Abstract
Osteochondroma is a rare condition in the spine that may be indolent due to its slow growth. The authors present a case of 32-year-old man with subclinical osteochondroma in the cervical spine presenting as Brown-Sequard syndrome after trivial neck trauma. After resection of the tumor through hemilaminectomy, his symptoms were improved with mild residual sequelae.
Osteochondroma accounts for more than one-third of all benign bone tumors in adolescents. Solitary osteochondroma of the spine is a rare manifestation14). It presents as a painless mass and sometimes causes neurological dysfunction if the tumor involves the spinal canal7,13). Since the tumor has a slowly-growing nature, the clinical symptoms may be indolent or unrecognized until significant spinal cord compression develops. However, these slow growing space occupying lesions in the spinal canal can be a aggravating factors when minor spinal injury occurs. The authors present a case of osteochondroma in the cervical spinal canal which had no symptom and presented as Brown-Sequard syndrome after trivial neck trauma.
A 32-year-old car mechanic without any previous medical problems was transported to emergency department. He was inebriated to a state of stupor. His friend stated that he stumbled and fell down some stairs but it was not a serious accident. After he became sober with fluid infusion, he found himself left hemiparetic and felt numbness of his right leg. On precise neurological examination, he showed muscle weakness below the C4 myotome only in his left upper and lower extremities (muscle power grade : 4 in the shoulder, 1 in the elbow, wrist and fingers, 3 during hip flexion extension, 1 in the area below the knee joint). His pain sensation decreased below the T4 dermatome only on the right side, while tactile and vibration sensations decreased only on the left side. His neurologic status was exactly compatible with Brown-Sequard syndrome. We could not identify specific bony abnormalities on plain X-rays but were able to find a subtle sclerotic lesion on the C4-5 facet area on retrospective review (Fig. 1). Computed tomography (CT) of the cervical spine revealed an exophytic bony mass from the inside and outside of the lamina. The C4-5 facet protruded into the spinal canal which was causing spinal cord compression (Fig. 2). Emergency magnetic resonance (MR) imaging was performed, which showed signal changes in the spinal cord at the C4-5 level on T2-weighted images (Fig. 3). As the cord compression seemed to be imminent, the patient underwent an emergency operation.
The patient was positioned prone under general anesthesia. After dissection of muscles on the left side of the spinous process,
the left side of the C4-5 lamina was exposed. The left side of the C4-5 lamina had a hyperostotic change and the spinal cord was severely compressed. We performed partial hemilaminectomy
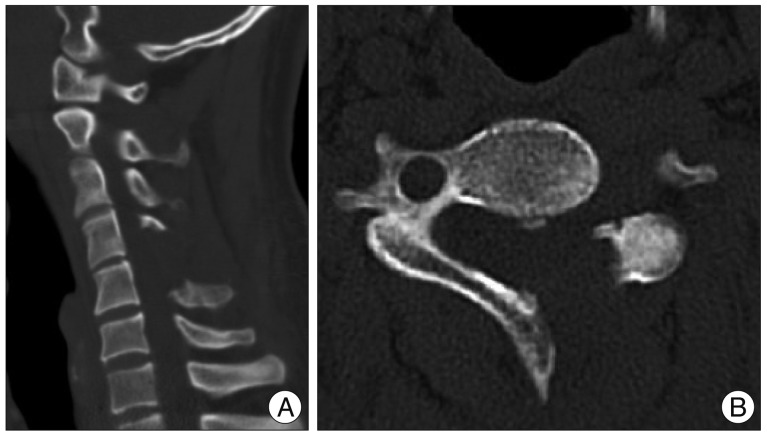
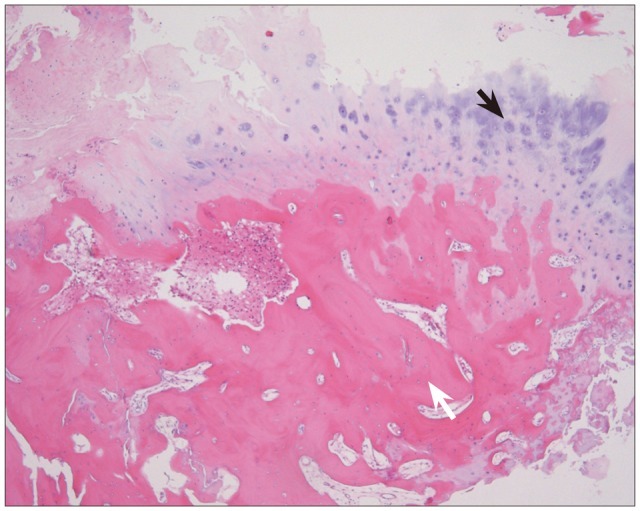
and removed the exophytic bony lesion. Pathogenic tissue was sent to pathology department for definite diagnosis. After confirmation of a fully decompressed dural sac, the wound was closed layer by layer without any instrumentation. The main pathologic findings were cartilaginous cap and underlying bony stalk. Postoperative CT image showed remaval of exophytic bony lesion (Fig. 4). The cellular architectures were not different with normal bone tissue. The abnormality of bony tissue with cartilaginous cap in aberrant location was compatible with osteochondroma (Fig. 5).
After the operation, the patient's motor weakness improved gradually (muscle power grade : 5 in the shoulder, 4 in the elbow, wrist and hand, 5 in the hip, 4 in the area below the knee joint). The sensory deficit improved to 8/10 during the follow-up. The patient could walk without any assistance and returned to his previous job.
His mild subjective sensory and motor deficits which were the same patterns as Brown-Sequard syndrome was sustained during follow-up. MR images checked at the outpatient clinic showed a complete decompression of the spinal cord. On the axial images, cord signal changes were improved on the right side of the cord but showed myelomalacia on the left one-third of the cord (Fig. 6). There was no recurrence and stability was maintained during the last 1.5-year of follow-up.
