Abstract
Background
C-arm fluoroscopy equipment is important for interventional pain management and can cause radiation injury to physicians and patients. We compared radiation safety education and efforts to reduce the radiation exposure of pain specialists.
Methods
A survey of 49 pain specialists was conducted anonymously in 2016. The questionnaire had 16 questions. That questionnaire was about radiation safety knowledge and efforts to reduce exposure. We investigated the correlation between radiation safety education and efforts of radiation protection. We compared the results from 2016 and a published survey from 2011.
Results
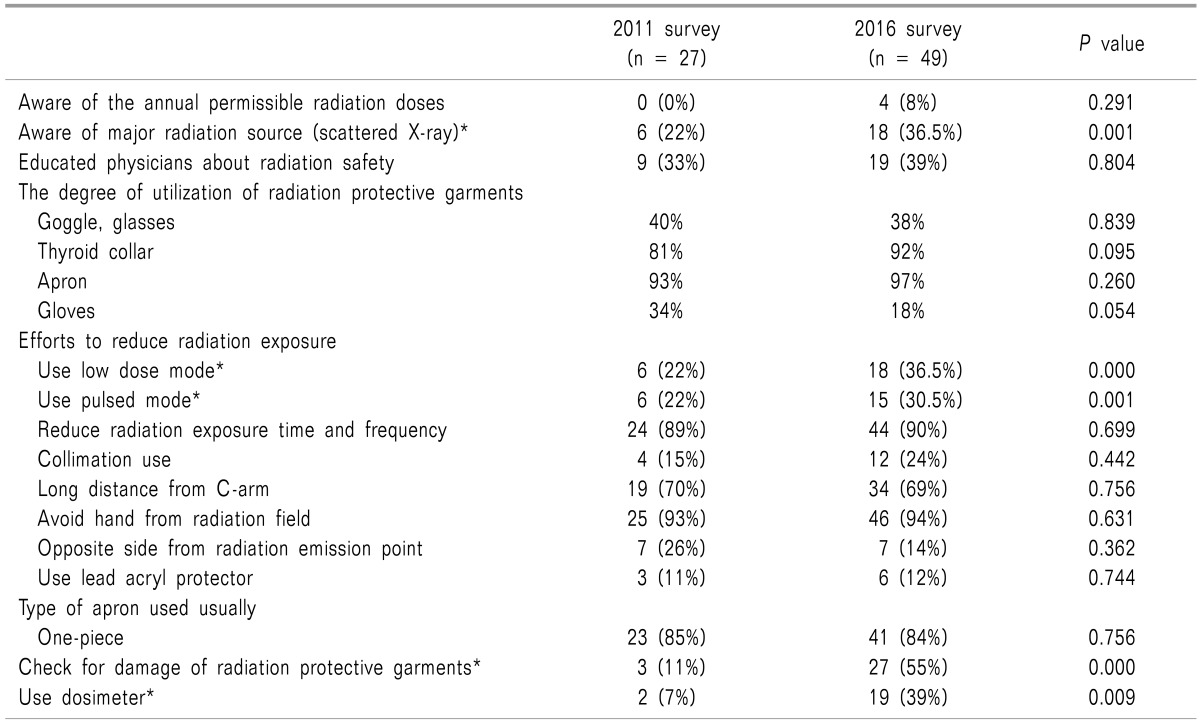
According to the 2016 survey, all respondents used C-arm fluoroscopy in pain interventions. Nineteen respondents (39%) had received radiation safety education. Physicians had insufficient knowledge about radiation safety. When the radiation safety education group and the non-education group are compared, there was no significant difference in efforts to reduce radiation exposure and radiation safety knowledge. When the 2011 and 2016 surveys were compared, the use of low dose mode (P = 0.000) and pulsed mode had increased significantly (P = 0.001). The number checking for damage to radiation protective garments (P = 0.000) and use of the dosimeter had also increased significantly (P = 0.009). But there was no significant difference in other efforts to reduce radiation exposure.
