Abstract
Objective
Percutaneous vertebroplasty (PVP) is usually carried out under three-dimensional (2D) fluoroscopic guidance. However, operative complications or bone cement distribution might be difficult to assess on the basis of only 2D radiographic projection images. We evaluated the feasibility of performing an intraoperative and postoperative examination in patients undergoing PVP by using three-dimensional (3D) reconstructive C-arm.
Methods
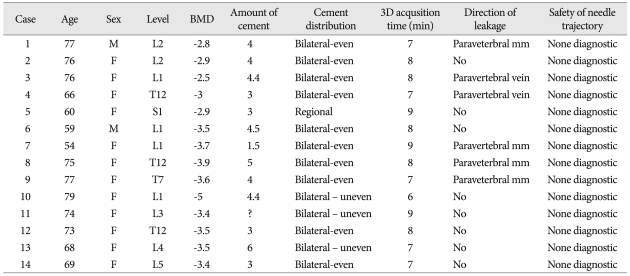
Standard PVP procedures were performed on 14 consecutive patients by using a Siremobil Iso-C3D and a multidetector computed tomography machine. Post-processing of acquired volumetric datasets included multiplanar reconstruction (MPR) and surface shaded display (SSD). We analyzed intraoperative and immediate postoperative evaluation of the needle trajectory and bone cement distribution.
Results
The male : female ratio was 2 : 12; mean age of patients, 70 (range, 77-54) years; and mean T score, -3.4. The mean operation time was 52.14 min, but the time required to perform and post-process the rotational acquisitions was 7.76 min. The detection of bone cement distribution and leakage after PVP by using MPR and SSD was possible in all patients. However, detection of the safe trajectory for needle insertion was not possible.
Percutaneous vertebroplasty (PVP) was developed by Galibert and Deramond in 1987, and it involves the injection of bone cement (polymethylmethacrylate; PMMA) into a collapsed vertebral body6). The main indications have been extended to the treatment of painful osteoporotic compression fractures, vertebral myeloma, and metastases13,18).
In many centers, all phases of the PVP procedure are usually performed under two-dimensional (2D) fluoroscopic guidance. However, the operative complications, e.g., cement extravasation into critical structures such as veins at the vertebral foramen, or bone cement distribution might be difficult to assess on the basis of only 2D radiographic projection images.
Computed tomography (CT) in combination with fluoroscopy-guided PVP was first described by Gangi et al.7) in a series of 10 patients. CT in combination with fluoroscopy during vertebroplasty provides excellent imaging and enables exact positioning of the vertebroplasty needle. Further, this technique facilitates optimal filling of the vertebral body because of detailed localization of the injected bone cement. Furthermore, potential bone cement leakages can be detected, especially cement leakage into smaller veins. However, CT in combination with fluoroscopy-guided PVP has some shortcomings : this technique requires expensive equipment and a large space, and it is difficult to maintain aseptic conditions during the procedure.
In vascular intervention, rotational image acquisition with a C-arm fluoroscopy unit is an established method. With the introduction of rotational image acquisition, it became possible to acquire high-resolution three-dimensional (3D) angiographic images5,11). However, in vertebroplasty, this technique is not used. We evaluated the feasibility of performing standard PVP procedures by using 3D rotational acquisitions by Siremobil Iso-C3D (Siemens Medical Solutions, Erlangen, Germany).
Fourteen consecutive patients (women, 12; men, 2; mean age, 70 years; age range, 54-77 years) in whom transpedicular PVP procedures were performed using a Siremobil Iso-C3D for intraoperative procedural control were studied. The indications for PVP were metastasis (n=1) and osteoporotic compression fractures (n=13). The total number of vertebrae controlled with 3D acquisitions and CT was 15 (thoracic, 5; lumbar, 9; sacral, 1) (Table 1). In all patients, we initially performed vertebroplasty by unilateral transpedicular approach and total twice single rotational acquisition was performed at after needle and PMMA insertion. If the injected cement was not evenly distributed, we performed transpedicular approach at contralateral side. This acquisition was focused on the region where visualization of needle trajectory, bone cement distribution, and leakage was of the most interest.
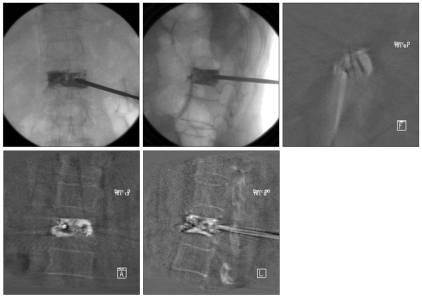
3D rotational images were acquired immediately after needle insertion and PMMA injection, with the patient remaining in the prone position (lumbar and thoracic spine) on the table. Patients who were awake were asked to hold their breath during image acquisition. Images were acquired using a Siremobil Iso-C3D (Siemens Medical Solutions, Erlangen, Germany) that allows creation of 3D anatomical images, with the anatomy to be imaged positioned in the system isocenter. The rotational scan covers 190 degrees of the circular trajectory and is accomplished in 30 seconds with 50 images per scan. The field of view could be chosen from 17 to 38 with a matrix of 1024×1024. To obtain images optimized for bone display, a dedicated acquisition system program ("bone run") was selected. The images from rotational acquisition were transferred to the commercially available post-processing station through a conventional network connection. To transfer 254 images, 5-6 seconds were required. The reconstructed data set was visualized using different display techniques such as multiplanar reformat and shaded surface display. With these display techniques, it was possible either to display a 3D model of the entire volume or to analyze image slabs in 3 perpendicular views with the ability to cross-reference the images (Fig. 1).