Osteochondroma is the most common bone tumor and accounts for about 8.5% of all bone tumors and for 36-40% of all benign tumors9,15). The spinal involvement rate of a solitary osteochondroma is reported to be 1-4%, half of which arise in the cervical spine11). Multiple lesions are considered to be associated with hereditary multiple exostosis, an autosomal dominant condition6,10). While a few cases of solitary osteochondromas arise in the spine, spinal involvement is seen in many cases of hereditary multiple exostosis1,9). Unfortunately, it was difficult to identify a familial history of osteochondroma in current case because his family could not be contacted.
Most patients present their symptoms at the age of 20 or younger5,6,12). It is noticeable that patients had no symptoms until the age of 32 before trauma even though the marked cord compression by extradural mass seems to be very imminent. We sometimes encounter the characteristic cases that slowly growing benign space-occupying lesions in the spinal canal are asymptomatic or presents as minor symptoms even though the lesion is considerably occupying the spinal canal. Similar to our case, Yukawa et al.15) have reported a few cases of silent osteochondroma showing neurological deficits after trivial trauma. Three cases of osteochondroma presenting with the symptoms in patients over 70 years old have been reported14).
Osteochondroma commonly presents as a painless mass because tumors usually arise from the posterior column as a secondary ossification center and grows to outside the spinal canal12,14). The tumor was formed by abnormal periphysial ectopic enchondral ossification and originates from cartilage or bone. It is an extension of the bone with a cap of cartilage, commonly near tip of spinous or transverse processes2,4,9).
Brown-Sequard syndrome, first reported by Brown and Sequard in 1846, is characterized by ipsilateral loss of motor function, proprioception and vibratory sense, combined with spinothalamic tract dysfunction resulting in contralateral loss of pain and temperature sensation3). Brown-Sequard syndrome is observed most frequently in association with penetrating injuries to the spinal cord or intradural extramedullary spinal tumors8). The cervical hyperflexion or hyperextension injury usually tends to cause central cord syndrome especially in cervical stenosis due to degenerative osteophyte or ossification of longitudinal ligament. If the degree of injury is severe, complete cord injury may occurs. The Brown-Sequard syndrome which is a unique pattern of incomplete spinal cord injury is actually infrequent in usual spinal trauma. This syndrome may be elicited by cervical injury only when there's a unilaterally occupying lesion in the spinal canal.
The most reliable diagnostic tools for osteochondroma are MR imaging and CT. Plain radiographs may show the bony projections of exostosis but do not outline the cartilaginous cap15). Therefore, bony abnormalities may not be identified on plain radiographs. On the other hand, CT scans show definite margins to the osseous and cartilaginous components of the tumor and sessile or pedunculated masses with cortex and marrow elements connecting with the bone of origin12). Our case showed bony hypertrophy and osseous components in the left C4-5 lamina and facet on CT images. MR imaging is useful for showing the level and extent of neural compression, as well as marrow content and cartilaginous cap. Our case showed high signal intensity in the C4-5 spinal cord on T2-weighted images. MR imaging and CT have their own advantages in preoperative assessment15). In the literature, most patients have complete disappearance of their deficits or have only minor residual deficits after surgical decompression9). Surgical resection of the lesion is the definite treatment modality. It is recommended that cartilaginous cap should be removed in order to prevent tumor recurrence.
When the lesion located unilaterally, removal of lesion through the unilateral hemilaminectomy has obvious benefits of preserving osseo-ligamentous structure at the midline and contralateral muscle structure, which leads better functional outcomes of spinal column. The risk of recurrence after a complete resection is less than 2%12).
Osteochondroma in the spinal canal is a rare but may be subclinical due to its slow growth. This indolent osteochondroma located unilaterally in the cervical spine presented as typical Brown-Sequard syndrome after trivial neck trauma. Emergency decompression and resection of the tumor improved the patient's neurologic symptoms.
References
1. Akagi S, Hashiguchi J, Sasai K, Kato I, Saito T, Ogawa R. Osteochondroma of the upper cervical spine presenting as vertigo. Orthopedics. 2003; 26:187–188. PMID: 12597225.

