Abstract
Background
Pain with neuropathic characteristics is generally more severe and associated with a lower quality of life compared to nociceptive pain (NcP). Short form of the Douleur Neuropathique en 4 Questions (S-DN4) is one of the most used and reliable screening questionnaires and is reported to have good diagnostic properties. This study was aimed to cross-culturally validate the Hindi version of the S-DN4 in patients with various chronic pain conditions.
Methods
The S-DN4 is already translated into the Hindi language by Mapi Research Trust. This study assessed the psychometric properties of the Hindi version of the S-DN4 including internal consistency and test-retest reliability after 3 days' post-baseline assessment. Diagnostic performance was also assessed.
Results
One hundred sixty patients with chronic pain, 80 each in the neuropathic pain (NeP) present and NeP absent groups, were recruited. Patients with NeP present reported significantly higher S-DN4 scores in comparison to patients in the NeP absent group (mean (SD), 4.7 (1.7) vs. 1.8 (1.6), P < 0.01). The S-DN4 was found to have an AUC of 0.88 with adequate internal consistency (Cronbach's α = 0.80) and a test-retest reliability (ICC = 0.92) with an optimal cut-off value of 3 (Youden's index = 0.66, sensitivity and specificity of 88.7% and 77.5%). The diagnostic concordance rate between clinician diagnosis and the S-DN4 questionnaire was 83.1% (kappa = 0.66).
Neuropathic Pain (NeP) is defined as pain caused by a lesion or disease of the somatosensory nervous system [1]. Pain with neuropathic characteristics is generally more severe and associated with a worse quality of life and incremental financial burdens as compared to nociceptive pain (NcP) [234]. Population studies using screening questionnaires have reported the NeP prevalence to be 7-8% [56]. However, a hospital based study in Germany found that 37% of people attending a primary care clinic with chronic low back pain had NeP [7]. NeP is often underdiagnosed and undertreated, probably due to lack of a golden standard for diagnosis, the requirement of specialized skills to assess NeP, and a lack of efficacious drugs for treatment [1].
NeP is presented with both positive and negative symptoms like allodynia, dysesthesia, numbness, etc. [8]. These symptoms can especially be used for differentiating NeP from NcP. Initial evidence by Dubuisson and Melzack [9] and later by Boureau [8] have suggested the discriminatory power of these key words for identification of NeP [89].
Screening questionnaires to assess NeP developed in past decade are based on this hypothesis, and have been extensively used across research and routine clinical practice including Douleur Neuropathique 4 (DN4), ID Pain, the Leeds Assessment of Neuropathic Symptoms and Signs (LANSS), the Pain DETECT questionnaire (PDQ), and the Neuropathic Pain Questionnaire (NPQ) for this purpose [10]. DN4, which was initially developed with French speaking patients with chronic pain is one of the most widely used and reliable screening questionnaires and is reported to have good diagnostic properties [11]. Its ease of use, understanding of the items, and easy scoring, not involving any complex calculations, are the major advantages.