Conclusions
Pain physicians seem to lack knowledge of radiation safety and the number of physicians receiving radiation safety education is low. According to this study, education does not lead to practice. Therefore, pain physicians should receive regular radiation safety education and the education should be mandatory.
In numerous medical cases, the use of radiation is essential for diagnosis and treatment [1]. C-arm fluoroscopy equipment has been useful in pain intervention [2]. However, C-arm fluoroscopy-guided intervention is followed by radiation exposure. Therefore, radiation exposure is inevitable to the physician, and can have a negative impact on their health. Manifestation of such effects can appear after a few years, so it's hard to recognize the relationship between radiation exposure and the symptoms [3]. Pain physicians who use C-arm fluoroscopy may be at relatively high risk of radiation because of radiation accumulated over the years. Risk management of radiation exposure is one of the most important priorities in using fluoroscopy [4].
Many ways to reduce the radiation exposure have been used [56789]. And it implemented an education related to radiation safety. Education is an essential element for the pain physicians, but it is not compulsory for physicians in Korea [10]. The degree of radiation safety knowledge and radiation safety education is not well known in Korea. We conducted a survey related to radiation safety and education in 2016 to investigate pain physicians' radiation safety knowledge and efforts.
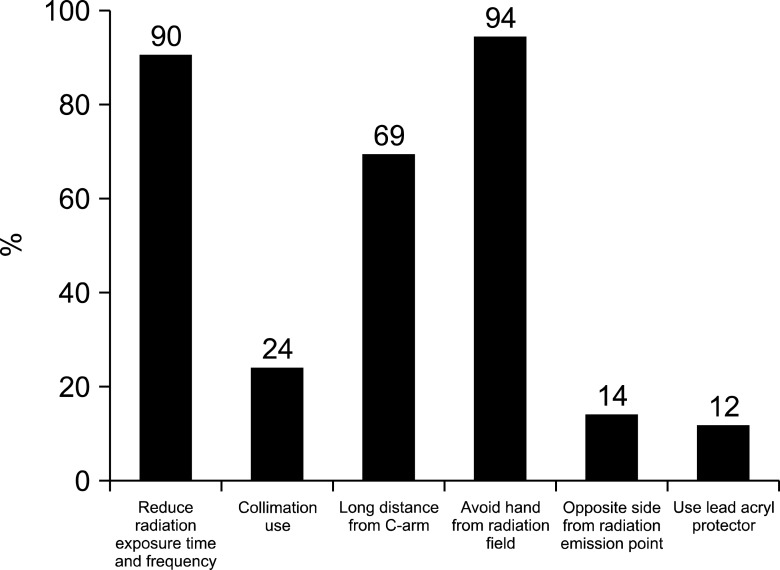
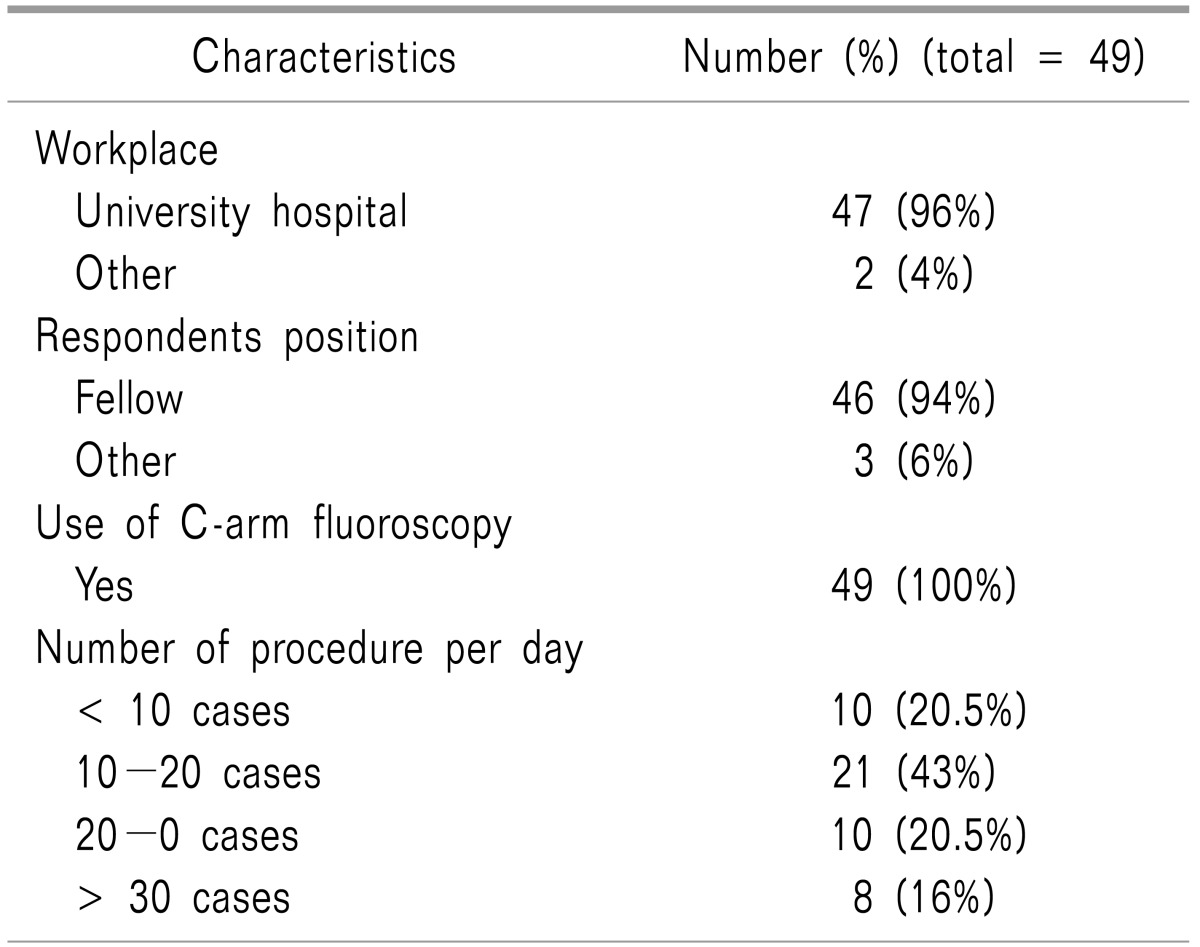
An anonymous survey was conducted of 49 pain physicians who completed the final exam of the Korean Pain Society to become pain specialists in 2016. The questionnaire contained 16 questions. These included the type of hospital they worked at, their position, the degree to which they use the C-arm fluoroscope, their average number of procedures per day, radiation safety education, knowledge of annual maximum permissible radiation doses, utilization ratio of radiation protection equipment, and so on. The 2016 survey contents are referenced in Appendix 1.
