterior root entry zone. Rootlets ran in an inferolateral direction and passed through the intervertebral foramen. The rootlets in the thoracic region formed a more acute angle and shaped overally thinner than in the cervical region. The rootlets consisted of a spinal cord segment with ovally inflated right before posterior root entry zone (Fig. 1).
The first cervical nerve root was found between the occipital bone and the first cervical vertebra. Cervical nerve roots from the second to the seventh were found at each corresponding cervical vertebrae. The eight cervical nerve root was found entering the intervertebral foramen located between the seventh cervical vertebra and the first thoracic vertebra. The thoracic nerve roots were found located at each corresponding thoracic vertebrae. The width of the fifth, sixth, and seventh cervical nerve roots at their origins was bigger than the rest. The rootlets exiting from the spinal cord were arranged in a line along the posterolateral furrow of the spinal cord. It was found that the rootlets from lower cervical spinal cord were located more medially. Intersegmental rootlets from the fifth-sixth, sixth-seventh, and seventh-eighth cervical nerve roots were anastomosed before entering the intervertebral foramen as illustrated in Fig. 2.
The average number of rootlets that composed each nerve root was seven in the cervical region, five in the upper thoracic region, and three in the lower thoracic region, as shown in Table 1.
In the cervical spine, the maximum number of rootlets was 7.4 and was in the sixth cervical nerve root. The third nerve root had 7.3 rootlets, the fourth nerve root had 7.0 rootlets, the fifth nerve root had 6.9 rootlets, the seventh nerve root had 6.8 rootlets, and the eighth nerve root had 6.4 rootlets. The number of rootlets decreased as the nerve root coursed inferiorly except for the sixth nerve root which had the most number of rootlets Fig. 2. In the thoracic spine, the number of rootlets decreased as it went inferiorly. The first thoracic nerve root had 5.5 rootlets, the second nerve root had 5.1 rootlets, the third nerve root had 4.5 rootlets, the fourth, fifth, and sixth nerve root had 3-4 rootlets, and the seventh-twelfth nerve root had 2-3 rootlets. There was no statistical difference between right and left side nerve roots.
Vertical length of the posterior root entry zone, which is the length between the uppermost rootlet and the lowermost rootlet originating from each cord segment, was 10-12 mm on average as shown in Table 2 and Fig. 3. In the cervical spine, the sixth nerve root entry zone was the longest at 12.7 mm. The fifth nerve root entry zone was 12.0 mm long, the fourth was 11.7 mm long, and the third was 11.1 mm long. It was found that the vertical length of the posterior root entry zone increased as one went down the cervical spinal cord segments until the sixth nerve root. The seventh nerve root was 11.2 mm long which was shorter than that of the sixth and eighth nerve roots (12.7 and 12.6 mm, respectively). Generally, the length of the nerve root entry zone tended to increase along the inferior direction.
In the thoracic spine, the second nerve root entry zone had the maximum length at 12.7 mm and the seventh was the shortest at 8.8 mm. While the sixth nerve root entry zone was relatively long at 11 mm, the length tended to increase towards the superior direction above the fifth and following the inferior direction below the seventh. There were statistical differences in the vertical length of the posterior root entry zones at the eighth cervical nerve root, and the third and eighth thoracic nerve roots between the right and left sides. The eighth cervical nerve root entry zone on the left side was significantly longer than the right side. Right nerve root entry zones of the third and eighth thoracic spine was statistically longer than the left.
The length of the rootlets from the spinal cord to the entrance of the intervertebral foramen tended to increase as we went down the spinal segments at all cervical and thoracic spinal levels as shown in Fig. 3. Due to the difference between the neural structures' and bony structures' rate and duration of growth on the basis of foramen magnum, there were relatively short length in the cervical spine and long length in the thoracic spine.
In the cervical spine, the third nerve root was 5.9 mm long and the eighth nerve root was 14.5 mm long. Table 3 shows that the length of the nerve roots increased by 3 mm compared to the nerve root immediately superior to it from the sixth, seventh, and eighth cervical levels. Thereafter, the nerve roots progressively lengthened as the spinal segments progressed caudally along the entire vertebral column including the thoracic region. The twelvth thoracic nerve root was approximately 52 mm long. In the thoracic spine, the inferior neural segment nerve root was generally 3 mm longer than its immediate superior counterpart. The seventh thoracic nerve root was 7 mm longer then the sixth. The nerve rootlet was significantly longer on the right side at the level of the third cervical spine. The nerve rootlets were were shorter on the right side at the eighth cervical, second thoracic, and sixth thoracic spinal levels.