DN4 consists of 10 items in its original version including 7 self-completing items by patients on various NeP symptoms, and 3 items which need to be filled by physician after bedside examination [11]. Thus, an expert or someone with training is required to complete it. As there is a dearth of resources in terms of trained manpower and time, use of the 10 item DN4 questionnaire in routine clinical practice is difficult.
Instead, various researchers including Bouhassira et al. [11] have validated an interview version of the DN4 or Short form of the Douleur Neuropathique en 4 Questions (S-DN4), which contains only 7 self-completing items on various NeP symptoms. Studies have reported a cut-off score of 3 as having the highest sensitivity (78%) and specificity (81.2%) [11]. The S-DN4 can be used in large scale epidemiological studies as a reliable patient reported outcome measure to identify NeP. The DN4 is cross-culturally adapted and validated in more than ten languages. The S-DN4 is cross-culturally adapted and validated in Arabic [1213], Dutch [14], and French [11].
There is no standardized screening questionnaire available in India for the assessment of NeP. We aimed to cross-culturally validate the Hindi version of the S-DN4 in patients with various chronic pain conditions.
This study proceeded following permission from the Mapi research trust to use and validate the S-DN4 questionnaire in the Hindi language. This study assessed the psychometric properties of the Hindi version of the S-DN4 in chronic pain conditions.
This study has been approved by the Institute Ethics Committee, PGIMER, Chandigarh, India. All participants provided written informed consent before participating in this study.
The S-DN4 is already translated into the Hindi language by Mapi Research Trust. In order to assess the comprehensibility of the Hindi version provided by Mapi Research Trust, cognitive debriefing of the provided Hindi version was done. Cognitive debriefing is a method to test and validate a questionnaire. It involves qualitative interview methods in small samples of patients. The translated Hindi version was initially assessed for comprehensibility in ten patients with chronic NeP (pain for 12 weeks in native Hindi speakers, with clinical diagnosis of NeP made by clinician).
During the interviews, patients discussed their understanding of the instructions, questionnaire items, and response options. Participants gave feedback on the relevance between items and evaluated the difficulty of the questionnaire.
To improve the performance of the translated questionnaire, pilot testing results were reviewed by the project manager. If there was any item where difficulties or misunderstandings were reported by more than 3 participants, then we modified it, incorporating the respondents' suggestions. Cross-cultural validation of the final version of the questionnaire translated into Hindi was tested. (final draft) (Supplementary material 1).
This stage was conducted in the referral pain clinic of a public tertiary care teaching hospital in India. All the recruited patients completed the S-DN4 together with socio-demographic information and other reference scales.
To assess test-retest repeatability, the questionnaire was re-administered to patients who agreed to participate in the repeatability part of this study 3 days after filling out the questionnaire at baseline.
(1) Numeric rating scale: Pain severity was assessed using a 0 to10 numeric rating scale (NRS). In the survey it asks: “On a scale from 0 to 10, mark/tell your level of present pain, with 0 being none and 10 being unbearable.”
