Abstract
We report a patient with a ruptured vertebral artery (VA) dissecting aneurysm that was treated by internal trapping of the aneurysm and parent artery using detachable coils with subsequent antegrade recanalization of occluded vertebral artery during the follow-up period. A 38-year-old man was admitted with a ruptured right VA dissecting aneurysm just distal to origin of right posterior inferior cerebellar artery. The dissected segment of the VA was occluded by coil embolization. The 14 months follow-up angiography showed that dissected aneurysm was completely occluded, but the parent artery was recanalized in an antegrade fashion. Based on this unique case, the authors suggest that careful angiographic follow-up of dissecting aneurysm is required, even in patients successfully treated with endovascular occlusion of the affected artery and aneurysm.
Dissecting aneurysms of the intracranial vertebral artery are increasingly diagnosed as a cause of subarachnoid hemorrhage (SAH), especially in young to middle-aged adults. Once ruptured to cause SAH, dissecting aneurysms are associated with a high incidence of re-bleeding and a high mortality rate at the time of re-bleeding, indicating the need for early treatment6). The most commonly accepted treatment modality is complete isolation of the dissected segment by surgical trapping or endovascular occlusion. Because surgery involves high risks for treatment-related morbidity and mortality, an endovascular method is preferred in treating vertebral artery dissecting aneurysm3,8,10). In endovascular treatment, shifting from proximal occlusion of vertebral artery to internal trapping of dissected site using controllable detachable coils has been advocated as a primary treatment with or without bypass.
In the preset article, we describe a case in which an occluded vertebral artery recanalized in an antegrade fashion, despite internal trapping of the aneurysm and affected artery using controllable coils. Possible explanations for the antegrade recanalization of the occluded vertebral artery are also discussed.
A 38-year-old man, with a history of stupor (Hunt and Hess grade III) after sudden severe headache, was admitted to our emergency room, where computed tomography (CT) revealed SAH predominantly in the posterior fossa and basal cistern. The patient had a history of hypertension. However, he did not have any previous neurologic disease, or history of drug abuse. Following CT angiography (CTA) revealed fusiform dilatation of right intracranial vertebral artery. Coronal CT source image also showed low density intimal flap and pseudoaneurysm, consistent with a dissecting aneurysm (Fig. 1). The cerebral angiography showed a fusiform aneurysm of the right distal vertebral artery and prolonged contrast stagnation in the false lumen of dissecting aneurysm. A washout of the contrast was also observed at the same time in the parent artery. The right posterior inferior cerebellar artery (PICA) arose proximal to the dissected segment of the intracranial right vertebral artery (Fig. 2). The vertebral arteries were codominant.
Endovascular treatment under general anesthesia was then performed just after the diagnostic angiography. A bolus of intravenous heparin (50-IU/kg body weight) was administered to achieve an activated clotting time of greater than 250 seconds. Next, 6 F guide catheter (Envoy, Cordis endovascular, Miami Lakes, FL, USA) was placed in the right vertebral artery via a femoral vascular sheath. An Excelsior SL-10 microcatheter (Boston Scientific/Target Therapeutics, Fermont, CA, USA) was prepared and passed into the distal right vertebral artery over an Agility 14 soft microguidewire (Cordis endovascular, Miami Lakes, FL, USA). The microcatheter was navigated to the dilated segment of the aneurysm in an attempt to occlude the dissection site and parent artery. Multiple GDCs (Boston Scientific/Target therapeutics, Fermont, CA, USA), totaling 100 cm in length, were placed at the dilated segment only. The dissecting aneurysm and affected right vertebral artery were both completely occluded, whereas the right PICA was preserved (Fig. 3). The opposite left vertebral artery adequately supplied the basilar artery and both posterior cerebral arteries. The patient was allowed to emerge from the anesthesia and transferred to the neurosurgical intensive care unit with no untoward events. A follow-up CTA performed 12 days after the procedure showed no residual or recurrence of aneurysm. The patient was doing well and returned to work 2 months after the onset of the symptoms. Fourteen months after the embolization, another follow-up angiography was performed, which revealed spontaneous recanalization of the occluded right vertebral artery with a normal arterial configuration and antegrade flow into the basilar artery. The recanalized vertebral artery was located just inferior and medial to the deployed coil meshes (Fig. 4). It was decided that no further intervention was needed. At the last clinical follow-up 16 months after initial treatment, the patient was fully symptom free.
Ruptured vertebrobasiar artery dissecting aneurysms have an extremely high rate of early rebleeding, and rebleeding is associated with a poor clinical outcome6). Considering the aggressive behavior of ruptured vertebral dissecting aneurysms, most definitive treatment is parent vessel deconstruction. This can be achieved by using either open surgical trapping or endovascular balloon or coil occlusion2). Several recent reports have shown that even deconstructive approach achieved by endovascular procedures does not completely eliminate the risk of re-bleeding from ruptured vertebral artery dissecting aneurysm4). However, endovascular occlusion of the affected site, including both aneurysm and parent artery, may be considered the first option for treatment in patients who will tolerate sacrifice of the parent vessel along its diseased segment5).
