Abstract
Spinal angiolipomas are rare lesions usually found in the epidural space of the thoracic spine. The infiltrating type of spinal angiolipomas is extremely rare. This report presents the case and reviews the related literature. A 58-year-old man was presented with a 7-month history of progressive weakness and sensory change of lower extremities. Magnetic resonance images showed a well-enhanced mass infiltrating the vertebral foramen at the T4-5 level. Resection of the tumor was performed. Histological study revealed the tumor as an angiolipoma. The patient was relieved from symptoms after tumor resection.
Spinal angiolipomas, benign tumors of fatty tissue of the spinal axis, are very rare3,13). They are usually present with slowly progressing signs and symptoms of cord compression from an epidural mass13). The most common location is the epidural mid-thoracic area5,10,13). This predilection may be explained by the tenuous blood supply of the thoracic spine with subsequent neovascularization of the ischemic area8). Angiolipomas are distinct entities from lipomas as they contain vascular tissue occurring mainly in adults and lack associated malformations13). Spinal angiolipomas are composed of mature fat cells and abnormal blood vessels that vary from capillary through sinusoid or venular to arterial in size3,10).
Angiolipomas can be further categorized into two subtypes : noninfiltrating and infiltrating. The noninfiltrating type is more common and is usually well encapsulated. The infiltrating ones are partially or entirely unencapsulated, ill-defined, and infiltrate the surrounding tissues, especially the bone2,5,9). Gelabert-González and García-Allut4) reviewed the literature of spinal angiolipoma since 1892 and found 123 cases of spinal angiolipomas. To the best our knowledge, approximately 18 cases of spinal infiltrating angiolipoma have been reported in the medical literature. This report now presents a case of thoracic infiltrating angiolipoma and reviews the literature on this rare entity.
A 58-year-old man was presented with progressive weakness and sensory change in the lower extremities for seven months. Neurological examination revealed weakness of lower extremities (manual muscle testing, MMT grade 4) and hypesthesia below the level of T10. Deep tendon reflexes were hyperactive on the right leg. Spine computed tomography (CT) scan revealed that the mass lesion compressed the spinal cord severely in the posterior extradural space at the T4-5 level, and it extended into the right T4-5 neural foramen to the paraspinal space. Due to the mass, right T4-5 neural foramen widen and scalloped (Fig. 1). On thoracic magnetic resonance image (MRI), the infiltrating epidural thoracic mass showed iso-signal intensity on T1-weighted image (WI), slightly high signal on T2WI, and homogenous enhancement with gadolinium (Fig. 2).
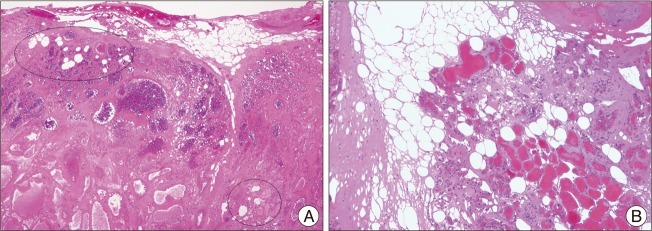
The patient underwent an operation. Afterwards, a total laminectomy of lower T3, T4, and T5, epidural fat was encountered at both the upper and lower end of the lesion. Below the epidural fat, the reddish-gray colored and highly vascularized mass appeared. The mass was removed by piecemeal pattern and dissected from the dura in spite of profuse bleeding. We excised all of the epidural mass but left behind a tumor part of the paraspinal portion. Microscopic examination revealed a mixture of mature adipose and abundant vascular tissues. Vascular components show a mixed pattern of capillary, cavernous, and venous type. Some fibrin thrombi are seen in the capillaries (Fig. 3). Immunohistochemistry stained positive for CD34 and smooth muscle actin (SMA) that were consistent with an angiolipoma. The patient showed improvement in strength (MMT grade 4+) and sensation in the days following surgery. Follow-up thoracic CT 18 months after surgery did not show recurred posterior epidural mass lesion except the remnant paraspinal lesion (Fig. 4).
In 1901, Liebscher was the first to describe a spinal angiolipoma4). However, the term angiolipoma was recognized in 1960 by Howard and Helwig as an anatomopathological entity containing mature fat cells and proliferating vessel6).
The pathogenesis of angiolipomas remains unclear, although several theories have been suggested10,13). Bardosi et al.1) postulated that angiolipomas originate from adipocytes with secretory activity containing lipid-like material in perivascular granules. Predisposing factors for angioliopomas have not been clearly established7). Weight gain in pregnancy was observed to increase the risk of angiolipoma11).
Plain radiography is often negative, whereas infiltrating tumors cause trabeculation of the affected vertebral body7). CT scan demonstrates a hypodense lesion and provides information on the degree of bony involvement7,13). MRI is the most valuable radiological technique for diagnosing spinal angiolipomas4,13). Spinal epidural angiolipomas are usually hyperintense and inhomogeneous on T1WIs with intense homogeneous enhancement5,13) while T2WI can be variable, but are usually hyperintense4,13). In the current case, iso-intensity on T1WIs correlated with increased vascularity within the spinal angiolipoma.
Noninfiltrating and infiltrating angiolipomas are considered histologically benign, although infiltrating angiolipomas have a locally aggressive nature and can erode the local bone, muscle, and neural and fibrocollagenous tissues12). The signs and symptoms do not differ from any other benign spinal tumors and the duration of symptoms is usually long in both non-infiltrating and infiltrating types5).
Fourney et al.2) reviewed all spinal angiolipomas in literature. The majority of cases (76%) were epidural without local infiltration, whereas the infiltrated vertebral bone (17%), with or without extension into the thoracic cavity, and intramedullary lesions (5%) were likewise presented.
Surgery appears to be the treatment of choice, and complete excision appears to be curative in most cases3,4,13) For the infiltrating type, a total resection can be more difficult. However, most patients have a good prognosis even with subtotal removal as these lesions are slowly growing and do not undergo malignant transformation5). Our case with subtotal resection presents no recurrence after 18 months of follow-up. No adjuvant radiation should be applied to patients with this benign pathological entity, even in the infiltrating group4).
References
1. Bardosi A, Schaake T, Friede RL, Roessmann U. Extradural spinal angiolipoma with secretory activity. An ultrastructural, clinico-pathological study. Virchows Arch A Pathol Anat Histopathol. 1985; 406:253–259. PMID: 3923701.
2. Fourney DR, Tong KA, Macaulay RJ, Griebel RW. Spinal angiolipoma. Can J Neurol Sci. 2001; 28:82–88. PMID: 11252303.

