This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
The anatomical knowledge is the most important and has a direct link with success of operation in cervical spine surgery. The authors measured various cervical parameters in cadaveric dry bones and compared with previous reported results.
Methods
We made 255 dry bones age from 19 to 72 years (mean, 42.3 years) that were obtained from 51 subjects in 100 subjects who donated their bodies. All measurements from C3-C7 levels were made using digital vernier calipers, standard goniometer, and self-made fix tool for two different cervical axes (canal and disc setting). We classified into 4 groups (uncinate process, vertebral body, lamina, and pedicle) and measured independently by two neurosurgeons for 28 parameters.
Results
We analyzed 23970 measurements by mean value and standard deviations. In comparing with previous literatures, there are some different results. The mean values for uncinate process (UP) width ranged from 5.5 mm at C4 and 5 to 6.3 mm at C3 and C7 in men. Also, in women, the mean values for UP width ranged from 5.5 mm at C5 to 6.3 mm at C7. C7 was widest and C5 was most narrow than other levels. The antero-posterior length of UP tended to increase gradually from C3 to C6. The tip way, tip distance, and base distance of UP also showed increasing pattern from C3 to C7.
Conclusion
These measurements can provide the spinal surgeons with a starting point to address bony architectures surrounding targeted soft tissues for safeguard against unintended damages during cervical operation.
Keywords: Cervical vertebra, Uncinate process, Dry bone, Parameters
INTRODUCTION
The definition of uncinate process (UP) is the bony protuberances that extends cranially from postero-lateral margins of superior end plates in lower cervical spine (C3-C7). In 1858, Luschka named as "eminentia costaria" due to resembled head of rudimentary rib, and Trolard named as "processus uncinatus" in 1893 and its function is to protect brachial plexus and to allow rotational movement
12). So far, anatomic studies for cervical UP were demonstrated by several investigators
6,
9,
11), the biomechanical role of cervical UP is both guiding mechanism during flexion and extension and a limiting mechanism during posterior translation and lateral bending
18).
Recently, anterior cervical microforaminotomy has been regarded as one of surgical methods, and UP is frequently removed during surgery. Therefore, the anatomical knowledge is 247the most important and has a direct link with success of operation in cervical spine surgery. For prevention of nerve roots and vertebral artery (VA) injuries, the surgeons must keep in mind of normal range and understand of the relationships between the neurovascular structures and bony surroundings. Authors measured various cervical parameters, especially for UP, in cadaveric dry bones and compared with previous reported results.
MATERIALS AND METHODS
Study population
A total of 100 individuals who donated their bodies to the Department of Anatomy were selected for appropriate study subjects. In 100 subjects, there are no information for age in 32 and severe cervical injuries in 11. So, we tried to make dry bones from 57 subjects. Fifty-seven subjects died with the cause of tumor, cerebral stroke, acute myocardial infarction, pneumonia, and etc. After making dry bone, we found that 6 subjects were exclusive status (cervical operation, severe degenerative change, vertebral body injuries, invasion of tumor, and loss of cervical level). Finally, 255 dry bones (32 male and 19 female) were obtained from 51 subjects.
Total of 51 subjects between the ages of 19 and 72 years (mean, 42.3 years) were categorized according to age and sex. We performed the measurements on 255 cervical dry vertebrae from the C3-C7 levels.