(2) The S-DN4: The S-DN4, consisting of seven items (verbal descriptors) not related to physical examination, was used for the diagnosis of NeP. The seven items included were burning, painful cold, electric shocks, tingling, pins and needles, numbness, and itching. Positive responses (Yes) to these items were scored as 1, and negative ones (No) as 0. A total sum of these items provided the summary score of the S-DN4. Previous studies have identified two cut-off values including 3 or 4 yes responses out of the 7 items to differentiate NeP from NcP [1114].
We have followed the sample size calculation method used by De Andrés et al. [15] to validate the painDETECT questionnaire. All consecutive patients with chronic pain were included in this study. We expected a Cohen's kappa of 0.7 (assumed based on previous studies) for the S-DN4 questionnaire.
We needed to include 133 patients with chronic pain for a Cohen's kappa of 0.7 with 0.12 accuracy. Assuming 15% non-evaluable respondents, and to match the sample sizes of previous studies for comparison of results, the final sample size needed to be 160 patients, 80 in each group (NeP and non-NeP).
Demographic and disease details are reported as number and percentage or mean ± standard deviation (SD). Receiver operating characteristic (ROC) curve analysis was performed to assess the discriminative ability of the S-DN4 (against the gold standard diagnosis) to diagnose NeP.
Area under the curve (AUC) of 0.5 indicates ‘ no discrimination’, 0.7-0.79 indicates ‘ acceptable discrimination’, 0.8-0.89 indicates ‘ excellent discrimination’ and > 0.9 indicates ‘ outstanding discrimination’.
We also determined the cut-off score providing the best values for sensitivity and specificity (highest Youden's index) to differentiate chronic pain patients with or without NeP. For each cut-off score, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated. Concordance between the S-DN4 and gold standard diagnosis is assessed by Cohen's kappa. The internal consistency of the questionnaire was estimated using Cronbach's alpha. Cronbach's alpha of ≥ 0.7 is considered sufficient. The test-retest method was used to evaluate repeatability.
The intra-class correlation coefficient (ICC) was calculated between the test and retest scores. We assumed that there wouldn't be any change in symptoms between the two observations conducted at such a short interval. An ICC > 0.80 was considered to have excellent reliability. All the analyses were carried out using SPSS version 14 (SPSS Inc., Chicago, IL, USA).
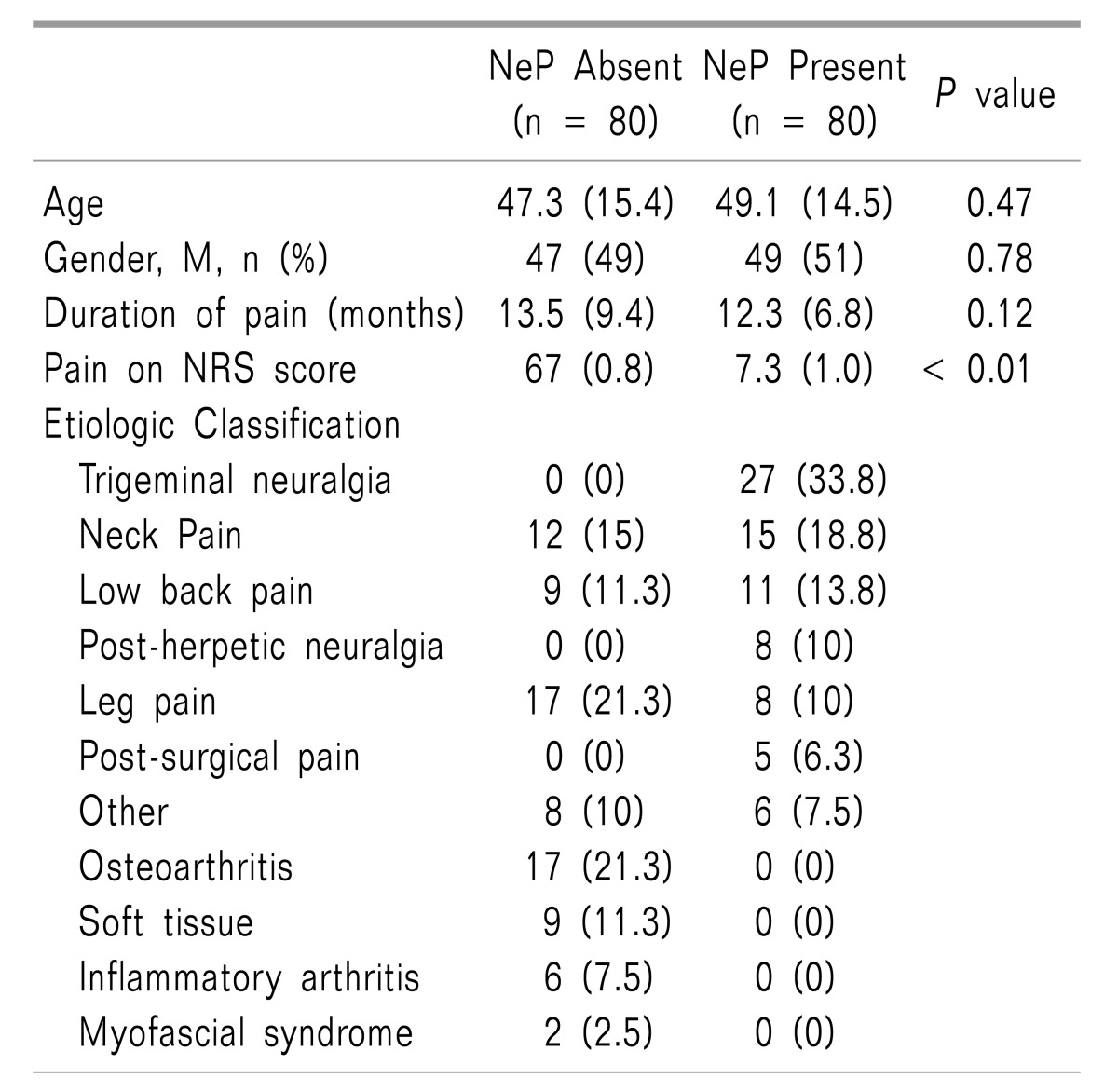
Results of the cognitive debriefing suggested that no modifications were required for any of the items in the Hindi version of the S-DN4. One hundred sixty patients with chronic pain were recruited, which included 80 patients each in the NeP present and NeP absent groups. The most prevalent diagnosis in the NeP present and NeP absent groups were trigeminal neuralgia and leg pain respectively (Table 1).
All included patients completed the baseline questionnaire. No significant difference in age (49.1), gender, or duration of pain was observed between patients between the NeP present and NeP absent groups (Table 1). NeP-positive patients suffered from significantly more severe pain (NRS, 7.3 (1.0) vs. 6.7 (0.8); P < 0.01) as compared to patients in the NeP absent group.
