Abstract
Spontaneous hematomas of the iliacus muscle are rare lesions and these are seen in individuals receiving anticoagulation therapy or patients with blood dyscrasias such as hemophilia. It can cause femoral neuropathy and resultant pain and paralysis. Although there is no clear consensus for the treatment of femoral neuropathy from iliacus muscle hematomas, delays in the surgical evacuation of hematoma for decompression of the femoral nerve can lead to a prolonged or permanent disability. We report here on a rare case of a spontaneous iliacus muscle hematoma that caused femoral neuropathy in a patient who was taking warfarin for occlusive vascular disease and we discuss the treatment.
Hematoma of the iliacus muscle is a rare lesion. It occurs, most often, in patients receiving anticoagulation therapy or in patients with either inherited or acquired clotting disorders11). It has also been reported to occur following trauma, harvesting an anterior iliac crest bone graft and hip arthroplasy4,8,14). It can occur even in a healthy patient who is not undergoing anticoagulant treatment or suffering from a clotting disorder6). It can cause severe pain in the affected groin, hip and thigh, and it can cause quadriceps weakness. Other associated findings may include a fall in the hematocrit, tachycardia, hypotension, abdominal pain and a palpable mass, depending on the severity of hemorrhgage11). Because of the rareness of this condition, the optimal treatment of iliacus muscle hematoma with associated femoral neuropathy remains controversial.
We report here on a rare case of a spontaneous iliacus muscle hematoma that caused femoral neuropathy in a patient who was taking warfarin for occlusive vascular disease with the discussion of the treatment.
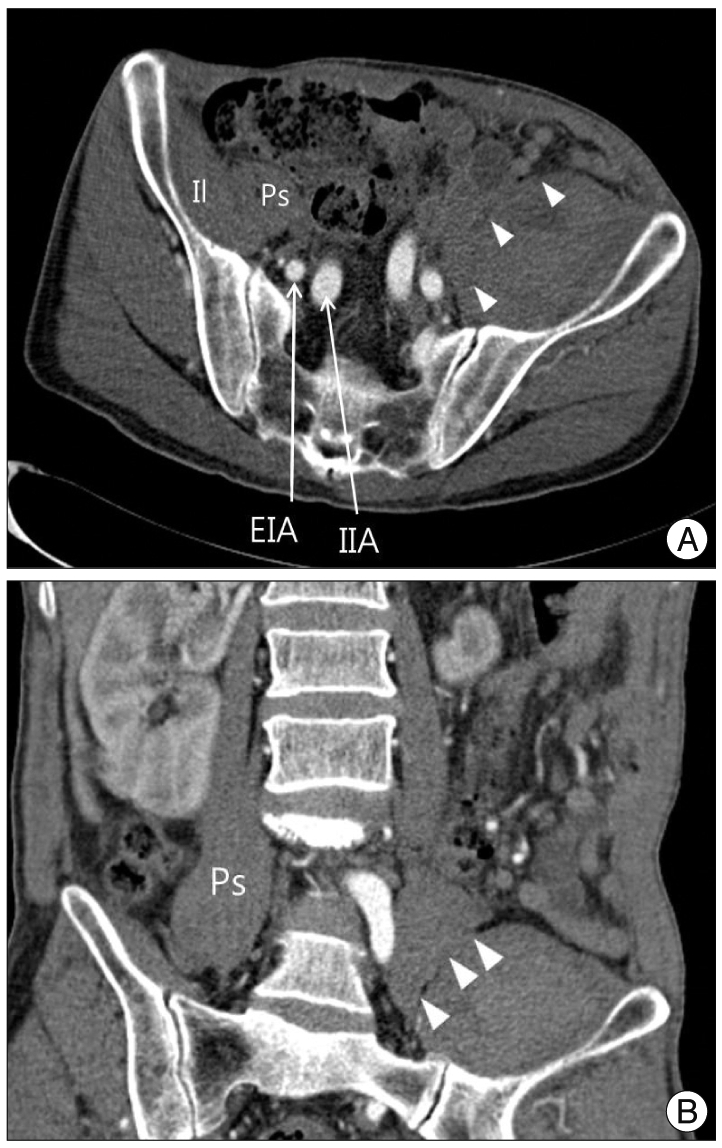
A 55-year-old male presented with severe pain and numbness in the groin that radiated to the left anterior thigh. After the sudden onset of the pain, weakness on the left lower extremity developed and this had worsened for one week. He had a previous history of a thrombectomy in the left femoral artery two years before and in the left external iliac artery one month before. He had taken warfarin for two years after the first thrombectomy. On admission, his vital signs were stable. His prothrombin time international normalized ratio was 1.6, the hemoglobin was 9.7 g/dL and the platelet count was 223×103/µL. Physical examination revealed paresis of the left quadriceps muscle with strength of 4/5 and a diminished knee jerk reflex. The femoral, popliteal and dorsalis pedis pulses were palpable but slightly weak and no change in the skin color was found. He kept the left knee flexed and complained of aggravated pain when he extended the knee. Initially, vascular insufficiency due to partial arterial occlusion by thrombus was suspected. But computed tomography (CT) angiography and Doppler ultrasonography revealed patent proximal arteries and intact flows on the lower extremities. The source images for CT angiography revealed the iliacus muscle hematoma (Fig. 1). Because the left psoas muscle was compressed and displaced by the hematoma compared with right psoas muscle and the femoral nerve runs between the psoas tendon and the iliacus muscle, compression or displacement of the left femoral nerve was suspected. The warfarin was immediately discontinued and he was managed with pain control and regular neurological assessment. But, his pain and weakness were further increased over the next five days. He became unable to raise the left leg and to stand without assistance. Electromyography and nerve conduction study showed left femoral neuropathy. After confirming the normalization of his coagulation parameters, percutaneous catheter insertion was performed under ultrasonographic guidance for aspiration and drainage of the hematoma. However, only a small amount of the hematoma was drained and then surgical evacuation of the hematoma via the left retroperitoneal approach was performed. The hematoma was under significant pressure and the psoas muscle was compressed. Soon after making the incision on the iliacus fascia, old blood clot gushed out. The hematoma was gently evacuated with the suction and forceps and irrigated, and a Jackson Pratt drain was placed for continued drainage.
The postoperative course was uneventful and the paresis of the quadriceps muscle slowly improved. Abdominal CT scan showed a decreased amount of the hematoma one month after the surgery (Fig. 2). He demonstrated recovery of his femoral nerve function, with an improvement of the quadriceps strength to Grade 4/5 at the 1-year-follow-up examination, but limping in his left leg remained.