Instruments of measurement
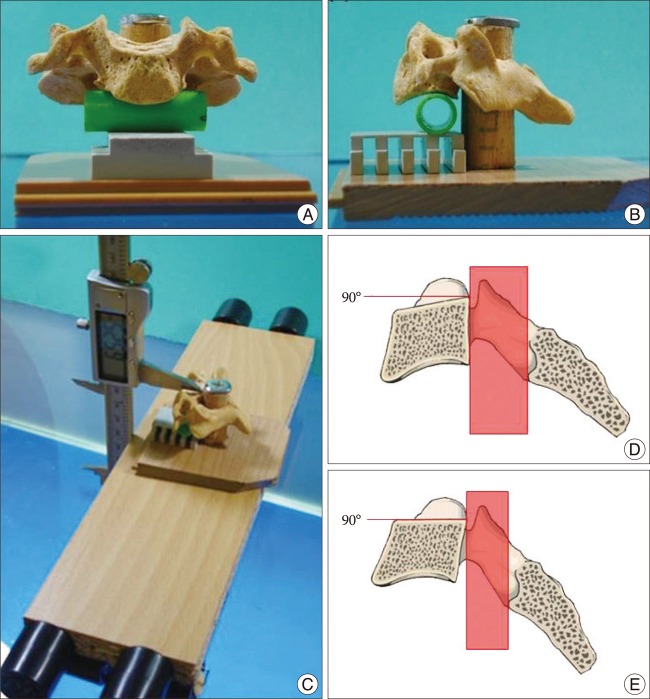
All measurements were made using digital vernier calipers which has accuracy to 0.01 mm and standard goniometer. We used self-made fix tool for cervical vertebrae measurements (
Fig. 1). Cervical vertebra has two different axes. One is canal setting and the other is disc setting. Canal setting is the state when imaginary longitudinal line made by posterior side of vertebral body (VB) is perpendicular to the ground (
Fig. 1D). Disc setting is the state when imaginary horizontal line made by superior side of VB (endplate) is parallel to the ground. Fix tool was able to support two kinds of axis (
Fig. 1E).
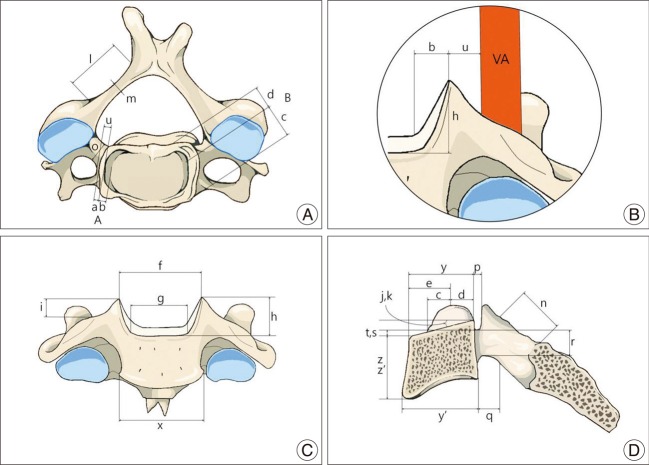
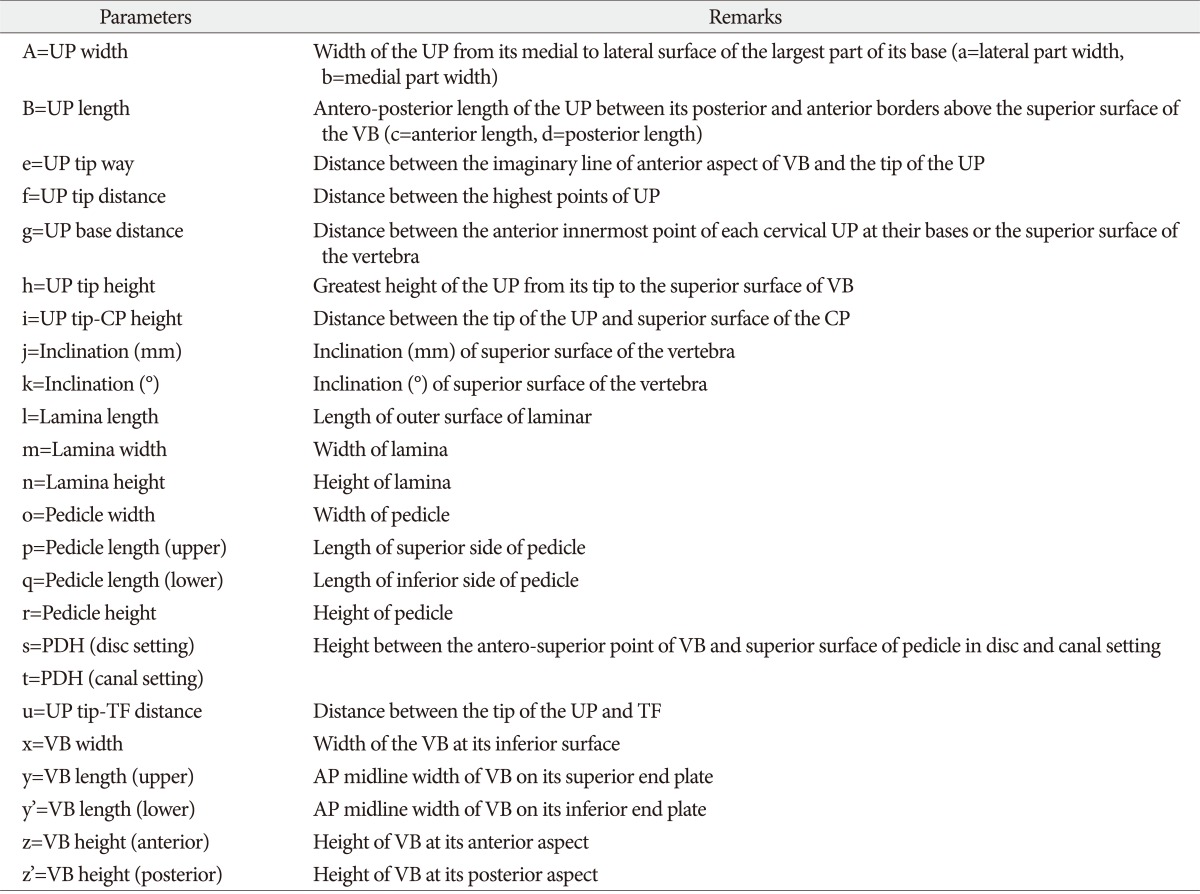
Parameters
We measured and classified into 4 groups which are UP, VB, lamina, and pedicle. The parameters of measurements from C3 to C7 were precisely performed. All measurements were checked independently by two neurosurgeons, and mean values were calculated. Total of 28 parameters (27 linear and 1 angular) for 255 vertebrae were used (
