Abstract
Burner or stinger syndrome is a rare sports injury caused by direct or indirect trauma during high-speed or contact sports mainly in young athletes. It affects peripheral nerves, plexus trunks or spinal nerve roots, causing paralysis, paresthesia and pain. We report the case of a 57-year-old male athlete suffering from burner syndrome related to a lumbar nerve root. He presented with prolonged pain and partial paralysis of the right leg after a skewed landing during the long jump. He was initially misdiagnosed since the first magnet resonance imaging was normal whereas electromyography showed denervation. The insurance company refused to pay damage claims. Partial recovery was achieved by pain medication and physiotherapy. Burner syndrome is an injury of physically active individuals of any age and may appear in the cervical and lumbar area. MRI may be normal due to the lack of complete nerve transection, but electromyography typically shows pathologic results.
Isolated nerve injuries in athletes are rare. They occur mostly during contact sports such as football, basketball, wrestling, baseball, and weightlifting, or during high-speed sports such as downhill skiing and cycling. In other kinds of sports, isolated injuries of peripheral nerves or nerve roots rarely occur. If observed, they are mainly located at the upper extremities or the cervical spine [1]. Mostly young athletes are afflicted. This sudden, sports-related injury is known as burner or stinger syndrome [23]. It presents as a sudden loss of sensitivity and motor function in the distribution area of the affected nerve, often accompanied by a radiating, burning, or stinging sensation of pain. It is caused by blunt trauma or sudden hyperextension during sports. Within a short period of time, signs of denervation can typically be verified by electrophysiological examination. We present the rare case of an elderly athlete suffering from lumbar burner syndrome.
In 2006, a 57-year-old sports teacher demonstrated the technique of the long jump to his students. He recalls having run and jumped off normally, but during the landing he touched the ground asymmetrically and a little twisted to the side, but without falling down. He immediately felt an acute pain in the lower back area accompanied by paraesthesia and partial paralysis of the right leg. He subsequently self-medicated with ibuprofen and stopped the sports lesson. During the following day, the pain didn't improve whereas the paralysis intensified.
He reported to an orthopedic clinic where a sensory-motor deficit corresponding to the distribution area of the fifth lumbar nerve root on the right side was found, based on clinical examination. Dorsiflexion force of the right foot and big toe was reduced to a level of 3/5, the Trendelenburg's-sign was positive. An electromyography was performed and found to be normal. A Magnet resonance imaging (MRI) of the lumbar spine was performed the same day, which only showed degenerative changes appropriate for the patient's age, but no signs of a fresh spinal injury or lesion explaining the symptoms corresponding to the fifth lumbar nerve root.
The patient was mobilized on crutches, received intensified oral pain medication and was discharged from the hospital.
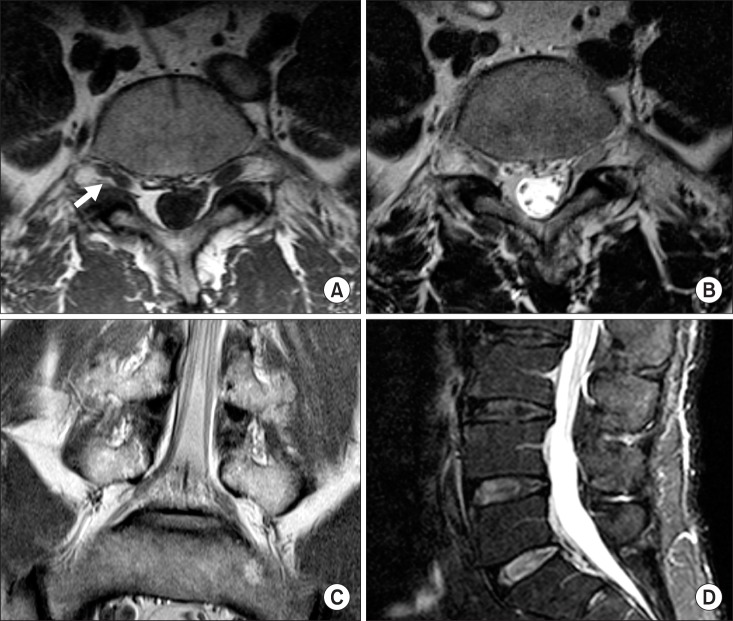
Since pain and paralysis remained, another MRI was performed two days later. The radiologist identified an hourglass-shaped constriction of the fifth lumbar nerve root as shown in Fig. 1. There were no signs of nerve root disruption or compression by other tissue, particularly there was no nor a herniated disc. Ten days later, the patient reported to another neurologist who, in a repeat EMG, now measured acute denervation (poly-phasic spontaneous activity) of the anterior and posterior tibialis muscles as well as of the gluteus medius muscle on the right side, compatible with an injury of the fifth lumbar nerve and the diagnosis of low back pain with sciatica and paralysis was made, despite the lack of an adequate imaging correlate. On the occasion of a follow-up visit one year later, paralysis and pain had improved slightly and another EMG was performed which still showed injury of the fifth lumbar nerve root.
Four years later, the patient still reports persisting sensory-motor deficits and pain in the distribution area of the fifth right lumbar nerve root despite consistent physio- and electrotherapy. Dorsiflexion force of the right foot and big toe is reduced to a level of 3/5 (Janda) while the Trendelenburg's sign is negative and the deep tendon reflexes of the lower limbs are equally symmetrical and of normal intensity. The straight-leg-raise test (Lasègue) and the passive foot extension test (Bragard) are negative.
