1. Lee YB, Ha Y, Chon YE, Kim MN, Lee JH, Park H, et al. Association between hepatic steatosis and the development of hepatocellular carcinoma in patients with chronic hepatitis B. Clin Mol Hepatol. 2019; 25:52–64. PMID:
30360031.

2. Sartorius K, Sartorius B, Aldous C, Govender PS, Madiba TE. Global and country underestimation of hepatocellular carcinoma (HCC) in 2012 and its implications. Cancer Epidemiol. 2015; 39:284–290. PMID:
25922178.

3. Yu SJ. A concise review of updated guidelines regarding the management of hepatocellular carcinoma around the world: 2010-2016. Clin Mol Hepatol. 2016; 22:7–17. PMID:
27044761.

4. Kim JM, Joh JW, Yi NJ, Choi GS, Kwon C, Lee KW, et al. Living donor liver transplantation should be cautiously considered as initial treatment in recurrent hepatocellular carcinoma within the Milan criteria after curative liver resection. Ann Transl Med. 2020; 8:288. PMID:
32355732.

5. Shah SA, Greig PD, Gallinger S, Cattral MS, Dixon E, Kim RD, et al. Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg. 2006; 202:275–283. PMID:
16427553.

6. Jung SM, Kim JM, Choi GS, Kwon CH, Yi NJ, Lee KW, et al. Characteristics of early recurrence after curative liver resection for solitary hepatocellular carcinoma. J Gastrointest Surg. 2019; 23:304–311. PMID:
30215196.

7. Kim JM, Kwon C, Joh JW, Sinn DH, Choi GS, Paik SW. Prognosis of preoperative positron emission tomography uptake in hepatectomy patients. Ann Surg Treat Res. 2018; 94:183–189. PMID:
29629352.

8. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, et al. Outcomes after curative hepatectomy in patients with non-B non-C hepatocellular carcinoma and hepatitis B virus hepatocellular carcinoma from non-cirrhotic liver. J Surg Oncol. 2014; 110:976–981. PMID:
25171344.

9. Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, et al. Differences between hepatocellular carcinoma and hepatitis B virus infection in patients with and without cirrhosis. Ann Surg Oncol. 2014; 21:458–465. PMID:
24132624.

10. Kim JM, Hyuck C, Kwon D, Joh JW, Lee JH, Paik SW, et al. Protein induced by vitamin K antagonist-II (PIVKA-II) is a reliable prognostic factor in small hepatocellular carcinoma. World J Surg. 2013; 37:1371–1378. PMID:
23443153.

11. Lee JH, Cho Y, Kim HY, Cho EJ, Lee DH, Yu SJ, et al. Serum tumor markers provide refined prognostication in selecting liver transplantation candidate for hepatocellular carcinoma patients beyond the Milan criteria. Ann Surg. 2016; 263:842–850. PMID:
26779979.

12. Korean Liver Cancer Association. National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver. 2019; 13:227–299. PMID:
31060120.
13. Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018; 67:358–380. PMID:
28130846.

14. Trevisani F, D'Intino PE, Morselli-Labate AM, Mazzella G, Accogli E, Caraceni P, et al. Serum alpha-fetoprotein for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: influence of HBsAg and anti-HCV status. J Hepatol. 2001; 34:570–575. PMID:
11394657.

15. Hoshida Y, Toffanin S, Lachenmayer A, Villanueva A, Minguez B, Llovet JM. Molecular classification and novel targets in hepatocellular carcinoma: recent advancements. Semin Liver Dis. 2010; 30:35–51. PMID:
20175032.

16. Okuwaki Y, Nakazawa T, Shibuya A, Ono K, Hidaka H, Watanabe M, et al. Intrahepatic distant recurrence after radiofrequency ablation for a single small hepatocellular carcinoma: risk factors and patterns. J Gastroenterol. 2008; 43:71–78. PMID:
18297439.

17. Poté N, Cauchy F, Albuquerque M, Voitot H, Belghiti J, Castera L, et al. Performance of PIVKA-II for early hepatocellular carcinoma diagnosis and prediction of microvascular invasion. J Hepatol. 2015; 62:848–854. PMID:
25450201.

18. Bae HM, Lee JH, Yoon JH, Kim YJ, Heo DS, Lee HS. Protein induced by vitamin K absence or antagonist-II production is a strong predictive marker for extrahepatic metastases in early hepatocellular carcinoma: a prospective evaluation. BMC Cancer. 2011; 11:435. PMID:
21985636.

19. Chang Y, Cho Y, Lee JH, Lee YB, Cho EJ, Yu SJ, et al. Comparison of models for tumor recurrence after liver transplantation for the patients with hepatocellular carcinoma: a multicenter long-term follow-up study. Cancers (Basel). 2019; 11:1295.

20. Nam JY, Lee JH, Bae J, Chang Y, Cho Y, Sinn DH, et al. Novel model to predict HCC recurrence after liver transplantation obtained using deep learning: a multicenter study. Cancers (Basel). 2020; 12:2791.

21. Yoo J, Lee MW, Lee DH, Lee JH, Han JK. Evaluation of a serum tumour marker-based recurrence prediction model after radiofrequency ablation for hepatocellular carcinoma. Liver Int. 2020; 40:1189–1200. PMID:
32056353.

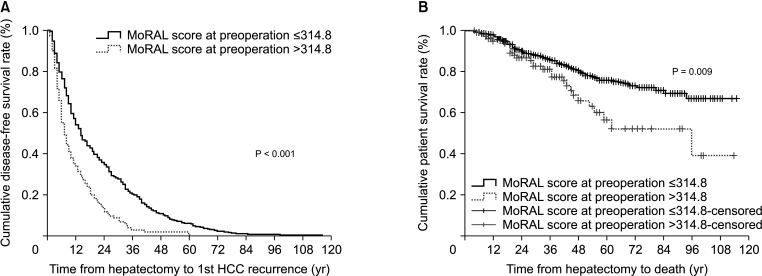
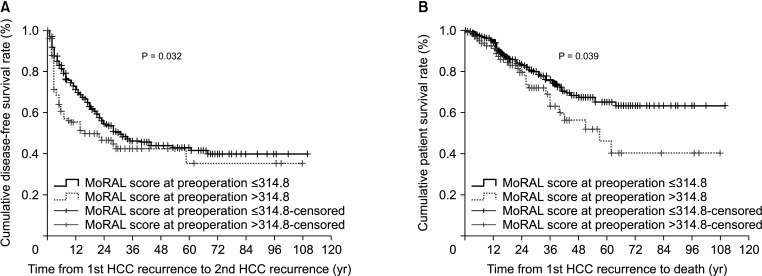
 ) employs 2 tumor markers [11]. A previous study reported that a low MoRAL score (<314.8 points) was closely associated with better recurrence-free survival and overall survival after LDLT compared with a high MoRAL score because MoRAL score reflects tumor aggressiveness and biology [11].
) employs 2 tumor markers [11]. A previous study reported that a low MoRAL score (<314.8 points) was closely associated with better recurrence-free survival and overall survival after LDLT compared with a high MoRAL score because MoRAL score reflects tumor aggressiveness and biology [11].



 PDF
PDF Citation
Citation Print
Print







 XML Download
XML Download