Table 1) (
Fig. 2). There were 19 paired and 9 unpaired parameters.
Statistical analysis
Analysis of total 23970 measurements (results from two neurosurgeons) was performed by mean value and standard deviations. The final table was made by the average of bilateral structures (right and left). The authors compared the data with the results in previous literatures.
RESULTS
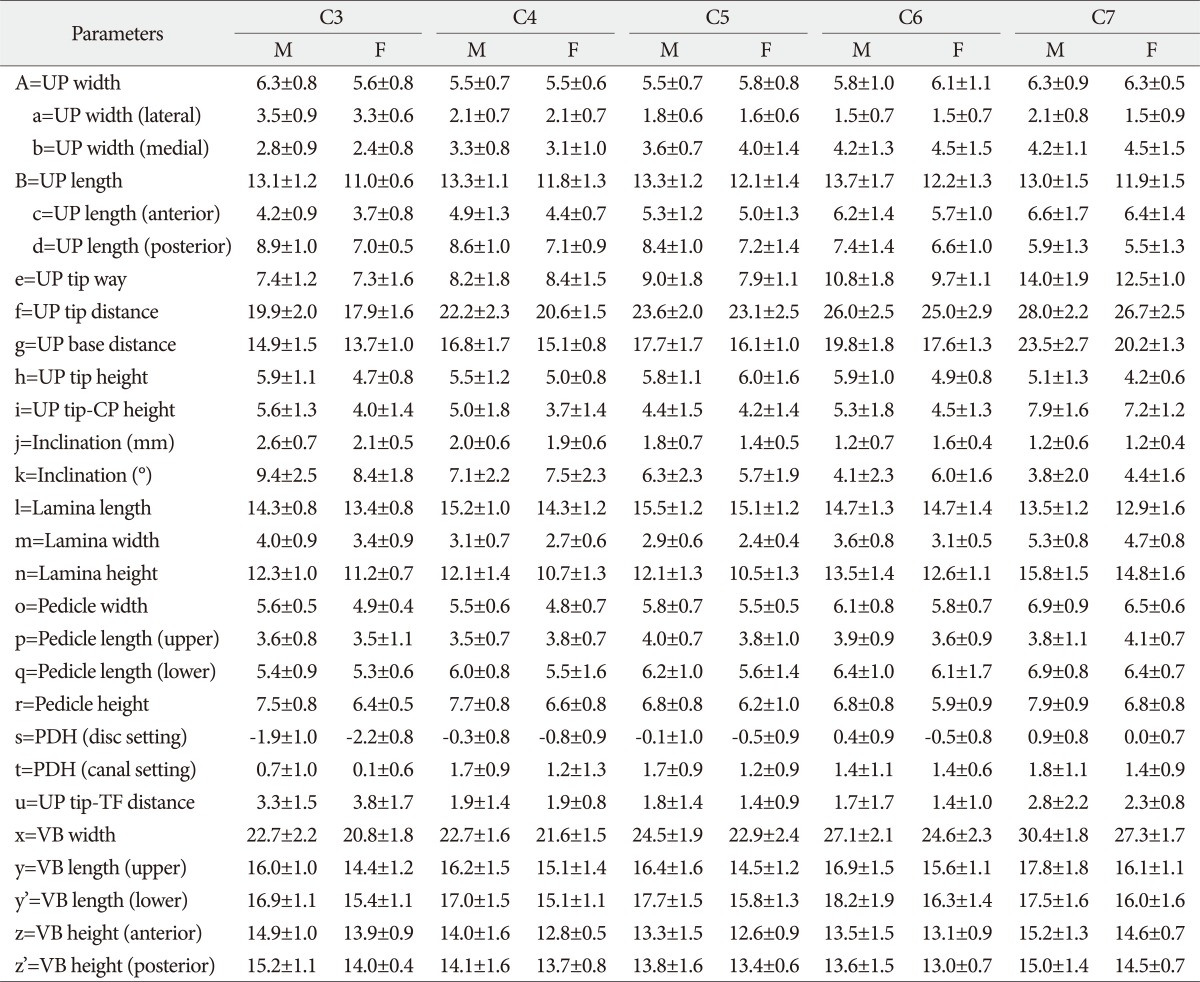
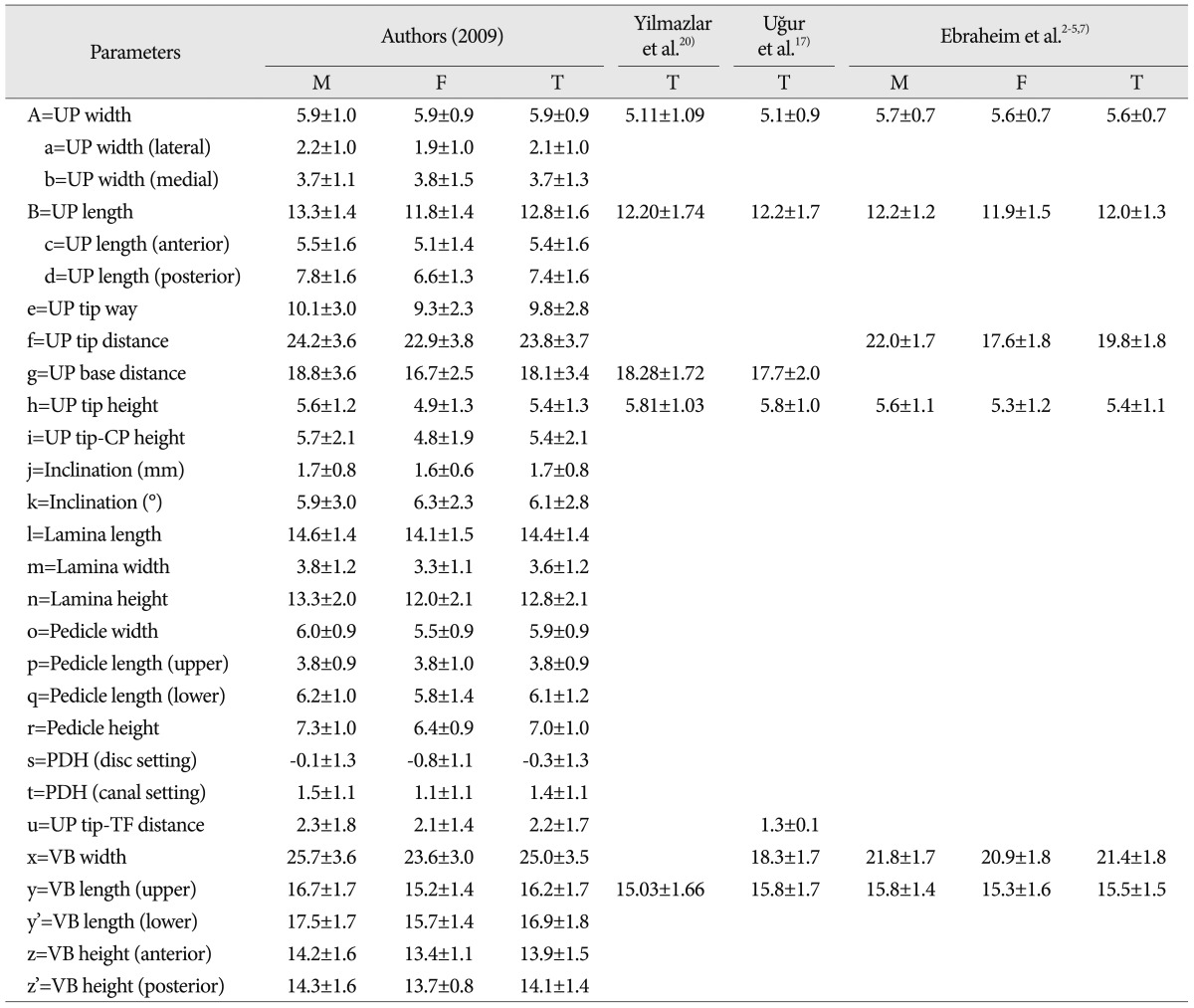
A total of 255 vertebrae obtained from 51 cervical spines were studied between the C3 and C7 levels. All symmetrical structures were measured bilaterally. The results of measurement for cervical parameters are shown in
Table 2 with the mean value and the standard deviation for linear and angular parameters.
The mean values for UP width ranged from 5.5 mm at C4 and 5 to 6.3 mm at C3 and C7 in men. Also, in women, the mean values for UP width ranged from 5.5 mm at C5 to 6.3 mm at C7. C7 was widest and C5 