Abstract
Objective
Chronic subdural hematoma (CSDH) is a typical disease that is encountered frequently in neurosurgical practice. The medications which could cause coagulopathies were known as one of the risk factors of CSDH, such as anticoagulants (ACs) and antiplatelet agents (APs). Recently, the number of patients who are treated with ACs/APs is increasing, especially in the elderly population. With widespread use of these drugs, there is a need to study the changes in risk factors of CSDH patients.
Methods
We retrospectively reviewed 290 CSDH patients who underwent surgery at our institute between 1996 and 2010. We classified them into three groups according to the time of presentation (Group A : the remote period group, 1996-2000, Group B : the past period group, 2001-2005, and Group C : the recent period group, 2006-2010). Also, we performed the comparative analysis of independent risk factors between three groups.
Results
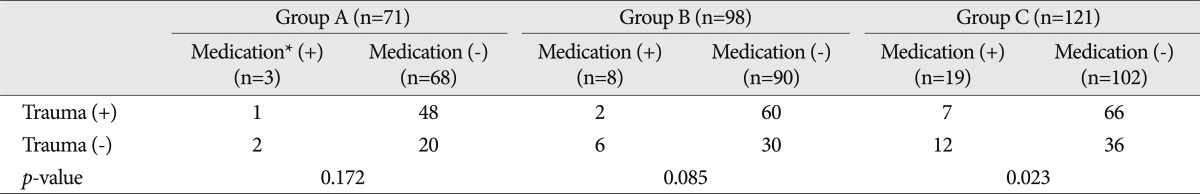
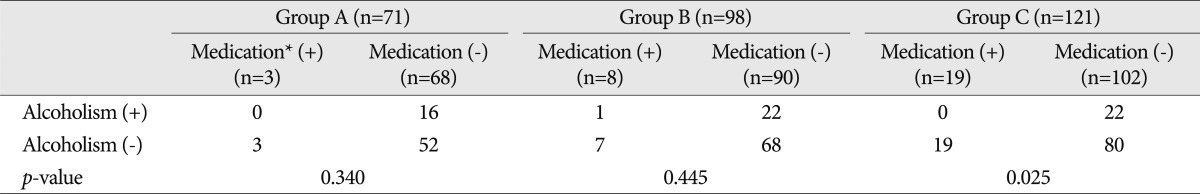
Among the 290 patients, Group A included 71 patients (24.5%), Group B included 98 patients (33.8%) and Group C included 121 patients (41.7%). Three patients (4.2%) in Group A had a history of receiving ACs/APs, 8 patients (8.2%) in Group B, and 19 patients (15.7%) in Group C. Other factors such as head trauma, alcoholism, epilepsy, previous neurosurgery and underlying disease having bleeding tendency were also evaluated. In ACs/APs related cause of CSDH in Group C, significantly less proportion of the patients are associated with trauma or alcohol compared to the non-medication group.
Chronic subdural hematoma (CSDH) is a common disease in neurosurgical practice, especially in elderly patients1,6). The current understanding is that CSDH is mostly the results of direct or indirect head trauma. Other factors such as alcoholism, liver cirrhosis, chronic renal failure and hematologic disease are also well known as causes of CSDH. And anticoagulants (ACs) and antiplatelet agents (APs) have an important role in the pathogenesis of CSDH. The previous reported incidence rate associated ACs/APs in CSDH, is ranged from 0.6 to 22.5%1,4,6,10,16).
Recently, with increasing numbers of elderly people in the general population, the number of patients who are treated with ACs/APs is also increasing8,16,19). These drugs are commonly used as prophylactics against cerebral ischemic stroke, myocardial infarction, valvular heart disease or deep venous thrombosis6-8,16).
Thus, we aimed to study the current changes in the risk factors of CSDH with special consideration on the use of ACs/APs.
The medical records of 290 consecutive patients with CSDH from January 1996 to April 2010 were retrospectively reviewed. We classified them into three groups according to the time of admission. The Group A is defined as the patients with CSDH treated during the period from January 1996 to December 2000, Group B from January 2001 to December 2005, and Group C from January 2006 to April 2010. The Group A included 71 patients, Group B included 98 patients and Group C included 121 patients.
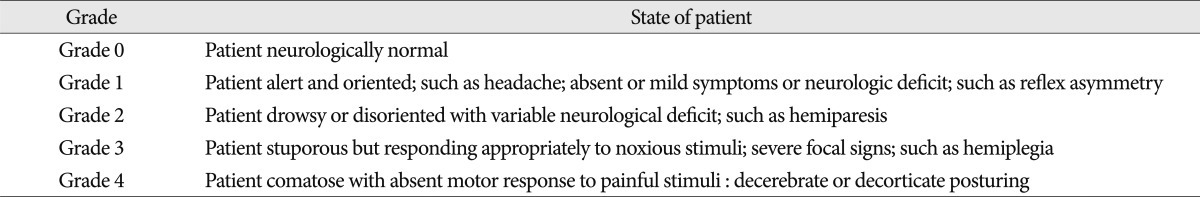