The patient was misdiagnosed as simply suffering from low back pain and disc protrusion over four years. He consulted several doctors, but the burner syndrome was not recognized. Only after his accident insurance company refused payment, an expert opinion by a spine surgeon was requested, finally resulting in a diagnosis of burner syndrome, which had resulted directly from the incident during the long jump.
Sports injuries of peripheral nerves, the nerve plexus, or spinal nerve roots can cause immediate pain and loss of sensory and motor function [234]. Most frequently, the cervical nerve roots and the cervico-brachial plexus are particularly affected because of their anatomical location between the exposed and highly mobile cervical spine on the one end and the shoulder joint and the arm on the other. In consequence, mostly young athletes performing contact or high-impact sports such as football, basketball, weightlifting, wrestling, or baseball are affected. Krivickas and Wilbourn [1] retrospectively found that out of 346 athletes who suffered from sports related accidents, 180 patients had 216 nerve injuries, but only 22 of these patients were older than 40 years of age. Three patients suffered from an injury sustained during the long jump, but no lumbar nerve roots were affected in these cases. Injuries of lumbar nerve roots have only been reported in football players and cyclists [1].
The burner syndrome has repeatedly been described as a rare complication of injuries to the upper extremity in young athletes [56]. Cases concerning injuries of the lower extremities describe damage to the femoral, the sciatic, and the peroneal nerves caused by high-speed accidents or direct trauma [78]. Further differential diagnoses include lumbar fractures, lumbar disc herniations, plexus neuritis, or spinal cord injury. Accidents resulting in lumbar spine injuries typically occur as a result of forced hyperextension during football or rugby [9].
Seddon's original classification system for nerve injuries based on neurophysiological changes is the most widely used [710]. Grade 1 nerve injury is a neuropraxic condition, grade 2 is axonal degeneration and grade 3 is nerve transection [7]. Most authors describe a slow spontaneous improvement of symptoms. Treatment options are predominantly conservative, including physical rest, physical therapy, analgesia, and sometimes anticonvulsive medication. They may include surgical options in grade 3 injuries.
We show a case whose presentation was different from all previously described cases. The injury occurred during the long jump, which definitely seems to be capable of raising enough energy for such an injury by sudden hyperextension of the musculoskeletal system [1112]. Especially the landing phase imposes a sudden strong stretching momentum on the dorsal body muscles and the skeleton, hence lumbar nerve roots and peripheral nerves such as the sciatic nerve may be affected. Since burner or stinger syndrome is rare, many physicians may not be familiar with it, and as a consequence, the correct diagnosis will not be made, as in our patient who was misdiagnosed with as suffering from disc protrusion and chronic lumbar pain syndrome for over four years. He consulted several doctors, and two electromyographies showed an injury of the fifth lumbar nerve root, but the burner syndrome was not recognized. His accident insurance primarily refused to pay because burner syndrome was unknown to them and the event was not considered sufficiently traumatic to cause such an injury. The relationship between the trauma suffered and the damage of the nerve root was not accepted at first. This experience ties in well with the established value of independent medical examinations in complicated pain problems [13].
We conclude that the burner or stinger syndrome is a rare sports injury that is characterized by partial or complete loss of sensory and motor functions of the affected nerves and by a very particular type of neuropathic pain. Since it does not result in a complete transection of the nerve, partial or even complete remission of symptoms may result. Also, it is an injury of physically active individuals of any age rather than that of only young athletes.
References
1. Krivickas LS, Wilbourn AJ. Peripheral nerve injuries in athletes: a case series of over 200 injuries. Semin Neurol. 2000; 20:225–232. PMID: 10946743.