The femoral nerve develops within the body of the psoas muscle from the posterior division of L2-L4. The femoral nerve then runs between the psoas tendon and the iliacus muscle beneath the iliacus fascia to the femoral canal, under the inguinal ligament11). Anatomic studies have revealed that the fascia overlying the iliacus muscle and the femoral nerve is strong and not easily stretched in the presence of underlying hematoma formation10). As a result, femoral nerve compression occurs along the iliopsoas gutter, where it is also at the most risk for ischemia due to the poor vascular supply to this region of the nerve. In addition, the hematoma may track down the iliacus muscle into the femoral canal and compress the femoral nerve against the rigid inguinal ligament, resulting in further ischemia and resultant neuropathy10,11). Goodfellow et al.3) demonstrated that a hematoma that is responsible for femoral nerve palsy is necessarily situated in the iliacus muscle and not in the psoas muscle. Fluid injected into the iliacus muscle or fascial sheath produces high pressure, and this compresses the femoral nerve against the psoas muscle tendon and induces an ischemic femoral neuropathy. An iliacus muscle hematoma never drains spontaneously, rather, it persists for a long period of time and induces chronic compression of the femoral nerve and then the hematoma becomes organized16). In the present case, the hematoma was found within the iliacus muscle and not in the psoas muscle. It might have stretched the iliacus fascia, and compressed and displaced the femoral nerve.
Although hematoma of the iliacus muscle has been reported to occur following trauma, harvesting an anterior iliac crest graft, hip arthroplasy, and even in a normal patient, it has been reported primarily in patients suffering from hemophilia and those receiving heparin or oral anticoagulant therapies4,6,8,11,14). The incidence of retroperitoneal hemorrhage has been reported at 1.3-6.6% of the patients undergoing therapeutic anticoagulation and at 5.5% and 10.4% of the patients with hemophilia1,2,11). It has also been reported in association with the use of antiplatelet agents9). Therapeutic anticoagulation is a frequently utilized treatment for a number of conditions, including atrial fibrillation, deep vein thrombosis, pulmonary embolism and so on. As the number of patients undergoing anticoagulation therapy increases, hemorrhagic complications will become more common11).
The treatment of iliacus muscle hematoma with associated femoral neuropathy remains controversial because of the rareness of this condition. Treatment depends on the speed of onset, the volume and the degree of neurological impairment6). A conservative approach is justified for hemodynamically stable patients with smaller hematomas, moderate neurological symptoms and there is no active bleeding6,11,14). In the case of active bleeding, transarterial embolization can be a treatment option13,15). Wada et al. advocated that because of its lower morbidity, transarterial embolization should be considered instead of surgery13). For large haematomas with severe motor function inhibition, if the lesion progresses or there is evidence of neurological worsening, then surgical treatment is mandatory by decompression and drainage5,11,16). Parmer et al.11) suggested when surgical hematoma evacuation was performed at the first identification of neuropathy, a full return of function is more likely to occur, and those patients who are treated conservatively for an extended period despite the presence of femoral neuropathy continue to have prolonged neurological deficit despite eventual intervention. In one series, all the patients who had a femoral motor deficit and who were conservatively treated or underwent surgical drainage after 48 hours had a permanent femoral nerve distribution paresis16). More recently, Pirouzmand and Midha recommended early fasciotomy of the iliacus muscle. They reasoned that early fasciotomy with or without hematoma evacuation should be considered in order to provide rapid decompression and to minimize the chance of permanent nerve injury. Nevertheless, they did not provide any specific information regarding the hematoma volume and management decisions12). In the present case, the patient's pain and motor weakness became worse despite of initial conservative management, and surgical evacuation of the hematoma was performed two weeks after the onset of pain and weakness. Although there was improvement in the quadriceps power after the surgery, he still walked with a limp in his left leg.
An alternative to open surgical treatment is percutaneous decompression. Merrick et al.7) reported the return of nerve function by percutaneous decompression of a retroperitoneal hematoma and they suggested that percutaneous drainage may represent a reasonable alternative to or the first step in surgical treatment. Of note, this treatment can be used only for liquid hematomas and it would not be useful for patients whose diagnosis is delayed until they already have organized hematomas14). In the present case, at the time two weeks after the onset of symptoms, the organized hematoma made percutaneous aspiration or drainage impossible, and this led us to perform open surgical treatment.
Spontaneous iliacus muscle hematoma should be considered in the differential diagnosis of leg pain in a patient who is on anticoagulation therapy. Although there is no clear consensus for the treatment of femoral neuropathy associated with iliacus muscle hematoma, the development of associated femoral neuropathy mandates early operative intervention. Delays in the surgical evacuation of a hematoma for decompressing the femoral nerve can lead to a prolonged or permanent disability.
References
1. Ashrani AA, Osip J, Christie B, Key NS. Iliopsoas haemorrhage in patients with bleeding disorders--experience from one centre. Haemophilia. 2003; 9:721–726. PMID: 14750939.