The patients' medical records and imaging data were reviewed. We analyzed the age, sex, neurological grade at admission, underlying disease, methods of operation and related factors of possible causes of CSDH. Various factors were considered to be risk factor of CSDH, such as head trauma, chronic alcoholism, epilepsy, previous shunt surgery, underlying disease having bleeding tendency and medications with ACs/APs such as warfarin, aspirin, clopidogrel, or triflusal. The criteria for chronic alcoholism was defined as more than 3 times of alcohol intake per week. All patients had been followed-up for more than 6 months until clinically regarded as in remission. On admission, neurological examination was performed using Markwalder's neurological grading system (Table 1). The diagnosis was based on brain computed tomography scan or magnetic resonance imaging prior to admission. Surgical interventions were performed by burr hole trephination with closed system drainage in 285 patients and small craniotomy with hematoma removal in 5 patients under general anesthesia. Local anesthesia was not used in any cases.
Statistical analysis was performed with Pearson chi-square test and the Student t-test to compare the variable factors that affecting the incidence of CSDH between three groups. And, ANOVA was used to analyze the relationship between medications and trauma, and medications and alcohol in each group. For all analyses, a p-value less than 0.05 was considered statistically significant (software was SPSS 12.0 for Windows, SPSS Inc., Chicago, IL, USA).
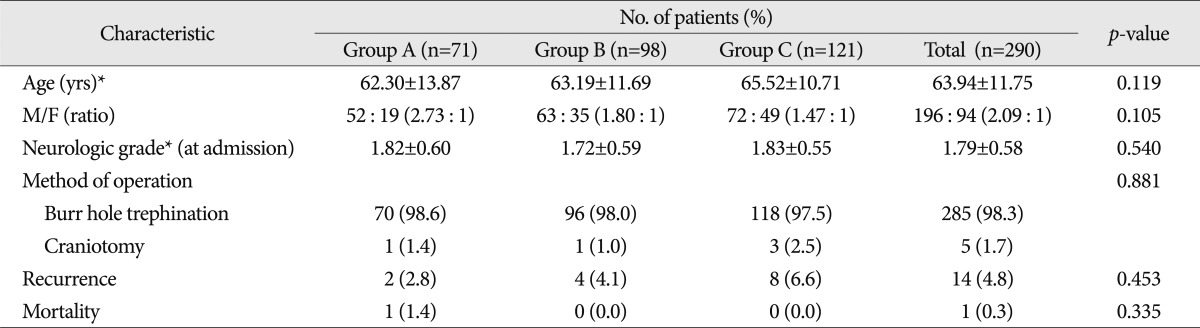
The clinical data of 290 consecutive cases were summarized in Table 2. Mean age (±standard deviation) in Group A was 62.30±13.87, whereas Group B was 63.19±11.69 and Group C was 65.52±10.71. Mean age of the patients in the latest group was increased, though it was not significant.
There were 52 men (73.2%) and 19 women (26.8%) in Group A, 63 men (64.3%) and 35 women (35.7%) in Group B, and 72 men (59.5%) and 49 women (40.5%) in Group C. Recently male preponderance have been decreased though it was not statistically significant.
Clinical findings such as preoperative neurological grade, methods of operation, recurrence rate and mortality were not different among three groups.
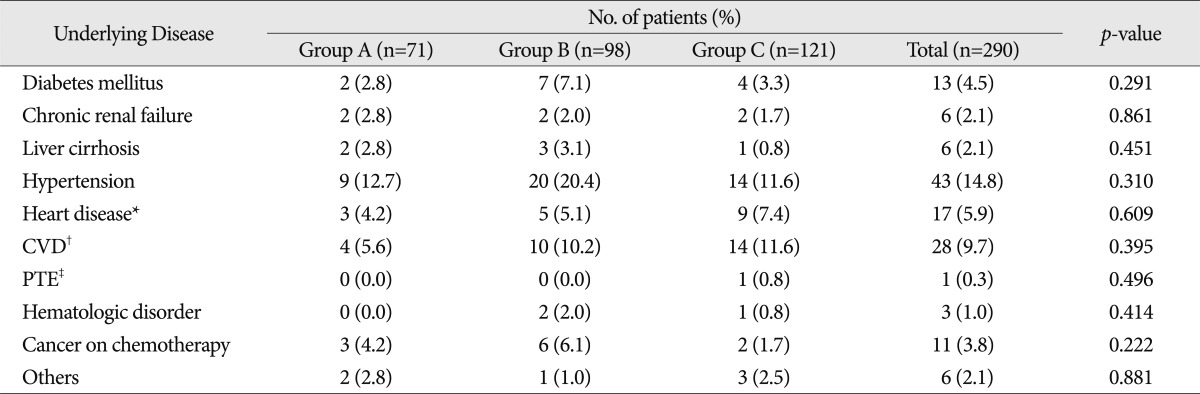
And underlying diseases in each group were analyzed in Table 3. Regarding the underlying medical conditions the recent group (Group C) had less frequent underlying diseases causing bleeding tendency such as liver cirrhosis, kidney disease, hematologic disorder, or cancer on chemotherapy, although it was not statistically significant. The share of heart disease and cerebro-vascular disease in the latest group have been somewhat increased, but it was not statistically significant.
Risk factor of CSDH in 290 patients were summarized in Table 4. Head trauma and alcoholism were major risk factors of CSDH in each group. Head trauma was the most important factor as a cause of CSDH. It was found in 49 of 71 patients (69.0%) in group A, 64 of 98 patients (65.3%) in group B, and 73 of 121 patients (60.3%) in group C. And alcoholism as the cause of CSDH was found in 16 of 71 patients (22.5%) in group A, 23 of 98 patients (23.5%) in group B, and 19 of 121 patients (15.7%) in group C. Recently, the proportion of head trauma and alcoholism have been somewhat decreased compared to the past, although it was not statistically significant.
Medications (ACs/APs) as a risk factors of CSDH were found in 3 patients (4.2%) in group A. All of the 3 patients were treated with aspirin only. ACs/APs were found in 8 patients (8.2%) in group B. Among them, 5 patients were treated with aspirin, whereas 3 patients with warfarin.
