LETTERS TO EDITOR
We want to report a case of a 7-year-old girl, weighing 20 kg, diagnosed with B-cell acute lymphocytic leukemia, who presented at our pain clinic for intractable anal pain which she had suffered for 20 days.
She received 4 cycles of chemotherapy (vincristine and doxorubicin) and 3 months after the last cycle, the patient developed a perianal abscess with perianal swelling and anal pain. The perianal abscess was drained and a colostomy was done to promote wound healing. Post-procedure, despite the healing of the abscess, the pain continued, and it was severe enough to hinder the child's ability to stand or ambulate. Local examinations did not reveal perianal tenderness or myofascial trigger points. The complete blood counts, as well as the renal, liver and coagulation profiles were within normal limits. Ultrasonography and contrast medium-enhanced computed tomography of the abdomen showed no significant findings. The pain was relentless and did not even respond to intravenous administration of paracetamol (200 mg tid), diclofenac (20 mg bid), tramadol injections (20 mg bid), and local lignocaine jelly application. Only a continuous intravenous fentanyl infusion (10 µg/kg/h) gave her 50% relief in pain, and the cause of pain was not known.
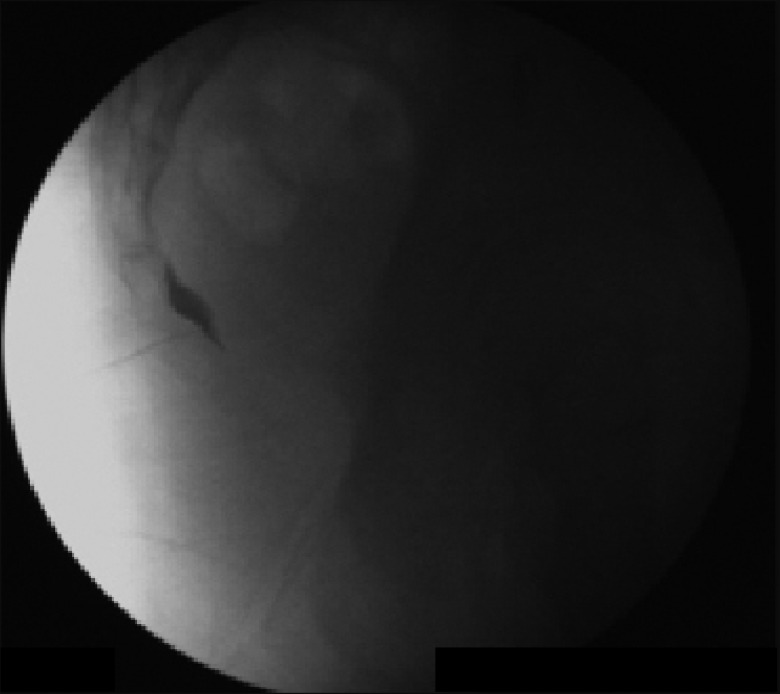
A ganglion impar block (transdiscal approach) was planned. The patient was shifted into the operation theater, and standard monitors were attached. The patient was positioned prone for the procedure, and, under strict asepsis, using fluoroscopic guidance, a 26 gauge 5 cm length needle was introduced at the sacro-coccygeal junction, crossing the disc in a single attempt. After satisfactory needle tip positioning in front of the sacro-coccygeal disc, 0.5 ml of the water soluble contrast medium iohexol was given. Contrast medium spread was satisfactory (Fig. 1), following which 3 ml of 2% lignocaine was instilled. Post-procedure, the needle was removed and a sterile bandage was applied over the wound site.
After the ganglion impar block the child had complete pain relief, and fentanyl infusion was stopped. On the 2nd day, when the patient was reassessed, she could sit and walk without pain. One week later the child was discharged from the hospital, and tablet paracetamol 250 mg was advised on an as-and-when-needed basis. At one month follow up she was pain free without any analgesics.
Anorectal diseases are a frequent complication with potentially fatal outcomes among patients with hematologic malignancies [1]. The incidence of perianal infection is approximately 8–9% in patients with acute leukemia [2]. Besides collateral damage to the normal gastrointestinal epithelium, cytotoxic chemotherapy leads to acute enteritis resulting in mal-absorption and tissue damage that can result in symptoms of bleeding, pain, diarrhea, and malnutrition [3]. Due to its life threatening nature, perianal signs and symptoms should be meticulously evaluated in such patients concerning early diagnosis and treatment. Pain in patients with blood cancers can be attributed to multiple causes with different neurobiological character, intensity, and duration. From somatic to visceral or sympathetic, infection to bone marrow infiltration or iatrogenic, the pain can have varied patho-physiologies and has to be managed accordingly [4]. Normally, the WHO pain ladder is to be followed for analgesia. Radiotherapy also helps in alleviation of pain, but the use of interventions for the management of pain due to blood cancers has not been widely studied.
The ganglion impar, is a singular retroperitoneal structure located at the level of the sacro-coccygeal junction. Blocking it is useful in patients who suffer from pain in the pelvic and perineal structures as it provides nociceptive and sympathetic supply to this region [5]. The ganglion impar block is a well established procedure for the treatment of coccydynia [6], but its role in the treatment of anal pain with varied aetiologies is not well studied. In our case, the ganglion impar block hit the pain pathway's bullseye, and we were able to relieve the patient's unbearable discomfort.
We therefore feel that once pain cannot be controlled by pharmacologic management, one should surely move to interventions, so as to provide relief to the patient. So, the ganglion impar block should be instituted early in the management of anal pain not responding to pharmacological management, all the more so in patients with acute lymphocytic leukemia following treatment of perianal infection.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download