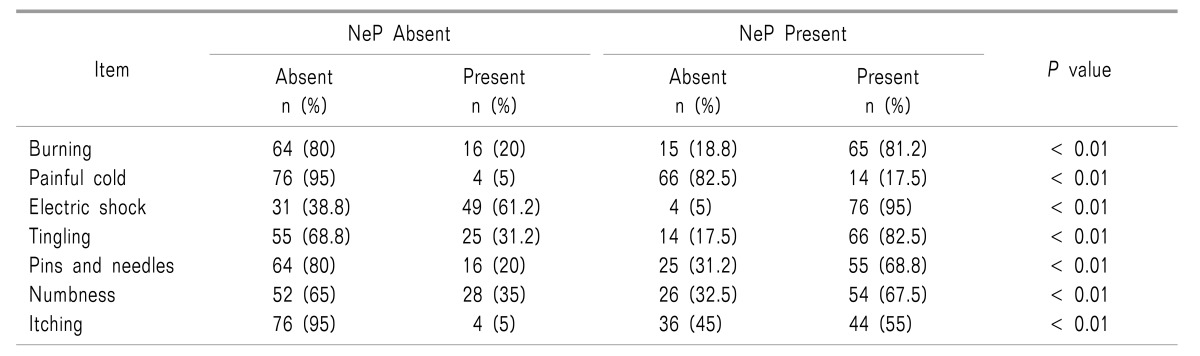
Patients in the NeP group have reported significantly higher S-DN4 scores in comparison to patients in the NeP absent group (mean (SD), 4.7 (1.7) vs. 1.8 (1.6), P <0.01). The proportion of patients responding “yes” to the items on the S-DN4 questionnaire was significantly (P < 0.01 for all individual items of S-DN4) higher in the NeP present group than that of the NeP absent group (Table 2).
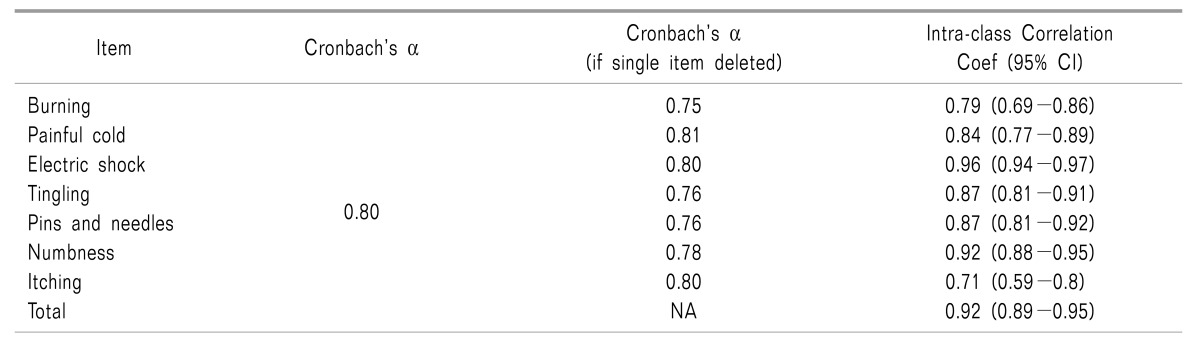
The Cronbach's α coefficient of the entire S-DN4 questionnaire is found to be 0.80, indicating acceptable to good internal consistency. Not much difference was observed in internal consistency by dropping any of the items in the questionnaire (Cronbach's α ranged from 0.75-0.81). Thus, all questions need to be present in the S-DN4 questionnaire (Table 3).
The retest was successfully administered after 3 days to 51.2% (n = 82) of the patients enrolled at baseline. Test-retest reliability was found to be very good with the ICC = 0.92 (95% CI, 0.89-0.95). The test-retest reliability of individual items was also found to be high with ICC ranging from 0.71 to 0.96. Results suggest that the S-DN4 has good to excellent test-retest reliability (Table 3).
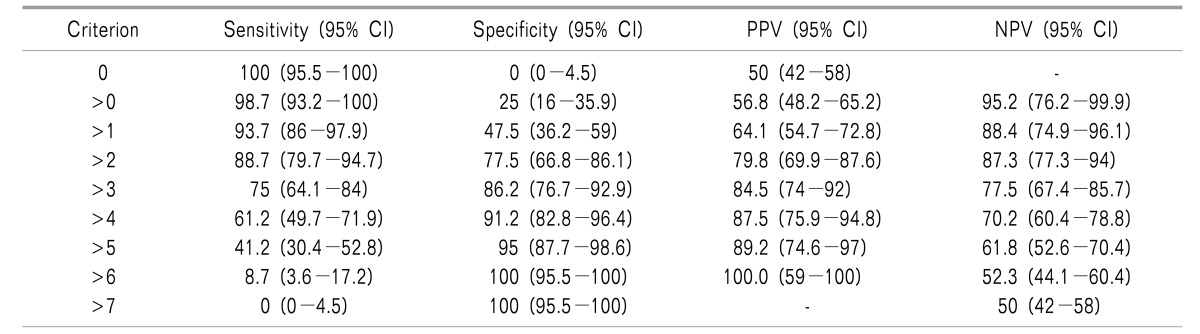
For calculating the AUC, the “clinician diagnosis (gold standard)” was considered as a reference. Sensitivity and specificity for various total cut-off scores of the questionnaire was calculated using an ROC curve. The AUC was found to be 0.88 (95% CI, 0.81-0.92) (Fig. 1A).
The best cutoff that maximizes sensitivity and specificity is a score of 3, with a Youden's index of 0.66, a sensitivity of 88.7% (95% CI, 79.5%-94.7%), a specificity of 77.5% (95% CI, 66.8%-86.1%), a PPV of 79.8% (95% CI, 69.9%-87.6%), and an NPV of 87.3% (95% CI, 77.3%-94%). Sensitivity and specificity according to various cutoff levels was also calculated (Table 4) and plotted (Fig. 1B).
According to the original developer, at cutoff level 4, the S-DN4 questionnaire's sensitivity and specificity are 75% (95% CI, 64.1%-84%) and 86.2% (95% CI, 76.7%-92.9%), respectively.
The diagnostic concordance rate between clinician diagnosis and the S-DN4 questionnaire is 83.1% (kappa = 0.66, 95% CI 0.55-0.79) at a cutoff level of 3 and 80.6% (kappa = 0.61, 95% CI 0.49-0.73) at a cutoff level of 4.
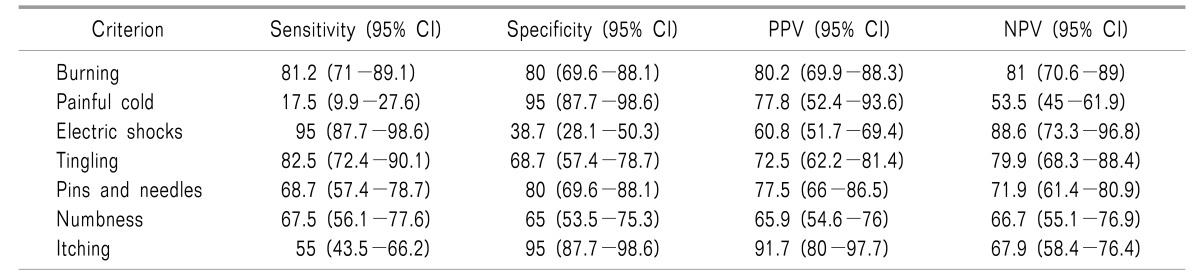
When the responses to individual questions of the S-DN4 were compared with the clinician diagnosis for diagnostic accuracy to differentiate NeP from non-NeP (Table 5), the question assessesing the “presence of electric shock pain” is found to have the highest sensitivity 95% but has a poor specificity 38.7%.
The question that assesses the “painful cold” is found to have the highest specificity, at 95%, but has poor sensitivity 17.5%. However, the question that assesses “burning pain” has a good sensitivity at 81.2% and a specificity at 80%.
This study evaluated the psychometric properties of the Hindi version of the S-DN4 in patients suffering from chronic pain. Overall, the results suggest that the Hindi version of the S-DN4 has good internal consistency and test-retest reliability along with good diagnostic accuracy. Few studies also shown that only the self-completing part of the DN4 have demonstrated good discriminatory properties in identifying NeP. The DN4 questionnaire is cross-culturally adapted and validated in Arabic [13], Dutch [14], French [11], Greek [16], German [14], Hungarian [14], Italian [17], Korean [18], Persian [19], Portuguese [20], Spanish [21], Turkish [22], and Thai languages [23].