19 patients (15.7%) were taking ACs/APs in group C. Among them, 7 patients were using warfarin, and 12 patients with aspirin. Among 12 patients with aspirin, 2 patients were also treated with clopidogrel, and 2 patients with triflusal.
Recently, the frequency of ACs/APs has been increased compared to the past, and it was statistically significant (p=0.029).
Other factors such as previous neurosurgery or coagulopathy in the recent CSDH group slightly decreased, but it was not significant. There were 34 patients without any medical histories which could be causes of CSDH. We classified them as "unknown" in Table 4.
We summarized relationships of trauma and medication or alcohol and medication in Table 5 and 6. Over all period, 10 of 30 (33.3%) patients with ACs/APs had histories of head trauma whereas 174 of 260 (66.9%) patients without ACs/APs had them. Especially in group C, 7 of 19 (36.8%) patients with ACs/APs had histories of head trauma whereas 66 of 102 (64.7%) patients without ACs/APs had them. There were significantly less histories of head trauma in patients with ACs/APs related CSDH. Medications with ACs/APs were statically associated with non-traumaic CSDH, especially in the recent group (p=0.023).
Over all period, 12 of 20 (60.0%) patients with aspirin therapy and 8 of 10 (80.0%) patients with warfarin therapy had no history of previous head trauma. Regarding the type of medication, between aspirin or warfarin, there was no statistically significant difference as a cause of CSDH (p=0.735).
Over all period, only 1 of 30 (3.3%) patients with ACs/APs had histories of alcoholism, while 60 of 260 (23.1%) without ACs/APs had them. There were significantly less histories of alcoholism in patients with ACs/APs related CSDH. Medications with ACs/APs were statistically associated with non-alcoholic CSDH, especially in the recent group (p=0.025).
In our study, ACs/APs seem to behave a more important role in the development of CSDH unrelated to head trauma or alcoholism.
In the literature, many risk factors for the development of CSDH were described1,5,10,25). More than one of contributing factors can be present, and they have a cumulative effect1,5,10,25). Commonly recognized important risk factors are direct or indirect head trauma, chronic alcoholism, male gender and advanced age4,5,10,11,13,18,25). Among them, a history of head trauma is commonly understood as the most important risk factor4,5,11,13,25). Other significant factors are bleeding tendency, kidney disease, hemodialysis, liver dysfunction, epilepsy, previous shunt surgery, chemotherapeutic agents, and arachnoid cysts4,5,10,11,13,18,25). Medications with ACs/APs are also considered as risk factors of CSDH. Especially with recent widespread use of ACs/APs, its importance has increased1,6,7,10,16). But, advanced studies on the CSDH related to increasing use of ACs/APs are lacking.
As confirmed in previous studies, CSDH is a typical disease in the elderly patients10,11,14,15). Older people have a higher tendency to have CSDH, because of brain atrophy10,11,14,15,21). Brain parenchymal atrophy induces enlargement of subarachnoid space and stretching of the bridging veins10,11,14,15,21). Reported peak age of CSDH was 7th decade of life4,10,11,13,14). This result was also seen in our study as mean age of CSDH patients was 63.94 years. Moreover, mean age in the latest group have been somewhat increasing. The importance of the advanced age as a risk factor of CSDH will increase with the progression of aging society.