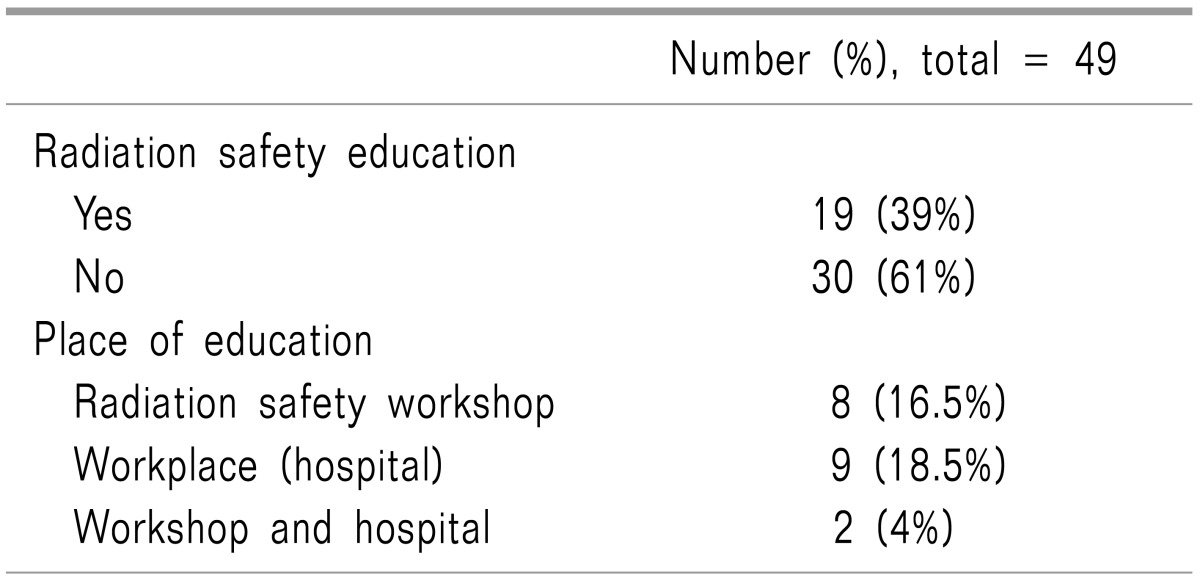
In the 2016 survey, each question was analyzed. Radiation safety knowledge and efforts to reduce radiation exposure were compared between the group who receive radiation safety education and the group who did not. We had investigated radiation safety through an anonymous survey in 2011. The 2011 survey was referenced in a previous article of Korean Journal of Pain [10]. And various data about radiation safety were compared between the 2011 and 2016 surveys.
Statistical analyses were performed on SPSS version 17. Mean differences such as the degree of using the C-arm fluoroscope, utilization ratio of radiation protection equipment, and so on, were analyzed using an independent sample t-test. Categorical data such as gender, the type of working hospital, position, radiation safety education, knowledge of annual maximum permissible radiation doses, and so on, were analyzed using chi-square test. A P value < 0.05 was considered statistically significant.
Forty-seven (96%) out of 49 respondents worked in university hospitals, and 2 respondents (4%) worked in hospitals specializing in the spine and joints in the 2016 survey. Forty-six (94%) out of 49 respondents were pain fellows, and all respondents used C-arm fluoroscopy during intervention. The number of procedures with C-arm fluoroscopy per day varied. Ten (20.5%) out of 49 respondents stated < 10, 21 respondents (43%) answered 10-20, 10 respondents (20.5%) reported 20-30, and 8 respondents (16%) answered > 30. All 49 respondents (100%) were worried about biological adverse effects due to radiation exposure (Table 1).
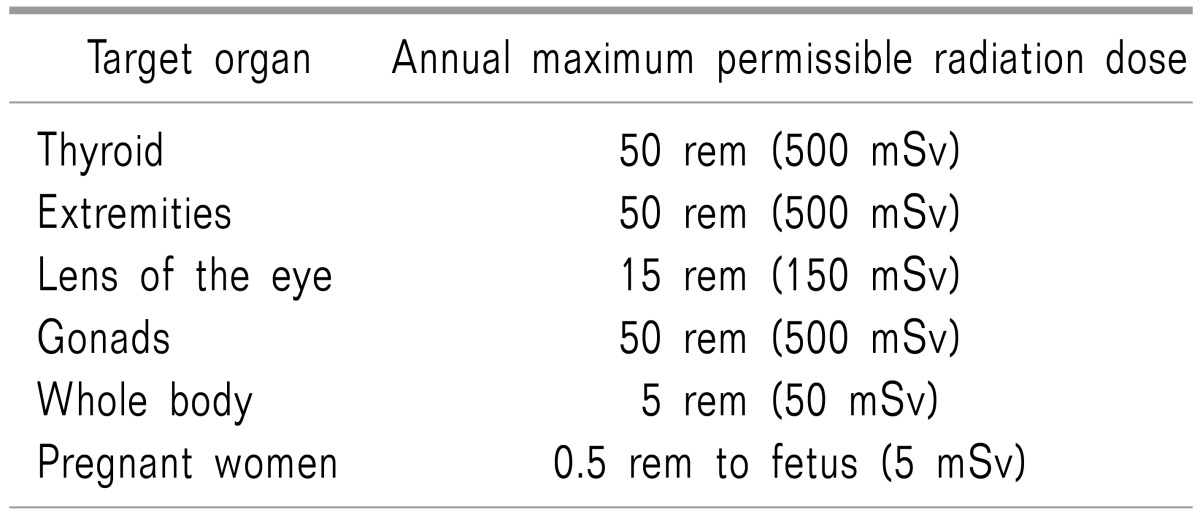
Nineteen (39%) out of 49 respondents were educated on radiation safety. Eight (16.5%) out of 49 respondents reported that they learned about radiation safety from a workshop of the Korean Pain Society, 9 (18.5%) respondents were educated by their working hospitals, and 2 (4%) respondents learned from both the workshop of the Korean Pain Society and their working hospitals (Table 2). Four (8%) out of 49 respondents knew the annual maximum permissible radiation doses exactly (Table 3). Eighteen (36.5%) out of 49 respondents knew the correct source of radiation exposure, scattered X-rays. Only 2 (4%) out of 49 respondents knew the exact degree of shielding from radiation in aprons or other radiation protective devices.
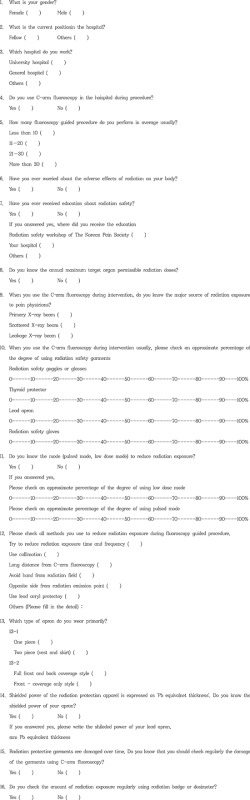
Radiation protective garments such as glasses or goggles, thyroid collars, aprons, and gloves were evaluated in the survey (Fig. 1). There was 1 physician who did not respond in the 2016 survey. Seven respondents (14.5%) used goggles all the time, 4 respondents (8%) used them 90% of the time, 2 respondents (4%) used them 80% of the time, 4 respondents (8%) used them 70% of the time, 2 respondents (4%) used them 60% of the time, 2 respondents (4%) used them 40% of the time, 2 respondents (4%) used them 20% of the time, 8 respondents (16.5%) used them 10% of the time, and 17 respondents (35%) did not use goggles. Regarding the thyroid collar, 32 respondents (65.5%) used it 100% of the time, 7 respondents (14.5%) used it 90% of the time, 4 respondents (8%) used it 80% of the time, 2 respondents (4%) used it 70% of the time, 2 respondents (4%) used it 50% of the time, 1 respondent (2%) used it 30% of the time, and there was no respondent who did not use the thyroid collar. In terms of the apron, 41 respondents (84%) used it 100% of the time, 4 respondents (8%) used it 90% of the time, 1 respondent (2%) used it 80% of the time, 2 respondents (4%) used it 50% of the time. No respondents reported that they did not use the apron. For the gloves, only 2 respondents (4%) used them 100% of the time, 1 respondent (2%) used them 90% of the time, 1 respondent (2%) used them 80% of the time, 5 respondents (10.5%) used them 50% of the time, 5 respondents (10.5%) used them 30% of the time, 2 respondents (4%) used them 20% of the time, and 6 respondents (12%) used them 10% of the time. Twenty-six respondents (53%) did not use the gloves at all.