The posterior root entry zones for the cervical nerve roots C1 to C5 were located at a level one vertebral body segment above their corresponding relevant vertebral bodies. At the lower segments of the spinal cord (T3 to T12), the posterior root entry zones for the relevant nerve roots were located at a level two vertebral body segments above their corresponding relevant vertebral bodies, as shown in Table 4. For example, the posterior root entry zone for the third cervical nerve was located at the level of the second cervical vertebral body and the posterior root entry zone for the third thoracic nerve was at the level of the first thoracic vertebral body. Both the right and left sides of all sixteen cadavers showed the same results.
The location of the sixth, seventh and eighth cervical, and the first and second thoracic nerve root entry zones showed some variation among different individuals. However, the posterior root entry zones of the sixth (94%) and seventh (81%) cervical nerve roots were located at a level one vertebral body segment above their corresponding relevant vertebral bodies. Unlike other cervical vertebral bodies that corresponded with one above segment vertebral body, the eighth cervical nerve root entry zone (88%) was at the level of the sixth cervical vertebra. The location of the posterior root entry zone for the first thoracic nerve root (100%) was identical with the seventh cervical vertebra and the location of the posterior root entry zone for the second thoracic nerve root was between the seventh cervical and the first thoracic vertebra in 12 cadavers (75%). The location of the posterior root entry zone for the second thoracic nerve root was at the level of the seventh cervical vertebra in 2 cadavers and at the first thoracic vertebra in another 2 cadavers. Table 4 shows these investigated anatomical relationships.
The spinal cord starts from the foramen magnum and ends at a level between the twelvth thoracic vertebra and the first lumbar vertebra. Segments of the spinal cord aren't generally called depending on relevant vertebral bodies. It was known that the spinal cord neural segments were located at one vertebral body level above their corresponding relevant vertebrae in the cervical region and at two vertebral body levels above in the thoracic region5). Nevertheless, it was difficult to find anatomical studies on the relationship between vertebral bodies and the neural segments of the spinal cord from which the relavent rootlets originated. While such morphologic knowledge helps in the understanding of spinal cord trauma, myelopathy due to pathological lesions of the spinal cord, and radicular pains; it was extremely difficult to standardize the anatomy of the spinal cord or nerve roots because of the individual variations in size and shape4,8). Considering the fundermental data presented above, safe and sufficient decompression can be achieved when surgical treaments are performed on the thoracic or cervical vertebrae and the spinal cord. It would also be helpful in determinig the cause of unexpencted disorders or surgical complications.
The normal relationships between the segments of the cervical or thoracic spinal cord and the intervetebral discs have already been mentioned in several anatomical textbooks. However, these were not clearly defined and classifed. There were even several different criteria used for the such relationships. Each segment of the spinal cord was defined and demarcated as either; 1) the segment in between the most superior rootlet of a nerve root to the most superior rootlet of the adjacent nerve root, 2) the middle portion of two adjacent nerve roots, or 3) the part in which a pair of nerve roots were attached to. This study used the first definition. Kubo6) reported that, with some exceptions, the seventh cervical nerve root generally started at the level of the fifth and sixth cervical intervertebral disc (C5-C6) and the eighth cervical nerve root originated at the level of the sixth and seventh cervical intervertebral disc (C6-C7) in eighty percent of subjects. Kim and Shin5) described that the seventh cervical nerve root was mostly located at the level of the fifth and sixth cervical intervertebral disc (C5-C6), the fifth cervical nerve root was at the level of the fourth cervical vertebra (C4), and the sixth cervical nerve root was at the level of the fifth cervical vertebra (C5). Tanaka et al.10) reported that the starting point of the fifth cervical nerve root was at the level of the fourth cervical vertebra (C4), the sixth cervical nerve root was at the level between the fourth and fifth cervical vertebrae, and the seventh cervical nerve root was at the level between the fifth and sixth cervical vertebrae. While there were some differences between the reported studies, the results led to very similar conclusions.