There is male preponderance of CSDH that men are 2-3 times more than women possible owing to greater exposure to head injuries10,11,14,15). Men with CSDH were almost twice as many as women (M : F=2.09 : 1) in our study. However, male to female ratio in recent group C (M : F=1.47 : 1) decreased when it was compared to that of remote group A (M : F=2.73 : 1) or past group B (M : F=1.80 : 1). But, it was not statistically significant.
In the literature, head trauma is considered as the most important risk factor of CSDH, and it can be identified in 50% to 80% of the patients suffering from CSDH4,6,10-16,25). Although previous minor head injuries could be sometimes unrecognized, the traumatic events were usually preceeded6,11,13,16). Previous head trauma (64.5% of 290 patients) also appears to be the most important etiological factor in our study. However, in the recent group, the proportion of head trauma as a risk factor of CSDH has decreased, although there was no statistically significance.
The frequent incidence of CSDH in chronic alcoholism is explained by that persistent alcohol intake induces brain atrophy and coagulation dysfunction4,6,10,11,13-16,25). The chronic alcoholism also has more chance of unrecognized head trauma. Reported rates of CSDH with chronic alcoholism range from 6 to 35%5,7,10,11,13-16). In our study, alcoholism still plays an important role as a risk factor like previous results, although proportion of alcoholism in CSDH have somewhat decreased.
Our results suggest that head trauma and chronic alcoholism are the most important risk factors of CSDH in agreement with earlier reports. However, prospective studies are needed for recent decreasing proportion of them in CSDH.
Reported proportion of CSDH associated with ACs/APs was ranged from 0.6% to 22.5% in the literature1,6,10,16,24). The proportion of CSDH associated with ACs/APs was reported to be 0.6% by Jeong et al.10), and 14.2% by Torihashi et al.23). The proportion of CSDH associated with warfarin was reported to be 11.8-20.0% by Gonugunta and Buxton7). The incidence of CSDH associated ACs/APs in our study (10.3% of 290 patients) was similar to previous results. But, there was significant difference between 3 groups. The rate in the recent group A (15.7%) was significantly higher than those of remote (8.2%) or past (4.2%) groups (p=0.029). We suggest that current widespread use of ACs/APs may have changed the incidence of CSDH. These agents are commonly used as prophylactic against ischemic stroke, myocardial infarction, or deep venous thrombosis8). Based on its unique cost-effectiveness and widespread availability, recently the utilization of AC and AP have expanded substantially for prevention of cardio-cerebrovascular events2,7-9,16,17,22,26). Despite the proven benefits of these drugs, concerns have been raised recently about its main side effect, hemorrhagic complications2,20,25,26). Aspirin works by irreversibly inactivating the enzyme cyclo-oxygenase, which results in decreased production of the natural platelet aggregant thromboxane A220). Clopidogrel (Plavix) also inhibits platelet aggregation by acting as glucoprotein IIb/IIIa inhibitors20). Warfarin interferes with vitamin K metabolism in the liver20). It results in the synthesis of nonfunctional coagulation factors II, VII, IV, and X, as well as protein C and S20,25). But, the reason why these mechanisms increase the incidence of intracranial hemorrhagic (ICH) complications including CSDH is unclear20). One idea is that ICH may be allowed to grow to clinical importance, because these agents inhibit normal hemostatic mechanisms2,20).