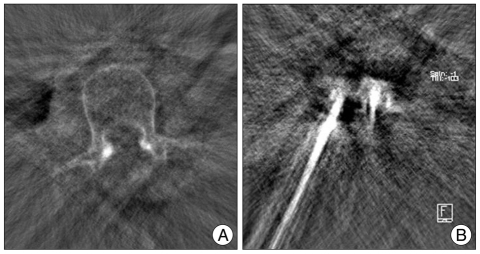
Two independent observers, blinded to any other information relating to the subjects, measured the distribution and leakage of cement and safety of needle trajectory (Fig. 2). We grouped the cement distribution (regional, focal distribution of cement; unilateral, unilateral distribution of cement; bilateral - uneven, bilateral distribution of cement but separated mass; bilateral-even, bilateral single mass of cement) and the presence of cement leakage (posterior to the vertebra, paravertebral; anterior or lateral to the vertebral body, foraminal, and in the region of the vessels).
On average, 1.07 vertebrae were treated per patient. In all cases, the time from rotational image acquisition to visualization of 3D volume images was less than 10 minutes. There was 1 vertebra in the regional group, 3 vertebrae in the bilateral - uneven group, and 11 vertebrae in the bilateral-even group. The 6 cases of regional or unilateral distribution of bone cement during operation received additional bone cement injection, but in 3 of 6 cases, a continuous-bivertebrate distribution could not be achieved. On reconstructive images, leakage was found in 6 (40%) of 15 vertebrae, with localization in the paravertebral muscular area [4 (26.7%) vertebrae] and vascular leakage [2 (13.3%) vertebrae]. Clinical symptoms caused by the paravertebral leakage were not observed in any patient. Because of severe needle artifacts and lower resolution of the device, the safety of needle trajectory could not be confirmed in any patient (Table 1) (Fig. 2).
PVP is a procedure that entails a percutaneous injection of PMMA, or cement, into a diseased vertebra12,14). There was some debate regarding PVP. Osteoporosis and osteoporotic vertebral body fractures affect not only 1 part of the vertebral body but also the entire vertebral body. Therefore, it is important to stabilize the whole vertebral body. Uneven distribution of bone cement in the vertebral body involves the risk of additional instability and concomitant danger of adjacent vertebral fractures. Therefore, even cement distribution is important for the long-term stability and good outcome of the compressed vertebral body.
Complications in percutaneous vertebroplasty can be divided into technical complications and bone cement-induced complications. Bone cement leakage is a common finding after PVP2,8) and is usually asymptomatic. The visualization provided by 2D fluoroscopy images is sufficient to control clinically significant cement leakages occurring after the PVP procedure. However, it can be difficult to exactly localize cement leakage on only 2D fluoroscopic images. If cement leakage to critical anatomic structures such as the neural foramen or posterior epidural space is suspected, it is important to have exact imaging information for performing further workup and administering appropriate treatment to the patient2,7,9,20). Furthermore, immediate availability of the 3D image data set after the cement injection (while the patient is still on the operating table) by using the same X-ray equipment facilitates 1) earlier and exact detection of a complication, 2) the therapeutic decision process, and 3) initiation of protective procedures. In our study, we could early and exact detect the leakage and uneven distribution of the bone cement and perform the rapid therapeutic and protective procedure for bone cement associated complication. However, the rate of bone cement leakage of this study was 40%, which was not significantly higher than that in previously reported data (range, 8-87.5%)4,10,15,16,19,23,24). Therefore, this 3D image CT guidance vertebroplasty technique seems to be of relatively helpful to detection and protection of bone cement associated complication.
Technical complications are rare and have been reported in less than 1% of the treated patients1,10,16,19,21,22,24). One of the major technical complications is a neural injury due to violation of the pedicle wall by the needle. Obtaining volumetric images immediately after an intervention is the key advantage of rotational acquisitions as compared with CT imaging. However, the resolution of the rotational images was clearly inferior as compared to that of CT images. The outlines of bones and the margin of the injection needle could be less distinctly detected using Siremobil Iso-C3D. Because of the lower resolution on rotational images, as reported previously3,17), the safe trajectory for needle insertion could not be detected in all of our cases. Eventually, 3D image CT guidance vertebroplasty technique would be helpful in complicated patients who need to exact insertion of the bone cement such as vertebra plana or need to be operated under the general anesthesia.
Our preliminary experiences indicate that 3D rotational image acquisition can be of relatively helpful to intra- or post-procedural assessment of the vertebroplasty procedure and detection of bone cement distribution and leakage. However, we could not significantly reduced the cement leakage rate and it was difficult to assess the safe trajectory for needle insertion.
References
1. Alvarez L, Pérez-Higueras A, Quiñones D, Calvo E, Rossi RE. Vertebroplasty in the treatment of vertebral tumors : postprocedural outcome and quality of life. Eur Spine J. 2003; 12:356–360. PMID: 12687441.