2. Chatzidakis E, Lypiridis S, Kazdaglis G, Chatzikonstadinou K, Papatheodorou G. A rare case of solitary osteochondroma of the dens of the C2 vertebra. Acta Neurochir (Wien). 2007; 149:637–638. PMID: 17450439.

3. Cheng WY, Shen CC, Wen MC. Ganglion cyst of the cervical spine presenting with Brown-Sequard syndrome. J Clin Neurosci. 2006; 13:1041–1045. PMID: 17113987.

4. Cirak B, Karabulut N, Palaoglu S. Cervical osteochondroma as a cause of spinal cord compression in a patient with hereditary multiple exostoses : computed tomography and magnetic resonance imaging findings. Australas Radiol. 2002; 46:309–311. PMID: 12196244.

5. Grivas TB, Polyzois VD, Xarchas K, Liapi G, Korres D. Seventh cervical vertebral body solitary osteochondroma. Report of a case and review of the literature. Eur Spine J. 2005; 14:795–798. PMID: 15912348.

6. Han IH, Kuh SU. Cervical osteochondroma presenting as brown-sequard syndrome in a child with hereditary multiple exostosis. J Korean Neurosurg Soc. 2009; 45:309–311. PMID: 19516952.

7. Kim WJ, Kim KJ, Lee SK, Choy WS. Solitary pelvic osteochondroma causing L5 nerve root compression. Orthopedics. 2009; 32:922. PMID: 19968229.

8. Kim YS, Lee JK, Joo SP, Kim SH. Brown sequard syndrome resulting from cervical disc herniation treated by anterior foraminotomy. J Korean Neurosurg Soc. 2005; 38:136–140.
9. Maheshwari AV, Jain AK, Dhammi IK. Osteochondroma of C7 vertebra presenting as compressive myelopathy in a patient with nonhereditary (nonfamilial/sporadic) multiple exostoses. Arch Orthop Trauma Surg. 2006; 126:654–659. PMID: 16906423.

10. Roach JW. Hereditary multiple exostoses with spine involvement in a 4-year-old boy. Am J Med Genet A. 2010; 152A:1263. PMID: 20425832.

11. Sakai D, Mochida J, Toh E, Nomura T. Spinal osteochondromas in middle-aged to elderly patients. Spine (Phila Pa 1976). 2002; 27:E503–E506. PMID: 12461407.

12. Schomacher M, Suess O, Kombos T. Osteochondromas of the cervical spine in atypical location. Acta Neurochir (Wien). 2009; 151:629–633. discussion 633. PMID: 19290470.

13. Xu J, Xu CR, Wu H, Pan HL, Tian J. Osteochondroma in the lumbar intraspinal canal causing nerve root compression. Orthopedics. 2009; 32:133. PMID: 19301786.