3. Gelabert-González M, Agulleiro-Díaz J, Reyes-Santías RM. Spinal extradural angiolipoma, with a literature review. Childs Nerv Syst. 2002; 18:725–728. PMID: 12483360.

4. Gelabert-González M, García-Allut A. Spinal extradural angiolipoma : report of two cases and review of the literature. Eur Spine J. 2009; 18:324–335. PMID: 19127373.

5. Guzey FK, Bas NS, Ozkan N, Karabulut C, Bas SC, Turgut H. Lumbar extradural infiltrating angiolipoma : a case report and review of 17 previously reported cases with infiltrating spinal angiolipomas. Spine J. 2007; 7:739–744. PMID: 17998134.

7. Hungs M, Paré LS. Spinal angiolipoma : case report and literature review. J Spinal Cord Med. 2008; 31:315–318. PMID: 18795485.
8. Labram EK, el-Shunnar K, Hilton DA, Robertson NJ. Revisited : spinal angiolipoma--three additional cases. Br J Neurosurg. 1999; 13:25–29. PMID: 10492681.
9. Leu NH, Chen CY, Shy CG, Lu CY, Wu CS, Chen DC, et al. MR imaging of an infiltrating spinal epidural angiolipoma. AJNR Am J Neuroradiol. 2003; 24:1008–1011. PMID: 12748114.
10. Nanassis K, Tsitsopoulos P, Marinopoulos D, Mintelis A, Tsitsopoulos P. Lumbar spinal epidural angiolipoma. J Clin Neurosci. 2008; 15:460–463. PMID: 18249122.

11. Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas. Report of three cases. J Neurosurg. 1993; 78:280–286. PMID: 8421211.
12. Rabin D, Hon BA, Pelz DM, Ang LC, Lee DH, Duggal N. Infiltrating spinal angiolipoma : a case report and review of the literature. J Spinal Disord Tech. 2004; 17:456–461. PMID: 15385889.
13. Samdani AF, Garonzik IM, Jallo G, Eberhart CG, Zahos P. Spinal angiolipoma : case report and review of the literature. Acta Neurochir (Wien). 2004; 146:299–302. discussion 302. PMID: 15015054.
Fig. 1
Axial CT scans of lower T4 level shows an infiltrating epidural mass extended to the right T4-5 neural foramen which was widening and scalloping.
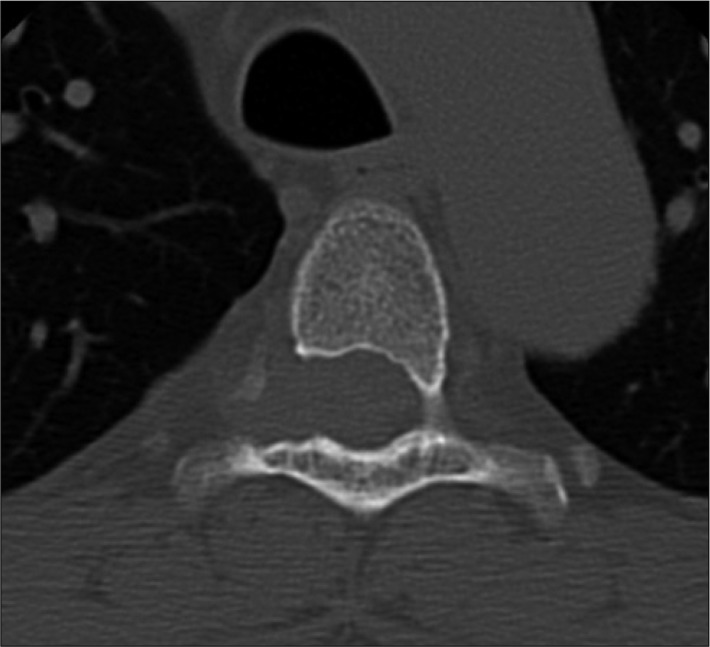
Fig. 2
MRI of thoracic spine. A : T1WI axial image with gadolinium (Gd) enhancement showing homogenous enhancing mass posterior to the spinal cord extending into the right T4-5 neural foramen (arrow). B : T1WI sagittal image reveals iso-signal lenticular-shaped mass at T4-5 level with marked cord compression. C : T1WI sagittal image with Gd administration demonstrating well the homogeneous enhancement.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download