Baik et al.1) reported a rare case of ruptured vertebral artery dissecting aneurysm that was treated by endovascular occlusion of the aneurysm and parent artery. Nine months following endovascular treatment, the vertebral artery recanalized in an antegrade fashion. Similiarly, Sawada et al.9) also reported two rare cases of ruptured vertebral artery dissecting aneurysms that were treated using GDCs, and the recanalized vertebral artery in an antegrade fashion was found during the follow-up period (3-6 months). In the present case, internal trapping was performed using detachable coils, thereby sacrificing the parent artery at the level of dissection and completely occluding the dissecting aneurysm. During follow-up period, right vertebral angiogram obtained fourteen months after endovascular treatment revealed recanalization of the antegrade blood flow just inferior and medial to the occluded coil meshes with the dissecting aneurysm.
For our rare recanalization case, we propose possibilities for the actual mechanism of the antegrade recanalization related to the internal trapping of a dissecting aneurysm. First, the true lumen may have been occluded by the false lumen. Thus, if the false lumen had both entrance and an exit and true lumen was collapsed based on the enlarged false lumen, the abnormal configuration of the dilated segment of the dissection may have been just the false lumen. As a consequence, the microcatheter could have been placed into the false lumen, thereby occluding the false lumen with the aneurysm in the initial procedure. Then, several months later, although the false lumen was still occluded, another channel opened in the true lumen that had been compressed by the enlarged false lumen. In our present case, the initial CTA coronal source images depicted a thin layer of intimal flap of the dissecting aneurysm and following angiogram also revealed persistent contrast stasis in the dissected false lumen. If the microcatheter had been navigated into the false lumen, thereby occluding the false lumen by detachable coils, then the false lumen could have compressed the true lumen during the initial treatment. On the other hand, technical explanation was also considered, such as, deployed coils did not cover the entry zone of the dissecting aneurysm and parent artery on the postembolization angiography. Given the proximity of PICA origin to dissecting aneurysm, there existed possibility of incomplete obliteration of the entry zone of dissecting aneurysm because blood flow to the PICA needed to be preserved. Finally, it was also considered whether the coil packing of the aneurysm was insufficient. However, near cessation of blood flow into the aneurysm and parent artery on the postembolization angiography argued against further dense coil packing.
The timing of recanalization of parent artery remains unclear. Sawada et al.9) reported that parent artery recanalized at three and six months, respectively in their two cases. Meanwhile, Baik et al.1) found recanalization of parent artery at nine months after embolization. In the present case, we found recanalization of parent artery fourteen months after treatment. Possibly, the timing of parent artery recanalization may depend on extent of arterial wall injury, neointima proliferation and fibrous change of vascular wall during the healing process7). Furthermore, if all asymptomatic vertebral artery dissecting aneurysm patients without re-bleeing and follow-up angiography were clinically followed up, the true incidence of post-treatment recanalization may be slightly higher than we expected.
Recently, much interest has centered on reconstructive endovascular treatment with use of a stent for a intracranial dissecting aneurysm. In general, post treatment recurrence of vertebral artery dissecting aneurysm has been expected to occur less frequently after deconstructive treatment than after reconstructive treatment5). Contrary to the expectation, Kim et al.4) reported that the rate of post-treatment recurrence was not different between two treatment modalities. This study also showed promising results for the use of multiple overlapping stents in the treatment of vertebral artery dissecting aneurysm. However, if the false lumen cannot be separated from the true lumen, the stent can be placed in the false lumen. Therefore, more caution should be taken to use stent as a scaffold to enable coil embolization of a dissecting aneurysm.
Although our observation is limited to one case, the findings suggest that when the dissecting aneurysm is located proximal to the PICA without hypoplasia of the contralateral vertebral artery, internal trapping of the dissected site as well as proximal parent vertebral artery could be required to completely eliminate the risk of rebleeding.
Based on this unique case, the authors suggest that physicians should be alert to the fact that revascularization may occur even in cases successfully treated with endovascular occlusion of dissecting aneurysm and the affected artery. Careful angiographic follow-up of dissecting aneurysm is required. Furthermore, if the false lumen cannot be separated from the true lumen, treatment using a stent should be done with greater caution.
References
1. Baik SK, Kim YS, Lee HJ, Park J, Kang DS. Antegrade recanalization of parent artery in internal trapping of vertebral artery dissecting aneurysm : a case report. Surg Neurol. 2007; 68:108–111. discussion 111. PMID: 17586243.