We found an AUC of 0.88 for the Hindi version of the S-DN4 which is comparable to that of the original French (AUC = 0.87) [11] and Arabic version of the S-DN4 (AUC = 0.88) [12], but higher than the Dutch version (AUC = 0.81) [14]. We found an optimal cutoff value at 3 out of 7 which is similar to that of original developer and Arabic versions of the S-DN4 [12], but differed from the Dutch version [14], which has reported an optimal cutoff level of 4 out of 10.
The original developer reported sensitivity and specificity of 78% and 81.2%, respectively, with a cutoff 3 out of 7 [11]. We found higher sensitivity (88.7%) but lower specificity (77.5%) as compared to the original version. These study results are in line with those of the Arabic version, reporting higher sensitivity (89.4%) [12], but lower specificity (72.4%) as compared to the original study [11]. The Dutch version [14] of the DN4 reported that a cutoff point of 5/10 for the full questionnaire resulted in a sensitivity of 75% and a specificity of 79%, while a cutoff point of 4/7 for the S-DN4 resulted in lower sensitivity (74%) but comparable specificity (79%) to that of this study.
We found a good concordance (83%) higher than the concordance rate reported in the original study (79.5%) [11]. Ideally, a screening test should have both good sensitivity and specificity, but most of the time it is unachievable. So, based upon the disease condition, one can make a trade-off between sensitivity and specificity. This study has reported sufficient diagnostic accuracy of the S-DN4 questionnaire for differentiating NeP from NcP.
Results of the internal consistency analysis revealed good reliability of the S-DN4. This gives a clue that all 7 items of the questionnaire assess a similar construct i.e., NeP and all questions in the S-DN4 must be retained. Cronbach's α of Hindi version was higher than that of the Arabic version of the S-DN4 (Cronbach's α = 0.63) [12]. Internal consistency was not assessed for the French and Dutch version of S-DN4 [1114].
The test-retest reliability of the Hindi version is high (ICC = 0.92) which shows that the scores obtained are consistent over time with no change in disease status. The ICC obtained in this study was similar to that obtained for the Arabic version of the S-DN4 (ICC = 0.94) [12]. The test-retest reliability was not assessed for the French and Dutch version of the S-DN4 [1114]. Observed differences between the psychometric properties of the various translations of the S-DN4 may be due to differences in the clinical characteristics of the study participants. Moreover, the differences between the various translations of the S-DN4 signify the importance of assessing the psychometric properties of the Hindi version, and compare it with existing translations for efficient use in the Hindi dialect.