2. Cotten A, Dewatre F, Cortet B, Assaker R, Leblond D, Duquesnoy B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma : effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996; 200:525–530. PMID: 8685351.

3. El-Sheik M, Heverhagen JT, Alfke H, Froelich JJ, Hornegger J, Brunner T, et al. Multiplanar reconstructions and three-dimensional imaging (computed rotational osteography) of complex fractures by using a C-arm system : initial results. Radiology. 2001; 221:843–849. PMID: 11719688.

4. Evans AJ, Jensen ME, Kip KE, DeNardo AJ, Lawler GJ, Negin GA, et al. Vertebral compression fractures : pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology. 2003; 226:366–372. PMID: 12563127.

5. Gailloud P, Oishi S, Carpenter J, Murphy KJ. Three-dimensional digital angiography : new tool for simultaneous three-dimensional rendering of vascular and osseous information during rotational angiography. AJNR Am J Neuroradiol. 2004; 25:571–573. PMID: 15090343.
6. Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie. 1987; 33:166–168. PMID: 3600949.
7. Gangi A, Kastler BA, Dietemann JL. Percutaneous vertebroplasty guided by a combination of CT and fluoroscopy. AJNR Am J Neuroradiol. 1994; 15:83–86. PMID: 8141070.
8. Garfin SR, Yuan HA, Reiley MA. New technologies in spine : kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976). 2001; 26:1511–1515. PMID: 11462078.
9. Harrington KD. Major neurological complications following percutaneous vertebroplasty with polymethylmethacrylate : a case report. J Bone Joint Surg Am. 2001; 83-A:1070–1073. PMID: 11451978.
10. Heini PF, Wälchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA : operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000; 9:445–450. PMID: 11057541.