Based on the previous studies, a formula for the relationship between the neural segments of the spinal cord and vertebral bodies can be derived. The spinal cord neural segements of the posterior root entry zones for the cervical nerve roots down to the first thoracic nerve root were located at the level one vertebral body segment immediately superior to their corresponding relevent vertebrae of exit. Seventy-five percent (75%) of the specimens examined showed that the spinal cord neural segment for the posterior root entry zone of the second thoracic nerve root was located one and a half vertebral body level above its corresponding relevent vertebrae of exit, which is between the seventh cervical vertebra and the first thoracic vertebra. Otherwise, it was located at the level of the seventh cervical vertebra or the first thoracic vertebra. Caudad of the third thoracic nerve root, the locations of the spinal cord neural segments for the posterior root entry zone were at the level 2 vertebral segments superior to their corresponding relevant vertebra of exit. Following the above rule, the eighth cervical spinal cord neural segment would have its posterior root entry zone located at the level of the seventh cervical vertebra. However, our cadeveric studies showed that it was located at the level of the sixth cervical vertebra. This may be due to the non-existence of an eighth cervical vertebra and the relative thickening of the spinal cord at the fourth, fifth, and sixth cervical vertebral levels. It was generally known and accepted that the cervical spinal cord neural segments were located at a level one vertebral segment above and the neural segments in the thoracic spinal cord were located at a level two vertebral segments above their corresponding relevant vertebra. This study showed that the generally accepted "one vertebral segment above" or "two vertebral segments above" rule is actually demarcated at the second thoracic nerve root. This result may be clinically interpreted as it could efffect the next inferior nerve root when C3-C4 intervertebral disc was posteriorly bulged and two nerval segments were related. In case where the thoracic spine is involved, three spinal cord neural segments could be affected.
This study did not look into the effect of aging on the morphometric relationship between the cervico-thoracic cord segments and the vertebral body. Payne and Spillane9) reported that the nerve roots were pointing in the inferior direction due to the different growth rates of the spinal cord and vertebral bodies. They also mentioned that the height of both intervertebral discs and vertebral bodies decreased with age. Considering small amount of the decrease and effects on overall height of whole spine, such decline of the height made the spinal cord lower comparing with vertebral bodies and the angle of the nerve roots could be reduced while Hwang et al.3) decribed that the angle was 60-68 degree. Spinal nerve roots are consisted of anterior horn beginning from the spinal cord and posterior horn going to the spinal cord. Kubo et al.6) discussed that the anterior root exit zone may not be anatomically defined but it could be defined as an oval shape from the most superior anterior rootlet to the most inferior anterior rootlet. Also, they studied anatomical difference of posterior root exit zone that posterior rootlet disposed in lines along the posterolateral furrow. Generally, the posterior rootlets were thicker than the anterior rootlets in the cervical spine. The mean vertical length of the anterior root exit zone was 10-15 mm and an anterior nerve root consisted of 17-25 rootlets. The vertical length of the posterior root exit zone was 6-14 mm and the number of rootlets was 7-12. It has been mentioned that there was a difference in the number of rootlets between the anterior and the posterior nerve roots even though they were on the same spinal cord neural segment. Clark2) described variations in the number of rootlets composing the posterior root exit zone but it was mostly 7-12.
This study was limited to the investigation of the posterior side of the spinal cord only. It showed similar results that vertical length of posterior root exit zone was 10-12 mm. The numer of rootlets (7) found in the current investigation was different from the referred studies. The reason for this difference may be because a microscope was used in the previous studies and this study relied on macrography. It is important, from a clinical standpoint, to know that the rootlets of the posterior root exit zone progressively shifted more medially as one follows the spinal cord inferiorly from the cervical spine region to the thoracic spine region. It was known that lesions on the spinal cord cause spinal cord diseases and leisons outside the spinal cord that press the nerve root, cause radicular pain. Even though this study was limited to the posterior spinal cord, the study was able to show that both myelopathy and radicular pain can result from a lesion on the spinal cord. Moreover, Kubo et al.6) and Tanaka et al.10) mentioned that on the anterior side of the spinal cord, the left and right anterior root exit zones progressivley moved medially as it went caudally and their distance was 1-3 mm. This meant that a medially herniated intervertebral disc can cause nerve root compression and lead to radicular pain even without intervertebral foraminal stenosis.
This study is in agreement with the results of previous research regarding the vertical length of the posterior root exit zone being shorter and the number of rootlets being less in the thoracic spinal cord than in the cervical spinal cord. The reason for a greater number of cervical rootlets than the number of thoracic rootlets may be related to the functions required of the nerves. Since the upper limbs need to perform much more functions than others, it is understandable that the upper spinal cord has to have more rootlets. Also, it can be related to width of the spinal cord that Chang et al.1) reported that the spinal cord was widest at the level of the sixth-seventh cervical spine.
It was observed that the rootlets were anastomosed before entering the intervertebral foramen. Most rootlets were anastomosed between the 5th and 6th nerve roots, between the 6th and 7th nerve roots, and between the 7th and 8th nerve roots. However, there were big individual differences. This result was the same with previous studies6,7,10). Since this anastomosis may cause confusion regarding the lesion's location, pre-operative neurological tests should be performed and it should be clearly confirmed through radiological images.