The Hindi version of the S-DN4 can be reliably used to assess NeP in both research and regular practice settings. The S-DN4 contains 7 verbal descriptors that can be self-completed by a patient and does not require trained personnel to administer. This makes the use of the S-DN4 convenient to administer and enables the screening of all patients attending the pain clinic. However, the results obtained from the S-DN4 can only provide initial clues about pain characteristics. Therefore, a sequential, complete diagnostic workup should be done after the initial assessment of NeP using the S-DN4. As the S-DN4 is easy to administer, analyze, and derive a result from, and is a reliable screening questionnaire, we recommend the usage of the S-DN4 in routine clinical practice, even in primary healthcare clinics.
The wide use of NP assessment screening questionnaires (the NPQ, ID Pain, PainDETECT, LANSS and DN4) has emerged recently over the past two decades [24]. These questionnaires have been used both for research and clinical practice. The questionnaires rely on either subject interview based questions or both interview based questions and physical examination tests for NP assessment. All the questionnaires are based on the differential presence of symptoms observed in patients with NP from NcP. The questionnaires consist of different symptoms, scoring methods, and modes of assessment (Table 6). Among all questionnaires, the DN4 is one of the most widely used.
This study has some limitations. It utilized the opinion of only one physician for determination of NeP, while many previous studies have used two physicians to determine the presence of NeP [1625]. Thus, this study results might be prone to assessment bias. Our institute pain clinic is considered a special clinic, and is only a referral clinic, where patients are referred from various other specialties. Hence, though the final discrimination of neuropathic or nociceptive pain was made by only one physician (pain physician), effectively one other physician (the primary referral physician) was involved in the diagnosis before referring the patient to the pain clinic. Discrimination of NP from NcP made by the pain physician was based on medical history, physical examination, electromyography, quantitative sensory tests, the quantitative sudomotor axon reflex test, laboratory examinations, and imaging techniques whenever indicated.
As no standard measure exists to assess NeP in the Hindi language, we did not assess the concurrent validity of the Hindi version of the S-DN4. Another limitation was the short test-retest time interval (3 days). This was selected assuming no change in the disease state within such a short span of time. However, the chance of the memory effect influencing the observed test-retest reliability cannot be ruled out. The sensitivity of instrument to change over time has not been tested. We have also not assessed the difference in properties of the S-DN4 according to various socio-demographic characteristics.
The Hindi version of the S-DN4 has good psychometric properties. As the S-DN4 is less time consuming and easy to administer, the present study recommends the use of the S-DN4 to assess NeP in regular clinical settings and research purposes, including epidemiological surveys. Further studies need to be done to assess the prognostic value of the Hindi version of the S-DN4.
ACKNOWLEDGEMENTS
To the best of our knowledge, no conflict of interest, financial or other, exists. No funding was provided for the analysis.
References
1. Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008; 70:1630–1635. PMID: 18003941.