14. Yagi M, Ninomiya K, Kihara M, Horiuchi Y. Symptomatic osteochondroma of the spine in elderly patients. Report of 3 cases. J Neurosurg Spine. 2009; 11:64–70. PMID: 19569943.
15. Yukawa Y, Kato F, Sugiura H. Solitary osteochondroma of the lower cervical spine. Orthopedics. 2001; 24:292–293. PMID: 11300298.

Fig. 2
Preoperative CT sagittal (A) and axial (B) images reveal an exophytic osseous mass in the C4-5 lamina and some part of the facet.
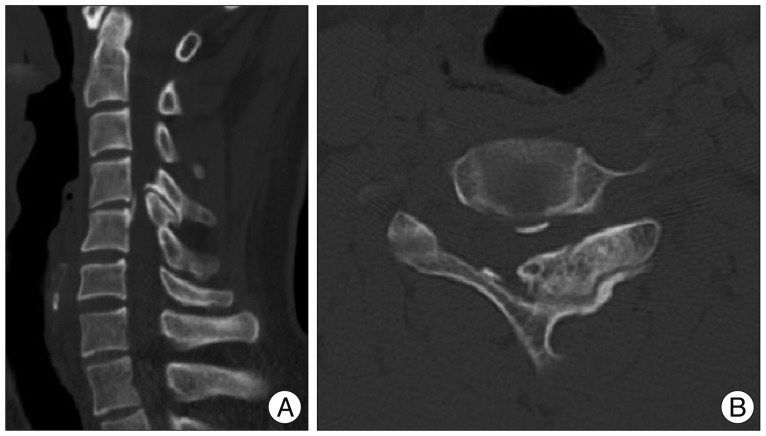
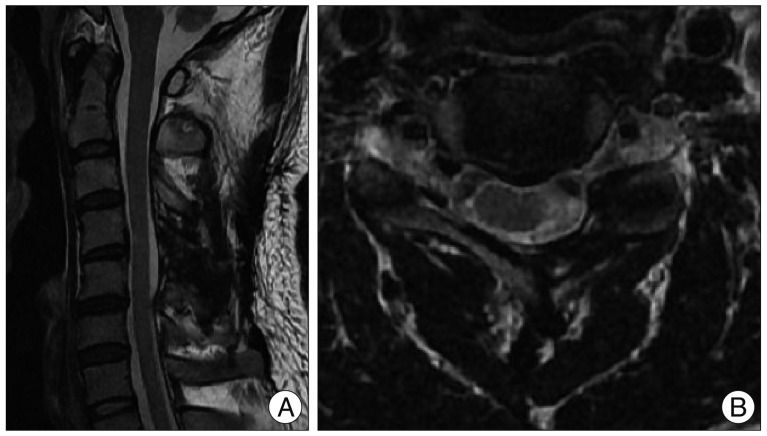
Fig. 3
Preoperative magnetic resonance T2 sagittal (A) and axial (B) images. The compression of the cord by an extradural mass seems to be imminent. The signal change of the cord is noticed.
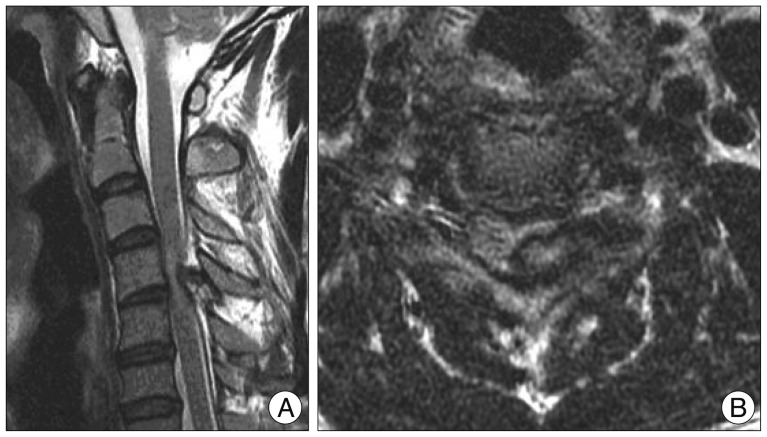
Fig. 4
Postoperative CT sagittal (A) and axial (B) images. The exophytic osseous lesion was removed through the hemilaminectomy.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download