Rootlets originating from the spinal cord that forms the spinal roots were arranged in single lines along the posterolateral furrow of the spinal cord. The more caudal cervical rootlets emerged from the spinal cord closer to the midline. This finding shows that pathological lesion in the central cord may cause both myelopathy and radicular pain. Since the growth rate of the spinal nerve root and the vertebral body are different, the spinal cord segments between the third cervical nerve root and the first thoracic nerve root were located one vertebral body level above their corresponding relevant vertebral bodies.
Because confusion over the anatomical structures can easily occur due to the limited surgical view associated with anterior cervical surgery, the measurement results taken from the subaxial cervical vertebrae in this study will contribute to a successful surgery.
References
1. Chang JC, Park HK, Bae HG, Cho SJ, Choi SK, Byun PJ. Morphometric measurement of the anatomical landmark in anterior cervical microforaminotomy. J Korean Neurosurg Soc. 2006; 39:340–346.
2. Clark CR. Anatomy of the cervical spine : the Cervical Spine. 2005. ed 4. Philadelphia: Lippincott Williams & Wilkins;p. 13–15.
3. Hwang JC, Bae HG, Cho SW, Cho SJ, Park HK, Chang JC. Morphometric study of the nerve roots around the lateral mass for posterior foraminotomy. J Korean Neurosurg Soc. 2010; 47:358–364. PMID: 20539795.

4. Kameyama T, Hashizume Y, Ando T, Takahashi A. Morphometry of the normal cadaveric cervical spinal cord. Spine (Phila Pa 1976). 1994; 19:2077–2081. PMID: 7825049.

5. Kim P, Shin WH. A guidebook for the future experts in the cervical spine surgery from neurological evaluation to microsurgical techniques. 2007. Seoul: ML Communication;p. 13.
6. Kubo Y, Waga S, Kojima T, Matsubara T, Kuga Y, Nakagawa Y. Microsurgical anatomy of the lower cervical spine and cord. Neurosurgery. 1994; 34:895–890. discussion 901-902. PMID: 8052389.

7. Marzo JM, Simmons EH, Kallen F. Intradural connections between adjacent cervical spinal roots. Spine (Phila Pa 1976). 1987; 12:964–968. PMID: 3441822.

8. Okada Y, Ikata T, Katoh S, Yamada H. Morphologic analysis of the cervical spinal cord, dural tube, and spinal canal by magnetic resonance imaging in normal adults and patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976). 1994; 19:2331–2335. PMID: 7846579.

9. Payne EE, Spillane JD. The cervical spine; an anatomico-pathological study of 70 specimens (using a special technique) with particular reference to the problem of cervical spondylosis. Brain. 1957; 80:571–596. PMID: 13499761.

10. Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine (Phila Pa 1976). 2000; 25:286–291. PMID: 10703098.

Fig. 1
Photograph of a cadaver specimen (P-A view) showing the contents of the spinal canal after total laminectomy and durotomy. The intervertebral disc spaces of the cervical spine are marked with pink pins and those of the thoracic spine are marked with green pins. The yellow arrow head indicates the C7-T1 intervertebral disc space.
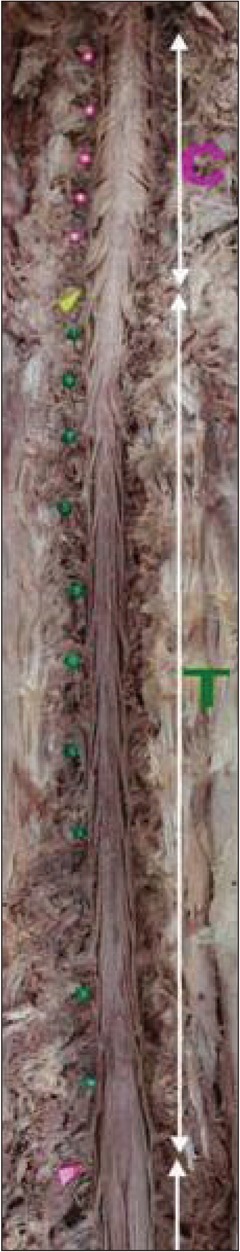
Fig. 2
Photograph showing the rootlet (black arrow head) entering each segment of the cervical (A) and thoracic (B) spinal cord. Red arrow head indicates the intersegmental anastomosis between the spinal rootlets.