2. Hiyama A, Watanabe M, Katoh H, Sato M, Sakai D, Mochida J. Evaluation of quality of life and neuropathic pain in patients with low back pain using the Japanese Orthopedic Association Back Pain Evaluation Questionnaire. Eur Spine J. 2015; 24:503–512. PMID: 25502001.

3. Freynhagen R, Baron R. The evaluation of neuropathic components in low back pain. Curr Pain Headache Rep. 2009; 13:185–190. PMID: 19457278.

4. Yamashita T, Takahashi K, Yonenobu K, Kikuchi S. Prevalence of neuropathic pain in cases with chronic pain related to spinal disorders. J Orthop Sci. 2014; 19:15–21. PMID: 24306580.

5. Torrance N, Smith BH, Bennett MI, Lee AJ. The epidemiology of chronic pain of predominantly neuropathic origin. Results from a general population survey. J Pain. 2006; 7:281–289. PMID: 16618472.

6. Bouhassira D, Lantéri-Minet M, Attal N, Laurent B, Touboul C. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain. 2008; 136:380–387. PMID: 17888574.

7. Freynhagen R, Baron R, Gockel U, Tölle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006; 22:1911–1920. PMID: 17022849.

8. Boureau F, Doubrère JF, Luu M. Study of verbal description in neuropathic pain. Pain. 1990; 42:145–152. PMID: 2247313.

9. Dubuisson D, Melzack R. Classification of clinical pain descriptions by multiple group discriminant analysis. Exp Neurol. 1976; 51:480–487. PMID: 1269574.

10. Bennett MI, Attal N, Backonja MM, Baron R, Bouhassira D, Freynhagen R, et al. Using screening tools to identify neuropathic pain. Pain. 2007; 127:199–203. PMID: 17182186.

11. Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005; 114:29–36. PMID: 15733628.

12. Harifi G, Ouilki I, El Bouchti I, Ouazar MA, Belkhou A, Younsi R, et al. Validity and reliability of the Arabic adapted version of the DN4 questionnaire (Douleur Neuropathique 4 Questions) for differential diagnosis of pain syndromes with a neuropathic or somatic component. Pain Pract. 2011; 11:139–147. PMID: 20602717.

13. Chatila N, Pereira B, Maarrawi J, Dallel R. Validation of a new Arabic version of the neuropathic pain diagnostic questionnaire (DN4). Pain Pract. 2017; 17:78–87. PMID: 26895970.

14. van Seventer R, Vos C, Giezeman M, Meerding WJ, Arnould B, Regnault A, et al. Validation of the Dutch version of the DN4 diagnostic questionnaire for neuropathic pain. Pain Pract. 2013; 13:390–398. PMID: 23113981.

15. De Andrés J, Pérez-Cajaraville J, Lopez-Alarcón MD, López-Millán JM, Margarit C, Rodrigo-Royo MD, et al. Cultural adaptation and validation of the painDETECT scale into Spanish. Clin J Pain. 2012; 28:243–253. PMID: 21926908.

16. Sykioti P, Zis P, Vadalouca A, Siafaka I, Argyra E, Bouhassira D, et al. Validation of the Greek version of the DN4 diagnostic questionnaire for neuropathic pain. Pain Pract. 2015; 15:627–632. PMID: 24796220.

17. Padua L, Briani C, Truini A, Aprile I, Bouhassirà D, Cruccu G, et al. Consistence and discrepancy of neuropathic pain screening tools DN4 and ID-Pain. Neurol Sci. 2013; 34:373–377. PMID: 22434411.

18. Kim HJ, Park JH, Bouhassira D, Shin JH, Chang BS, Lee CK, et al. Validation of the Korean version of the DN4 diagnostic questionnaire for neuropathic pain in patients with lumbar or lumbar-radicular pain. Yonsei Med J. 2016; 57:449–454. PMID: 26847299.

19. Madani SP, Fateh HR, Forogh B, Fereshtehnejad SM, Ahadi T, Ghaboussi P, et al. Validity and reliability of the persian (Farsi) version of the DN4 (Douleur Neuropathique 4 Questions) questionnaire for differential diagnosis of neuropathic from non-neuropathic pains. Pain Pract. 2014; 14:427–436. PMID: 23763722.

20. Santos JG, Brito JO, de Andrade DC, Kaziyama VM, Ferreira KA, Souza I, et al. Translation to Portuguese and validation of the Douleur Neuropathique 4 questionnaire. J Pain. 2010; 11:484–490. PMID: 20015708.

21. Perez C, Galvez R, Huelbes S, Insausti J, Bouhassira D, Diaz S, et al. Validity and reliability of the Spanish version of the DN4 (Douleur Neuropathique 4 questions) questionnaire for differential diagnosis of pain syndromes associated to a neuropathic or somatic component. Health Qual Life Outcomes. 2007; 5:66. PMID: 18053212.

22. Unal-Cevik I, Sarioglu-Ay S, Evcik D. A comparison of the DN4 and LANSS questionnaires in the assessment of neuropathic pain: validity and reliability of the Turkish version of DN4. J Pain. 2010; 11:1129–1135. PMID: 20418179.