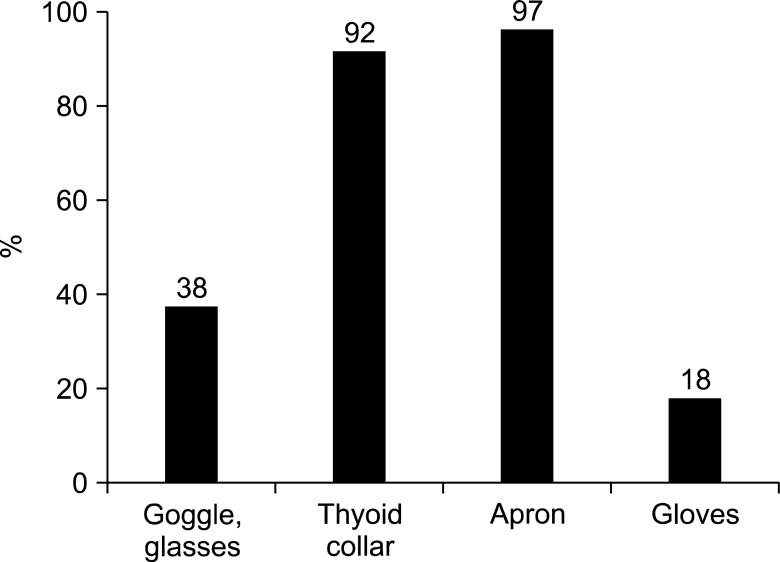
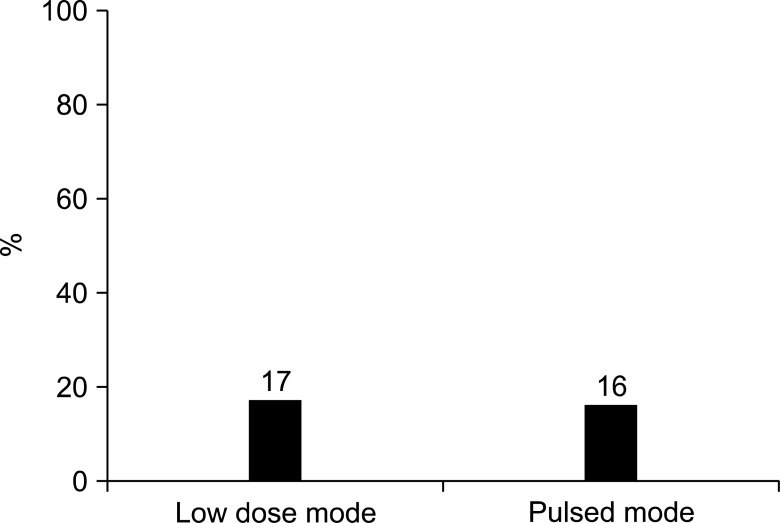
Twenty-four respondents (49%) knew the modes to reduce radiation exposure from the C-arm fluoroscope; low dose mode and pulsed mode (1 non-respondent) (Fig. 2). Eighteen respondents (36.5%) have been using low dose mode (14 non-respondents (28.5%)). One respondent (2%) used it 100% of the time, 2 respondents (4%) used it 90% of the time, 2 respondents (4%) used it 80% of the time, 1 respondent (2%) used it 70% of the time, 4 respondents (8%) used it 50% of the time, 1 respondent (2%) used it 30% of the time, 2 respondents (4%) used it 20% of the time, and 5 respondents (10.5%) used it 10% of the time. Seventeen respondents (35%) did not use low dose mode. Fifteen respondents (30.5%) used pulsed mode. There were 15 non-respondents (30.5%). Two respondents (4%) used it 100% of the time, 4 respondents (8%) used it 90% of the time, 3 respondents (6.17%) used it 50% of the time, 3 respondents (6.17%) used it 20% of the time, 3 respondents (6.17%) used it 10% of the time, and 19 respondents (39%) did not use pulsed mode. We also evaluated other methods to reduce radiation exposure (Fig. 3). One non-respondent was noted. Forty-four respondents (90%) tried to reduce frequency and duration of exposure, and 12 respondents (24%) used collimation. Thirty-four respondents (69%) maintained as much distance from C-arm as much as they could, 46 respondents (94%) tried not to put their hands in radiation fields, 7 respondents (14%) performed procedures on the opposite side from the radiation source, and 6 respondents (12%) used a lead acrylic protector.