was narrower than other levels. The AP length of UP ranged 13.1 mm at C3, 13.3 mm at C4 and C5, 13.7 mm at C6, and 13.0 mm at C7 in men. In women, it ranged 11.0 mm at C3 and 12.2 mm at C6. Thus, they tended to increase gradually from C3 to C6. The tip way, tip distance, and base distance of UP also showed increasing pattern from C3 to C7. The UP height ranged from 5.9 mm at C3 to 5.1 mm at C7 in men and from 6.0 mm at C5 to 4.2 mm at C7 in women. There was no increasing pattern in height and C5 was highest than other levels. Not unexpectedly, the inclination tended to decrease gradually from C3 to C7.
There were no increasing patterns in lamina parameters. C5 lamina was longest in length, narrowest in width, and lowest in height than other levels. The width and lower length of pedicle showed increasing pattern from C3 to C7. But upper pedicle length had a similar value in 5 cervical vertebrae. The pedicle-disc height (PDH) were within 1 mm at C3 in canal setting (0.1-0.7 mm) and at C4-C7 in disc setting (0.0-0.9 mm). The distance of UP tip and transverse foramen (TF) was narrowest at C4, C5 and C6.
The parameters of VB showed gradual increasing pattern in width, length, and posterior height. But in anterior height, C5 was lowest than other levels.
DISCUSSION
According to our study result, the mean values for UP width ranged from 5.5 mm at C4 and 5 to 6.3 mm at C3 and C7. In 1996, Ebraheim et al.
3) reported that C5 is widest level, and this may be originated from the clinical occurrence of cervical spondylosis due to excessive cervical segmental motion
3,
8). In our subject, C7 was widest and C5 was narrower than other levels. The AP length of UP tended to increase gradually from C3 to C6. And the tip way, tip distance, and base distance of UP also showed increasing pattern from C3 to C7. These patterns were similar with previous studies
2,
3). However, the UP height showed no increasing pattern in height, and C5 was highest than other levels. Ebraheim et al. reported that C6 was highest level in UP height
1) and Yilmazlar et al.