A reasonable estimates of the risk of ICH including CSDH associated with the use of these agents in primary prevention patients were variable2,3,7,9,16,20,25).
However, we came to suggestion that recent increased incidence of ICH might be a complication in aspirin users20). Physician's Health Study reported 23 hemorrhagic strokes among 11307 individuals receiving aspirin compared with 12 hemorrhagic strokes in 11034 individuals receiving placebo20). Swedish Aspirin Low-Dose Trial investigators reported that the prevalence of ICH with aspirin was 1.5%20). CAPRIE Steering Committee reported that incidence of ICH in the aspirin group was 0.47% and it was 0.33% in the clopidogrel group8). Wintzen and Tijssen25) reported that 1% of patients older than 40 years of age treated with antiplatelet agents had experienced CSDH. Mattle et al.19) reported that 23% of CSDH patients had been over anticoagulated. We obtained significant results that the proportion of ACs/APs related CSDH have increased in the recent period compared to the past and remote period (p=0.029). We think these findings are related with recent widespread use of ACs/APs. But community based epidermiologic survey is necessary to confirm that ACs/APs have increased actual incidence of CSDH.
In our series, CSDH cases associated with ACs/APs have significantly less history of trauma or alcoholism (p=0.023, 0.025 respectively). Lindvall and Koskinen16) reported similar finding that 71% in the non-trauma group were treated with ACs/APs compared to 18% in the trauma group.
These findings suggest that causative role of the ACs/APs in the development of CSDH unrelated with head trauma or alcoholism.
Thus, we conclude that recent increase in the CSDH cases associated with ACs/APs is not a epiphenomenon, but an actual increase in the incidence of drug-related CSDH cases. This phenomenon will probably be more prominent in the future with widespread use of ACs/APs. Other factors surveyed such as underlying disease, previous shunt surgery and epilepsy had no statistically significant changes. However, our study is not a community based one, so we suggest such a kind of survey to get the actual prevalence of ACs/APs prescription and real incidence of ACs/APs related CSDH.
Recently, there have been some changes in the risk factors of CSDH. In particular, ACs/APs have become more significant important as risk factors of CSDH, compared to the past. With widespread use of these drugs in modern cardio-cerebrovascular disease prevention, careful attention should be taken as important factors of CSDH. When medications such as aspirin or warfarin are used for prevention of cardio-cerebrovascular disease, the benefits of the drugs should outweigh possible harm from a risk of CSDH. Furthermore, community-based prospective studies are needed to quantify the actual changes in the incidence of CSDH associated with ACs/APs.
References
1. Baechli H, Nordmann A, Bucher HC, Gratzl O. Demographics and prevalent risk factors of chronic subdural haematoma : results of a large single-center cohort study. Neurosurg Rev. 2004; 27:263–266. PMID: 15148652.
2. Bershad EM, Farhadi S, Suri MF, Feen ES, Hernandez OH, Selman WR, et al. Coagulopathy and inhospital deaths in patients with acute subdural hematoma. J Neurosurg. 2008; 109:664–669. PMID: 18826353.