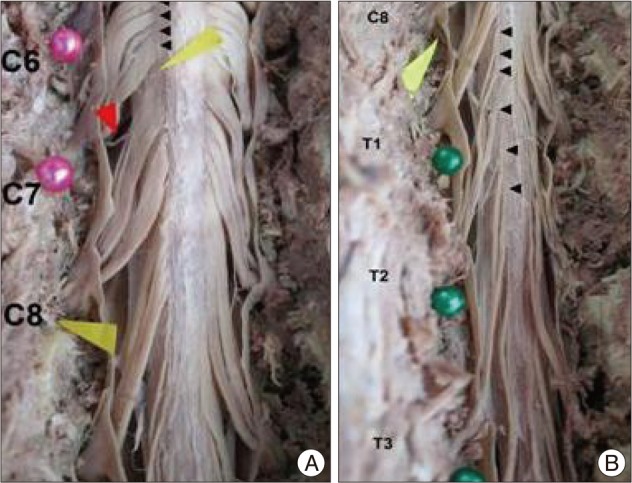
Fig. 3
Photograph showing the distance of the cervical (A) and thoracic (B) spines. Red line indicates the distance between the uppermost rootlet and the lowermost rootlet in each segment. Blue line is the length of the rootlet between the spinal root entry zone to the intervertebral foramen. The distance from the midline to the posterior root entry zones is decreased in the lower cervical spine.
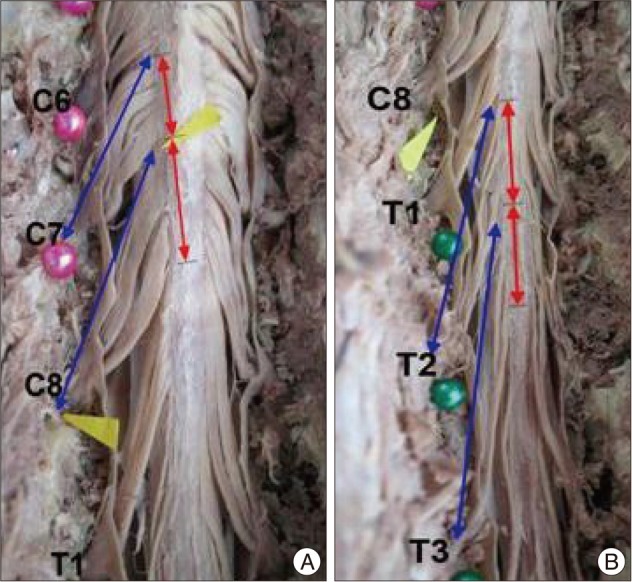
Table 1