20) reported that C7 was highest level. We thought that it might have caused from different measuring method (disc or canal setting), ethnic character, and etc.
The PDH was within 1 mm at C3 in canal setting (0.1-0.7 mm) and at C4-C7 in disc setting (0.0-0.9 mm). So, antero-superior point of VB and superior pedicle surface can be considered as nearly same height. The distance of UP tip and TF was narrowest at C4, C5 and C6 (1.4 and 1.7 mm). Ebraheim et al.
2) reported that the UP tip-TF distance showed decreasing pattern from C3 to C4 (1.2 and 1.6 mm) and increasing from C4 to C7. In that study, they used calculation formula instead of direct measuring as following; (TF medial border distance-interuncinate distance)/2. Pait et al.
10) reported that the distance from the tip of UP to VA averaged 0.8 mm at C2-C3 and 1.6 mm at C4-C5 in cadaver. In view of the results so far achieved, when UP is recognized, we must remember that the VA is within about 1-2 mm from the lateral border of UP. In a review of 10 cases of VA injury, Smith et al.
15) found that the use of a high-powered drill was the most frequent cause of VA injury.
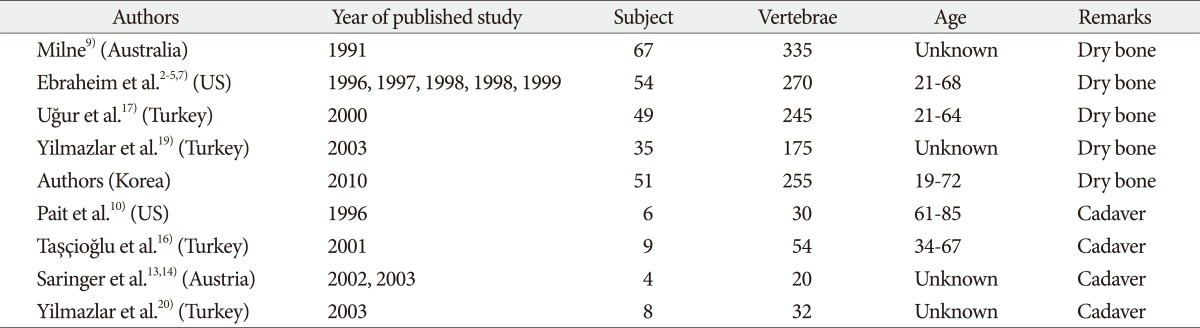
There are some literatures about measurement for cervical UP and VB using dry bone (
Table 3). We selected 3 literatures used dry bone, and compared with our results (
Table 4). We averaged all the values from C3 to C7, and compared with those of previous reports. Eight parameters are comparable among 28 parameters, and 3 parameters showed a difference above the standard deviation. The UP tip distance, the UP-TF distance, and the VB width were slightly wide in our result. Other parameters showed similar figures and within the standard deviation.
The authors started this study because there were only few data of oriental cadaveric measurements for cervical vertebra, although increasing of cervical operation. We introduced the concept of disc and canal setting. This is important that without these setting, the more parameters are measured, the more the error is increased. We had interest in the PDH values, because anterior cervical disc height and upper pedicle height are nearly same level, unlikely lumbar and thoracic vertebra. We would like to emphasis that various parameters and methods for cervical measuring, along with results of measurement.
These measurements can provide the spinal surgeons with a starting point to address bony architectures surrounding targeted soft tissues. The spinal surgeon must have a complete understanding of the hidden vascular and bony anatomy and knowledge of the changes during discectomy in anterior cervical spine surgery. Although avoiding unfortunate injury is not always possible, being well-informed with the location and relations among the anatomic features is the only safeguard against unintended damages during cervical operation.
CONCLUSION
The authors measured various cervical parameters with dry bones from donated subjects, and reported the result. There were some different results with previous literatures. These measurements could help spinal surgeon to success in cervical operation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download