In terms of the type of apron, a majority of the aprons were still the one-piece type; 41 (84%) out of 49 respondents answered they were using the one-piece type. Fifteen respondents (30.5%) used the front and back protection type, 20 respondents (41%) used the front protection type, and 14 respondents (28.5%) did not respond.
Thirty-six (73%) out of 49 respondents were aware of the need for evaluation of radiation protection devices such as aprons or goggles to make sure their radiation protection functions work properly. Twenty-seven respondents (55%) actually checked, which reveals a significant increase in evaluation of radiation protection devices. Nineteen respondents (39%) used a dosimeter.
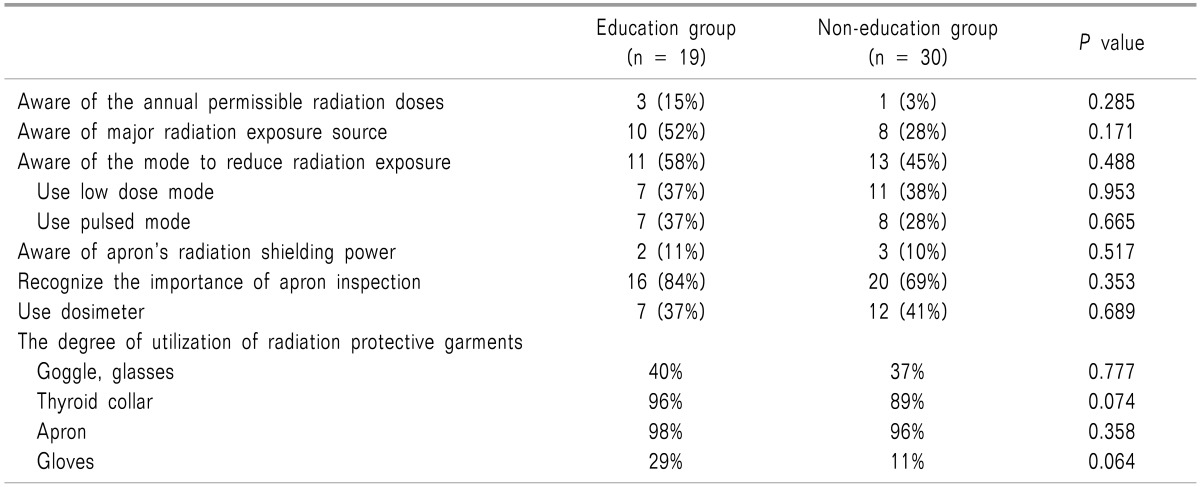
We evaluated the difference in efforts to reduce radiation exposure between physicians who received radiation safety education and who did not in the 2016 survey (Table 4). There was no statistically significant difference in the rate of using goggles, thyroid collars, aprons, and gloves, the knowledge of the annual permissible radiation dose, the major source of radiation exposure, modes to reduce radiation exposure, the apron's radiation shielding power, and knowledge in general about radiation exposure. Also this result did not show statistically significant difference in use of low dose mode, and pulsed mode between the education and non-education groups.