2. Iihara K, Sakai N, Murao K, Sakai H, Higashi T, Kogure S, et al. Dissecting aneurysms of the vertebral artery : a management strategy. J Neurosurg. 2002; 97:259–267. PMID: 12186451.
3. Jin SC, Kwon DH, Choi CG, Ahn JS, Kwun BD. Endovascular strategies for vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2009; 30:1518–1523. PMID: 19474118.

4. Kim BM, Shin YS, Kim SH, Suh SH, Ihn YK, Kim DI, et al. Incidence and risk factors of recurrence after endovascular treatment of intracranial vertebrobasilar dissecting aneurysms. Stroke. 2011; 42:2425–2430. PMID: 21778439.

5. MacKay CI, Han PP, Albuquerque FC, McDougall CG. Recurrence of a vertebral artery dissecting pseudoaneurysm after successful stent-supported coil embolization : case report. Neurosurgery. 2003; 53:754–759. discussion 760-761. PMID: 12943592.
6. Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995; 36:905–911. discussion 912-913. PMID: 7791980.

7. Mizutani T, Kojima H, Asamoto S. Healing process for cerebral dissecting aneurysms presenting with subarachnoid hemorrhage. Neurosurgery. 2004; 54:342–347. discussion 347-348. PMID: 14744280.

8. Rabinov JD, Hellinger FR, Morris PP, Ogilvy CS, Putman CM. Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2003; 24:1421–1428. PMID: 12917140.
9. Sawada M, Kaku Y, Yoshimura S, Kawaguchi M, Matsuhisa T, Hirata T, et al. Antegrade recanalization of a completely embolized vertebral artery after endovascular treatment of a ruptured intracranial dissecting aneurysm. Report of two cases. J Neurosurg. 2005; 102:161–166. PMID: 15658109.

10. Sugiu K, Tokunaga K, Watanabe K, Sasahara W, Ono S, Tamiya T, et al. Emergent endovascular treatment of ruptured vertebral artery dissecting aneurysms. Neuroradiology. 2005; 47:158–164. PMID: 15703929.