The mean number of rootlets composing each spinal nerve root in 32 specimens from 16 cadavers
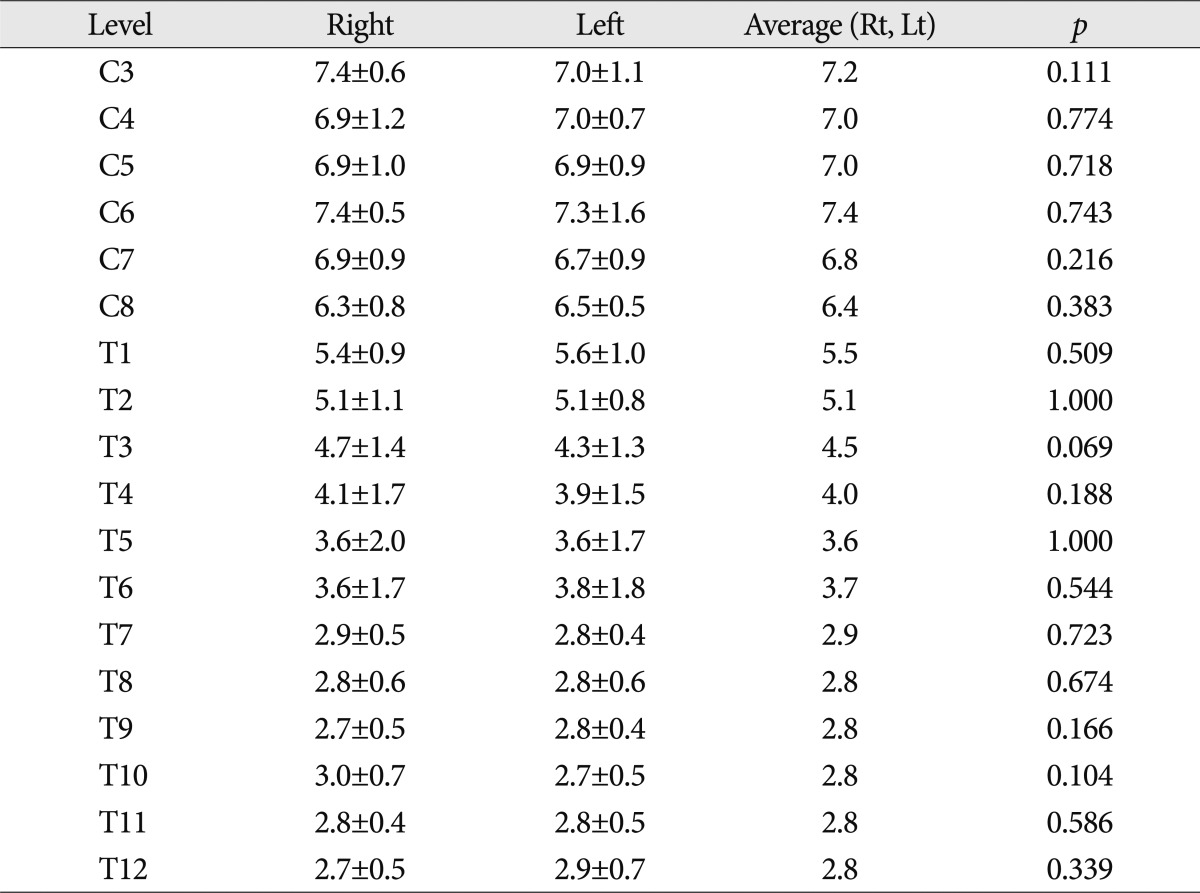
Table 2
The mean distance between the uppermost and the lowermost rootlet of each spinal nerve root at the level of the spinal cord in 32 specimens from 16 cadavers
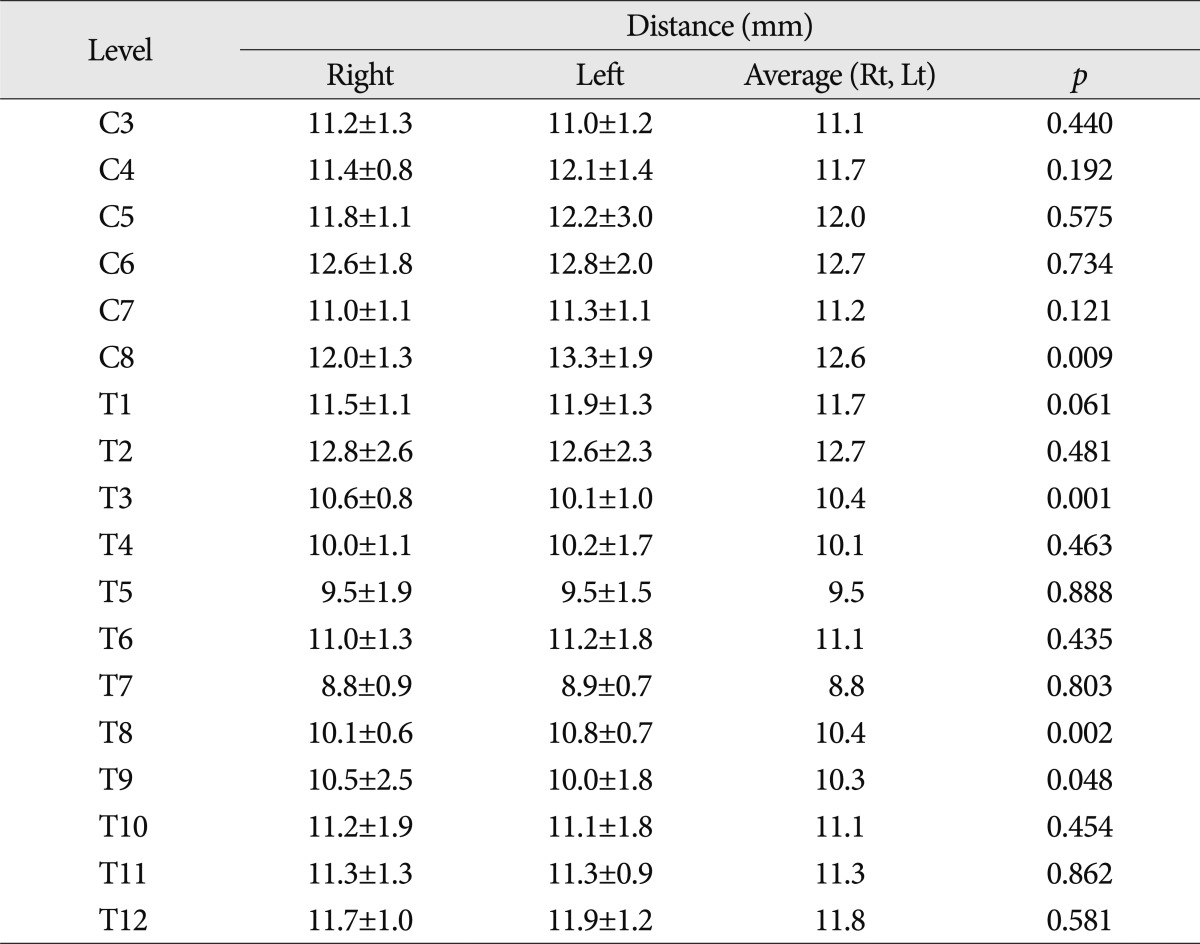
Table 3
The mean length of the spinal nerve root measured from the spinal root entry zones to the intervertebral foramen at each level in 32 specimens from 16 cadavers
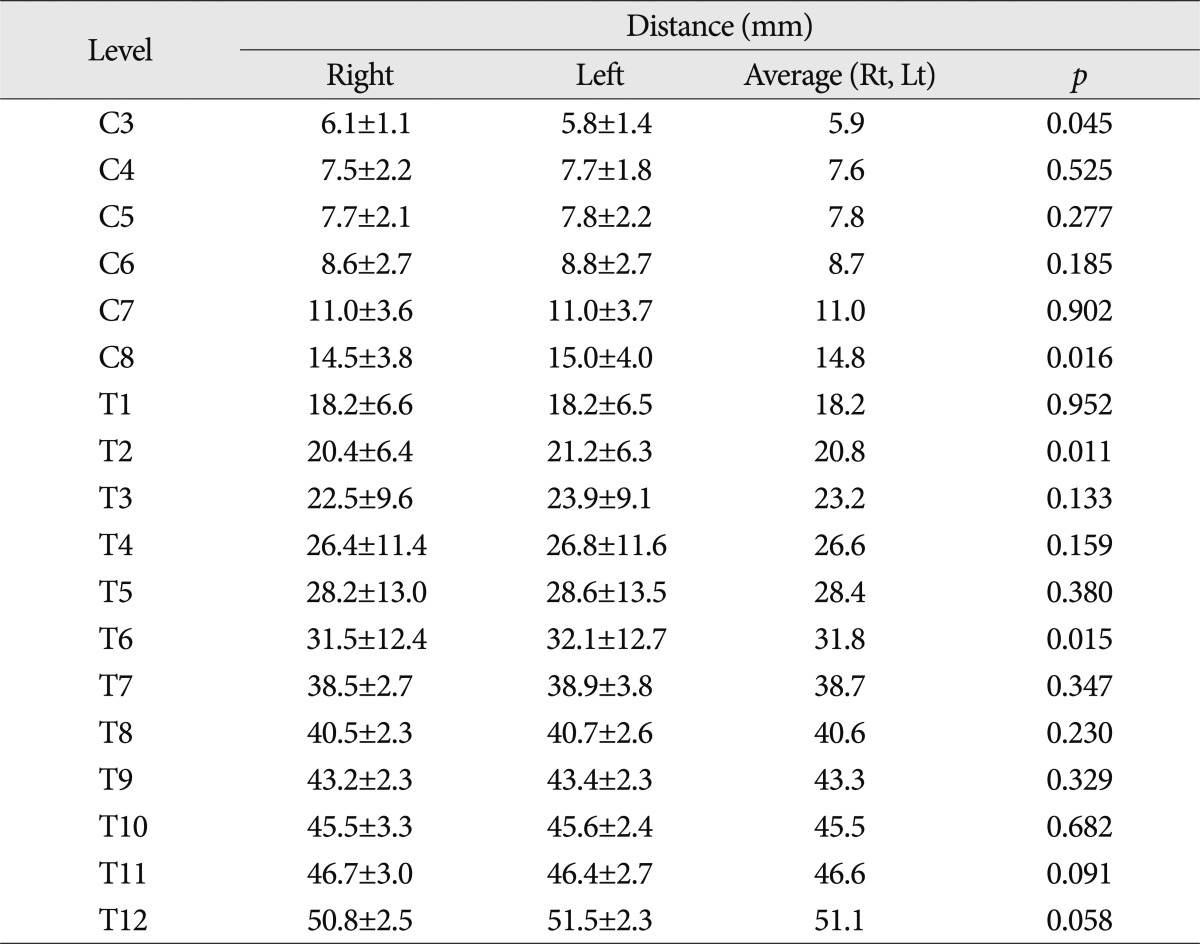