2. Kuhlman GS, McKeag DB. The “burner”: a common nerve injury in contact sports. Am Fam Physician. 1999; 60:2035–2040. 2042PMID: 10569506.
3. Speer KP, Bassett FH 3rd. The prolonged burner syndrome. Am J Sports Med. 1990; 18:591–594. PMID: 2285087.

5. Hirasawa Y, Sakakida K. Sports and peripheral nerve injury. Am J Sports Med. 1983; 11:420–426. PMID: 6650720.

6. Nissen SJ, Laskowski ER, Rizzo TD Jr. Burner syndrome: recognition and rehabilitation. Phys Sportsmed. 1996; 24:57–64.
7. Feinberg JH, Nadler SF, Krivickas LS. Peripheral nerve injuries in the athlete. Sports Med. 1997; 24:385–408. PMID: 9421863.

8. Lorei MP, Hershman EB. Peripheral nerve injuries in athletes. Treatment and prevention. Sports Med. 1993; 16:130–147. PMID: 8378668.
9. Fuller CW, Brooks JH, Kemp SP. Spinal injuries in professional rugby union: a prospective cohort study. Clin J Sport Med. 2007; 17:10–16. PMID: 17304000.

10. Choi EJ, Choi YM, Jang EJ, Kim JY, Kim TK, Kim KH. Neural ablation and regeneration in pain practice. Korean J Pain. 2016; 29:3–11. PMID: 26839664.

11. Hay JG. Citius, altius, longius (faster, higher, longer): the biomechanics of jumping for distance. J Biomech. 1993; 26(Suppl 1):7–21. PMID: 8505354.

12. Hay JG, Nohara H. Techniques used by elite long jumpers in preparation for takeoff. J Biomech. 1990; 23:229–239. PMID: 2324119.

13. Nahm FS, Lee PB, Kim TH, Kim YC, Lee CJ. Comparative analysis of the independent medical examination reports and legal decisions in pain medicine. Korean J Pain. 2010; 23:28–34. PMID: 20552070.

Fig. 1
Lumbar magnet resonance imaging. Magnet resonance imaging of the lumbar spine three days after the injury, showing an intraforaminal hourglass-shaped constriction of the right fifth lumbar nerve root in axial T2-weighted turbo-spin-echo sequences (A) and the axial T1-weighted sequences (B). The hourglass-shaped constriction can hardly be identified in the proton-density-weighted coronary sequence (C). There is no nerve transection or rupture. The sagittal stir sequence of the lumbar spine shows only mild degenerative changes of the lumbar discs without relevant protrusions (D).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download