23. Chaudakshetrin P, Prateepavanich P, Chira-Adisai W, Tassanawipas W, Leechavengvongs S, Kitisomprayoonkul W. Cross-cultural adaptation to the Thai language of the neuropathic pain diagnostic questionnaire (DN4). J Med Assoc Thai. 2007; 90:1860–1865. PMID: 17957931.
24. Cruccu G, Truini A. Tools for assessing neuropathic pain. PLoS Med. 2009; 6:e1000045. PMID: 19360134.

25. Li J, Feng Y, Han J, Fan B, Wu D, Zhang D, et al. Linguistic adaptation, validation and comparison of 3 routinely used neuropathic pain questionnaires. Pain Physician. 2012; 15:179–186. PMID: 22430656.
Fig. 1
(A) Receiver operating characteristic curve of S-DN4 questionnaire vs. clinician diagnosis to detect NeP in patients with chronic pain; AUC 0.88 (95% CI, 0.81–0.92; P < 0.01). (B) Plot representing change in sensitivity and specificity according to the overall S-DN4.
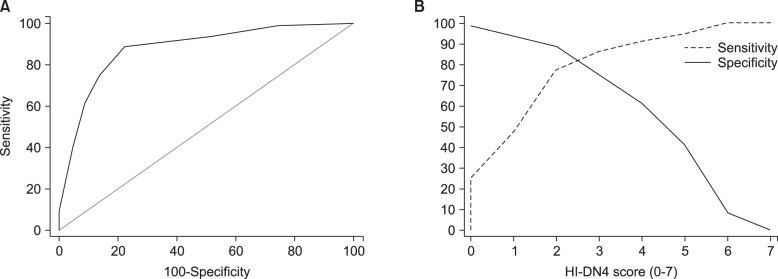
Table 6
Tools for Assessing Neuropathic Pain
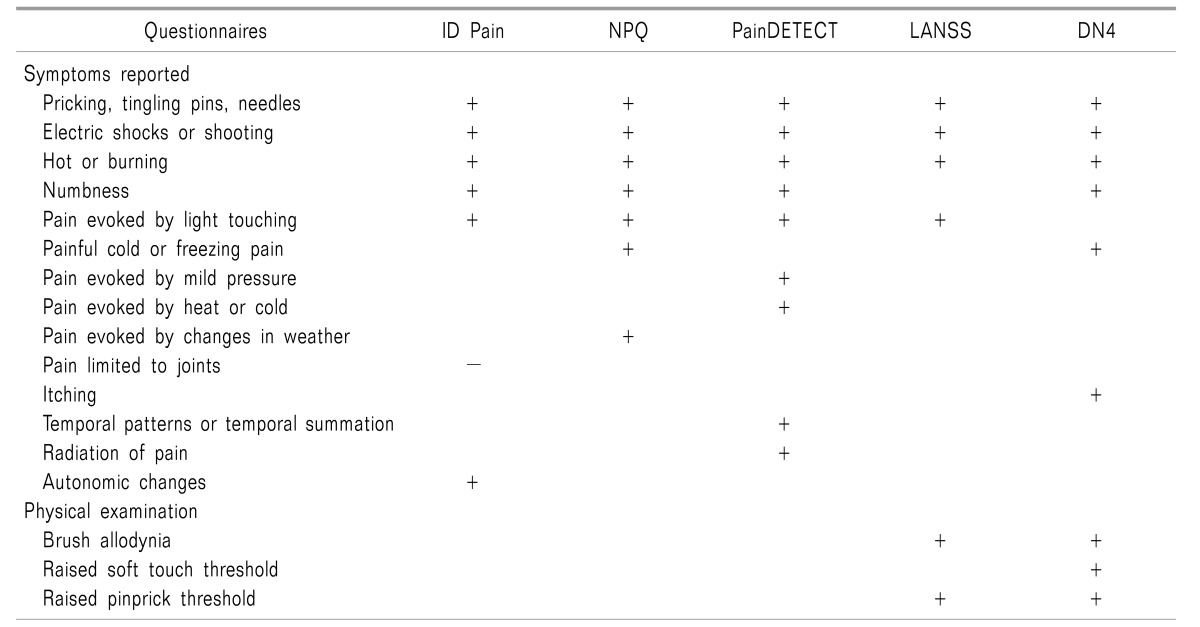
The plus (+) and minus (−) signs indicates items that increase and decrease the score respectively. Table adapted from Cruccu G et al. PLoS Med 6(4): e1000045. doi: 10.1371/journal.pmed.1000045 [24].




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download