Table 4
The vertebral body level corresponding to the level of the spinal cord segment from where each spinal nerve root exited in 32 specimens from 16 cadavers
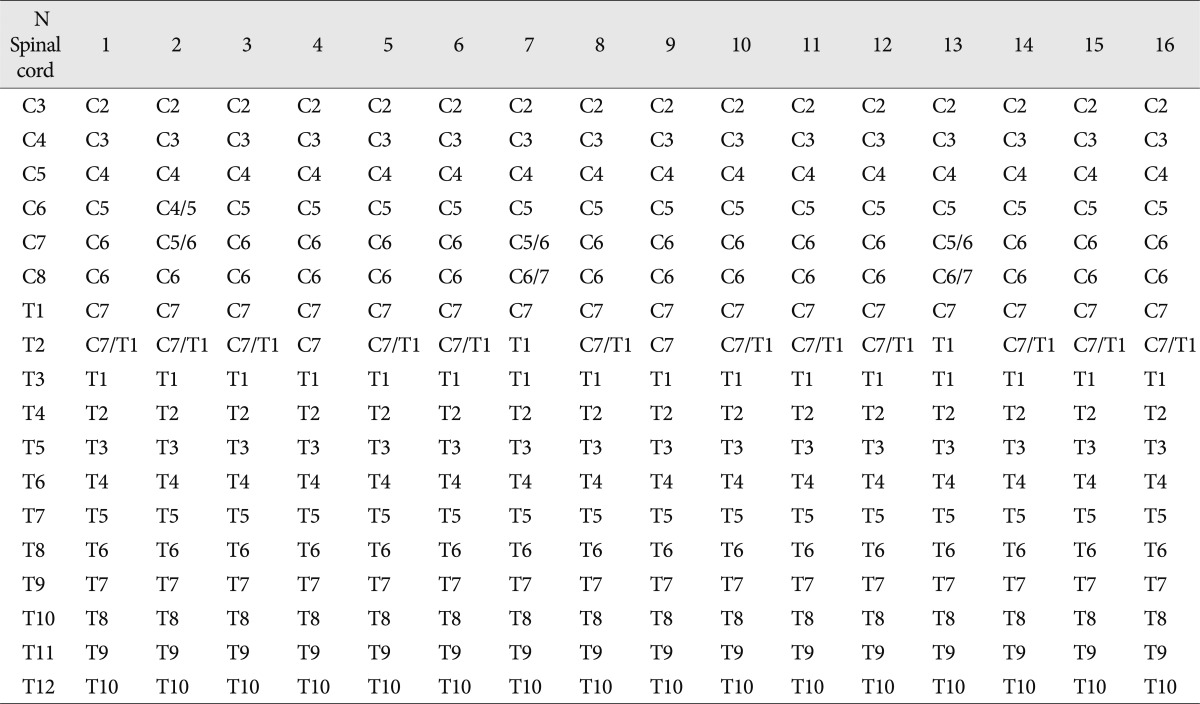
Table 5
Summary of anatomical relationship between the vertebral body level and the level of the spinal cord segment from where each spinal nerve root exited in 32 specimens from 16 cadavers
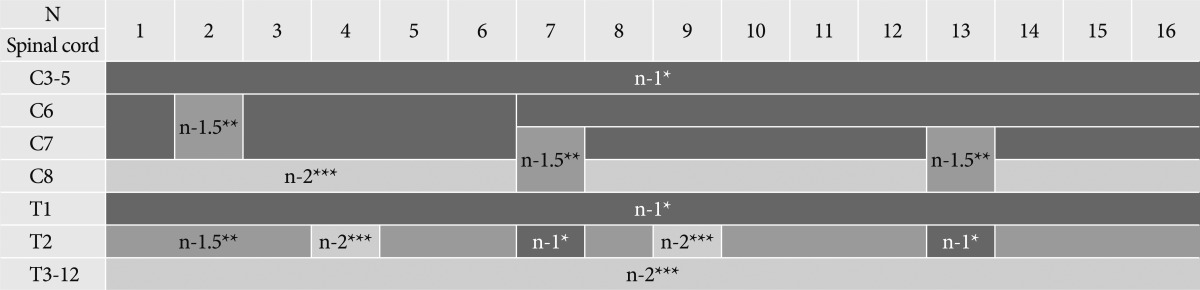
N : numbers of cadavers, n : level of root. *n-1 : spinal cord segment is located one vertebral body level higher than its corresponding intervertebral foamen through which the nerve root passed. **n-1.5 : spinal cord segment is located one and a half vertebral body level higher than its corresponding intervertebral foamen through which the nerve root passed. ***n-2 : spinal cord segment is located two vertebral body levels higher than its corresponding intervertebral foamen through which the nerve root passed




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download