3. The Stroke Prevention in Atrial Fibrillation Investigators. Bleeding during antithrombotic therapy in patients with atrial fibrillation. Arch Intern Med. 1996; 156:409–416. PMID: 8607726.
4. Chen JC, Levy ML. Causes, epidemiology, and risk factors of chronic subdural hematoma. Neurosurg Clin N Am. 2000; 11:399–406. PMID: 10918008.

5. Choi WW, Kim KH. Prognostic factors of chronic subdural hematoma. J Korean Neurosurg Soc. 2002; 32:18–22.
6. Forster MT, Mathé AK, Senft C, Scharrer I, Seifert V, Gerlach R. The influence of preoperative anticoagulation on outcome and quality of life after surgical treatment of chronic subdural hematoma. J Clin Neurosci. 2010; 17:975–979. PMID: 20580997.

7. Gonugunta V, Buxton N. Warfarin and chronic subdural haematomas. Br J Neurosurg. 2001; 15:514–517. PMID: 11814005.

8. Gorelick PB, Weisman SM. Risk of hemorrhagic stroke with aspirin use : an update. Stroke. 2005; 36:1801–1807. PMID: 16020759.
9. Hart RG, Boop BS, Anderson DC. Oral anticoagulants and intracranial hemorrhage. Facts and hypotheses. Stroke. 1995; 26:1471–1477. PMID: 7631356.
10. Jeong JE, Kim GK, Park JT, Lim YJ, Kim TS, Rhee BA, et al. A clinical analysis of chronic subdural hematoma according to age factor. J Korean Neurosurg Soc. 2000; 29:748–753.
11. Kang HL, Shin HS, Kim TH, Hwang YS, Park SK. Clinical analysis of recurrent chronic subdural hematoma. J Korean Neurosurg Soc. 2006; 40:262–266.
12. Kang MS, Koh HS, Kwon HJ, Choi SW, Kim SH, Youm JY. Factors influencing recurrent chronic subdural hematoma after surgery. J Korean Neurosurg Soc. 2007; 41:11–15.
13. Ko BS, Lee JK, Seo BR, Moon SJ, Kim JH, Kim SH. Clinical analysis of risk factors related to recurrent chronic subdural hematoma. J Korean Neurosurg Soc. 2008; 43:11–15. PMID: 19096538.

14. Kwon HJ, Youm JY, Kim SH, Koh HS, Song SH, Kim Y. Postoperative radiological changes in chronic subdural hematoma and its relation to recurrence. J Korean Neurosurg Soc. 2004; 35:410–414.
15. Lee JK, Choi JH, Kim CH, Lee HK, Moon JG. Chronic subdural hematomas : a comparative study of three types of operative procedures. J Korean Neurosurg Soc. 2009; 46:210–214. PMID: 19844620.