11. Hochmuth A, Spetzger U, Schumacher M. Comparison of three-dimensional rotational angiography with digital subtraction angiography in the assessment of ruptured cerebral aneurysms. AJNR Am J Neuroradiol. 2002; 23:1199–1205. PMID: 12169480.
12. Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures : technical aspects. AJNR Am J Neuroradiol. 1997; 18:1897–1904. PMID: 9403451.
14. Kim AK, Jensen ME, Dion JE, Schweickert PA, Kaufmann TJ, Kallmes DF. Unilateral transpedicular percutaneous vertebroplasty : initial experience. Radiology. 2002; 222:737–741. PMID: 11867793.

15. Kobayashi K, Shimoyama K, Nakamura K, Murata K. Percutaneous vertebroplasty immediately relieves pain of osteoporotic vertebral compression fractures and prevents prolonged immobilization of patients. Eur Radiol. 2005; 15:360–367. PMID: 15662480.

16. Legroux-Gérot I, Lormeau C, Boutry N, Cotten A, Duquesnoy B, Cortet B. Long-term follow-up of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Clin Rheumatol. 2004; 23:310–317. PMID: 15293091.

17. Linsenmaier U, Rock C, Euler E, Wirth S, Brandl R, Kotsianos D, et al. Three-dimensional CT with a modified C-arm image intensifier : feasibility. Radiology. 2002; 224:286–292. PMID: 12091697.

18. Martin JB, Jean B, Sugiu K, San Millán Ruíz D, Piotin M, Murphy K, et al. Vertebroplasty : clinical experience and follow-up results. Bone. 1999; 25:11S–15S. PMID: 10458267.
19. Martin JB, Wetzel SG, Seium Y, Dietrich PY, Somon T, Gailloud P, et al. Percutaneous vertebroplasty in metastatic disease : transpedicular access and treatment of lysed pedicles--initial experience. Radiology. 2003; 229:593–597. PMID: 14595155.

20. Mathis JM, Barr JD, Belkoff SM, Barr MS, Jensen ME, Deramond H. Percutaneous vertebroplasty : a developing standard of care for vertebral compression fractures. AJNR Am J Neuroradiol. 2001; 22:373–381. PMID: 11156786.
21. Peh WC, Gilula LA, Peck DD. Percutaneous vertebroplasty for severe osteoporotic vertebral body compression fractures. Radiology. 2002; 223:121–126. PMID: 11930056.

22. Pérez-Higueras A, Alvarez L, Rossi RE, Quiñones D, Al-Assir I. Percutaneous vertebroplasty : long-term clinical and radiological outcome. Neuroradiology. 2002; 44:950–954. PMID: 12428134.
23. Winking M, Stahl JP, Oertel M, Schnettler R, Böker DK. [Polymethylmethacrylate-vertebroplasty. A new and effective method of pain treatment in vertebral compression]. Dtsch Med Wochenschr. 2003; 128:2525–2530. PMID: 14648434.
24. Winking M, Stahl JP, Oertel M, Schnettler R, Böker DK. Treatment of pain from osteoporotic vertebral collapse by percutaneous PMMA vertebroplasty. Acta Neurochir (Wien). 2004; 146:469–476. PMID: 15118884.

Fig. 1
A 54-year-old female with traumatic compression fracture at L1; we conducted unipedicular L1 vertebroplasty; reconstructed intraoperative conventional and rotational acquisition multiplanar reconstruction image.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download