2. Balkan C, Kavakli K, Karapinar D. Iliopsoas haemorrhage in patients with haemophilia : results from one centre. Haemophilia. 2005; 11:463–467. PMID: 16128889.

3. Goodfellow J, Fearn CB, Matthews JM. Iliacus haematoma. A common complication of haemophilia. J Bone Joint Surg Br. 1967; 49:748–756. PMID: 6073189.
4. Guha SC, Poole MD. Stress fracture of the iliac bone with subfascial femoral neuropathy : unusual complications at a bone graft donor site : case report. Br J Plast Surg. 1983; 36:305–306. PMID: 6860856.

5. Guivarc'h M. [Hematoma of the iliac psoas muscle. 29 cases]. J Chir (Paris). 1997; 134:382–389. PMID: 9682753.
6. Marquardt G, Barduzal Angles S, Leheta F, Seifert V. Spontaneous haematoma of the iliac psoas muscle : a case report and review of the literature. Arch Orthop Trauma Surg. 2002; 122:109–111. PMID: 11880914.
7. Merrick HW, Zeiss J, Woldenberg LS. Percutaneous decompression for femoral neuropathy secondary to heparin-induced retroperitoneal hematoma : case report and review of the literature. Am Surg. 1991; 57:706–711. PMID: 1660685.
8. Nakamura Y, Mitsui H, Toh S, Hayashi Y. Femoral nerve palsy associated with iliacus hematoma following pseudoaneurysm after revision hip arthroplasty. J Arthroplasty. 2008; 23:1240e1–e4. PMID: 18534465.

9. Nakao A, Sakagami K, Mitsuoka S, Uda M, Tanaka N. Retroperitoneal hematoma associated with femoral neuropathy : a complication under antiplatelets therapy. Acta Med Okayama. 2001; 55:363–366. PMID: 11779099.
10. Nobel W, Marks SC Jr, Kubik S. The anatomical basis for femoral nerve palsy following iliacus hematoma. J Neurosurg. 1980; 52:533–540. PMID: 6445414.

11. Parmer SS, Carpenter JP, Fairman RM, Velazquez OC, Mitchell ME. Femoral neuropathy following retroperitoneal hemorrhage : case series and review of the literature. Ann Vasc Surg. 2006; 20:536–540. PMID: 16741653.

12. Pirouzmand F, Midha R. Subacute femoral compressive neuropathy from iliacus compartment hematoma. Can J Neurol Sci. 2001; 28:155–158. PMID: 11383942.

13. Qanadli SD, El Hajjam M, Mignon F, Bruckert F, Chagnon S, Lacombe P. Life-threatening spontaneous psoas haematoma treated by transcatheter arterial embolization. Eur Radiol. 1999; 9:1231–1234. PMID: 10415268.

14. Rochman AS, Vitarbo E, Levi AD. Femoral nerve palsy secondary to traumatic pseudoaneurysm and iliacus hematoma. J Neurosurg. 2005; 102:382–385. PMID: 15739570.

15. Wada Y, Yanagihara C, Nishimura Y. Bilateral iliopsoas hematomas complicating anticoagulant therapy. Intern Med. 2005; 44:641–643. PMID: 16020897.

Fig. 1
Source images of the computed tomography angiography of the lower extremities. Axial (A) and sagittal (B) images show an iliacus hematoma compressing the left psoas muscle (white arrow heads), as compared with the right psoas muscle. EIA : external iliac artery, IIA : internal iliac artery, Il : iliacus muscle, Ps : psoas muscle.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download