Fig. 1
A 38-year-old male patient with dissecting aneurysm. A : CT angiography of right vertebral artery reveals fusiform dissecting aneurysm. B : Coronal CT source image shows low density intimal flap (arrow) and pseudoaneurysm. CT : computed tomography.
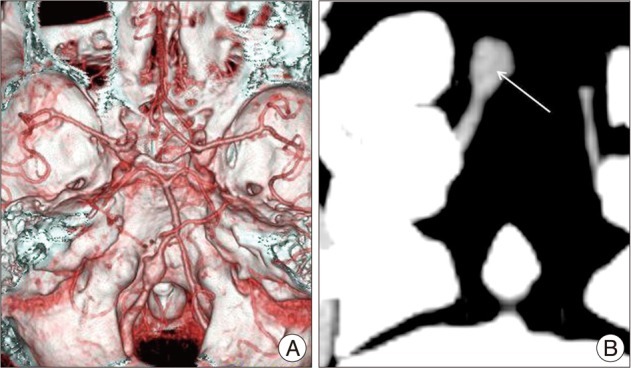
Fig. 2
Anteroposterior angiogram of the right vertebral artery shows a dissecting aneurysm arising from the right vertebral artery distal to origin of PICA. PICA : posterior inferior cerebellar artery.
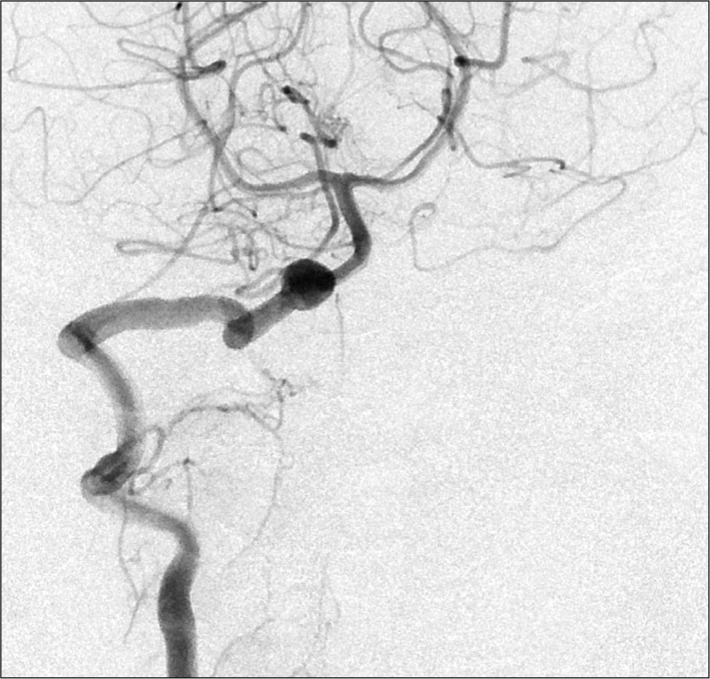
Fig. 3
A : The dissecting aneurysm and affected right vertebral artery are completely occluded, whereas the right PICA is preserved. B : Anteroposterior left VA angiogram obtained after embolization, depicting obliteration of the aneurysm. PICA : posterior inferior cerebellar artery, VA : vertebral artery.
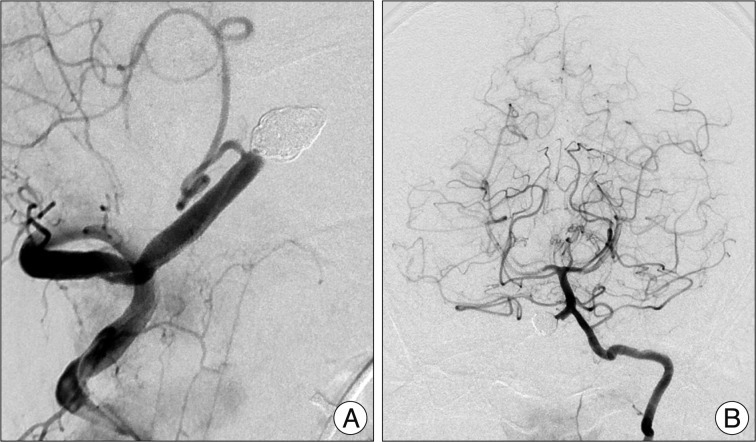
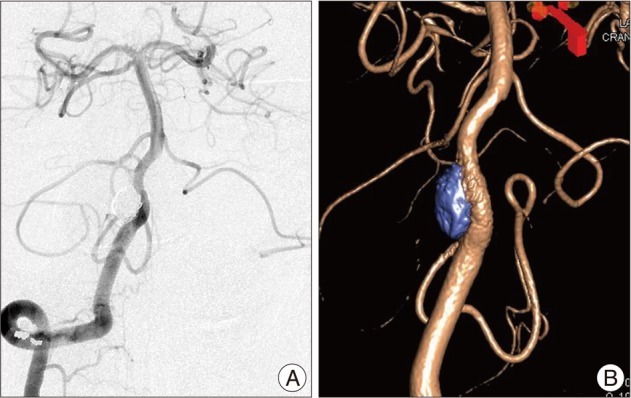
Fig. 4
A : Follow-up angiogram after 14 months reveals recanalization of the occluded right vertebral artery with a normal arterial configuration and antegrade flow into the basilar artery. B : The 3-dimensional reconstruction image shows recanalized vertebral artery which is located just inferior and medial to the deployed coil meshes.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download