16. Lindvall P, Koskinen LO. Anticoagulants and antiplatelet agents and the risk of development and recurrence of chronic subdural haematomas. J Clin Neurosci. 2009; 16:1287–1290. PMID: 19564115.

17. Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994-1998 : analysis of data from the general practice research database. Heart. 2001; 86:284–288. PMID: 11514479.

18. Markwalder TM. Chronic subdural hematomas : a review. J Neurosurg. 1981; 54:637–645. PMID: 7014792.
19. Mattle H, Kohler S, Huber P, Rohner M, Steinsiepe KF. Anticoagulation related intracranial extracerebral haemorrhage. J Neurol Neurosurg Psychiatry. 1989; 52:829–837. PMID: 2769275.
20. Quinones-Hinojosa A, Gulati M, Singh V, Lawton MT. Spontaneous intracerebral hemorrhage due to coagulation disorders. Neurosurg Focus. 2003; 15:E3. PMID: 15344896.

21. Roob G, Fazekas F. Magnetic resonance imaging of cerebral microbleeds. Curr Opin Neurol. 2000; 13:69–73. PMID: 10719653.

22. Spektor S, Agus S, Merkin V, Constantini S. Low-dose aspirin prophylaxis and risk of intracranial hemorrhage in patients older than 60 years of age with mild or moderate head injury : a prospective study. J Neurosurg. 2003; 99:661–665. PMID: 14567600.

23. Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S. Independent predictors for recurrence of chronic subdural hematoma : a review of 343 consecutive surgical cases. Neurosurgery. 2008; 63:1125–1129. discussion 1129. PMID: 19008766.
24. Weir B, Gordon P. Factors affecting coagulation : fibrinolysis in chronic subdural fluid collections. J Neurosurg. 1983; 58:242–245. PMID: 6848682.

25. Wintzen AR, Tijssen JG. Subdural hematoma and oral anticoagulant therapy. Arch Neurol. 1982; 39:69–72. PMID: 7059302.

26. Zingale A, Chibbaro S, Florio A, Distefano G, Porcaro S. Management of chronic subdural hematoma in patients treated with anticoagulation. J Neurosurg Sci. 1999; 43:277–284. PMID: 10864390.
Table 4
The risk factors of CSDH in 290 patients
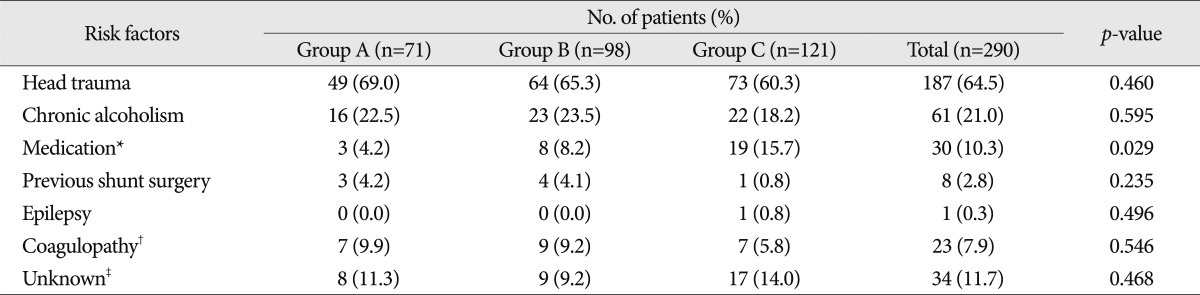
*Antiplatelet agents (including aspirin, clopidogrel, or trifulsal) or anticoagulants (warfarin), †Medical condition having bleeding tendency such as liver cirrhosis, chronic renal failure, receiving chemotherapy, or hematologic disorders, ‡Having no clinical history that could be a cause of CSDH. CSDH : chronic subdural hematoma




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download