We also evaluated the difference between the 2011 survey [10] and the 2016 survey (Table 5). Eighteen (36.5%) out of 49 respondents knew the correct source of radiation exposure, scattered X-rays, which is a statistically significantly increase compared to the 2011 results; 6 (22%) out of 27 respondents had known the source of radiation exposure in the 2011 survey. The number of pain physicians who used low dose mode and pulsed mode was statistically significantly increased compare to the 2011 results. And the number of pain physicians who actually checked the damage to radiation protective devices and who used a dosimeter was significantly increased (Table 5). However, 19 (39%) out of 49 respondents were educated on radiation safety, which did not show a significant difference compared to the 2011 results; 9 (33%) out of 27 respondents had been educated in the 2011 survey. The number of pain physicians who knew the annual permissible radiation dose and who used radiation protective garments is not significantly difference between the 2011 survey and the 2016 survey (Table 5). There were no significant differences in other methods of reducing radiation exposure compared to the 2011 survey, except using low mode and pulsed mode. Most pain physicians still wear one-piece type aprons, with no significant difference compared to the 2011 survey results (2016: 84% of pain physicians, 2011: 85% of pain physicians).
In this study, all pain physicians used C-arm fluoroscopy in pain interventions; therefore, they were inevitably exposed to radiation. All pain physicians worried about the harmful effect of radiation exposure, however they seem to lack knowledge of radiation safety. The important thing in reducing radiation exposure is to acquire knowledge related to radiation safety and protection. However, the number of physicians who received radiation safety education was only 39% (19 out of 49).
The International Committee on Radiation Protection recommended the annual maximum permissible target-organ radiation doses in 1991 (Table 3) [3]. Only 4 (8%) out of the 49 respondents knew the annual maximum permissible target-organ radiation doses in this survey. Pain physicians must know the annual maximum permissible radiation dose to protect their body against radiation exposure and check their radiation exposure doses regularly to know their annual radiation exposure doses exactly. A single dosimeter is worn under the lead apron, a double dosimeter with one dosimeter inside and one outside the apron provides the radiation dose for eyes and extremities. It can be recommended that physicians use the double dosimeter during interventional procedures [11]. In 2016, the dosimeter use rate was 39%, which was significantly higher than the 7% in 2011, but not much.
Because of the adverse effects of radiation, pain physicians should make several efforts to reduce radiation exposure and be adequately trained to minimize radiation exposure by using ALARA (as low as reasonably achievable) principle [1213]. The 3 types of Ionizing radiation exposure are primary X-ray beams, scattered X-ray beams, and leakage X-ray beams [5]. The major radiation exposure source to physicians is the scattered X-ray beam. Scattered radiation is spread in all directions from the patient and table, and it is difficult to predict the direction [14]. The scattered exposure dose is higher near the X-ray tube and the scattered levels are inversely proportional to the square of the distance from the irradiated patient and table [5]. Therefore, exposure to radiation can be reduced by positioning physicians farther away from the C-arm fluoroscope and patient. It is recommended that pain physicians perform procedures on the side of the image receptor not the side of the X-ray tube while checking lateral fluoroscopy, and that they should keep their hands away from the irradiated area [15].
There are several protective garments such as the lead apron, goggles or glasses, gloves, and thyroid collar, and use of a large mobile lead acrylic shield to reduce radiation exposure [16]. It is recommended that physicians use more protective devices for their radiation protection [16]. To attenuate over 90% of scattered X-rays, an apron with over 0.5 mm lead equivalent thickness is needed. And the lead acrylic shield has a 1.0-1.5 mm lead equivalent thickness which almost completely attenuates the scattered X-ray beams [5]. A thyroid collar can block radiation for the neck and thyroid, and should be of 0.5 mm lead equivalent thickness. Generally, radiation protective gloves used in pain intervention reduce radiation by 25.8-26.5% [9]. The average rate of wearing the lead apron and thyroid collar were high (97% and 92%, respectively). And there was no one who did not use them in the 2016 survey. The average rate of wearing goggles and gloves were low (38% and 18% respectively). The rate of physicians using the acrylic protector was only 12% (6 out of 49). Despite the high rate of wearing the apron, only 2% of the pain physicians knew the shielding power of the apron they were wearing. Aprons can be divided into 3 types: front – coverage only, full front and back coverage, and two – piece aprons with a wraparound skirt and vest. Full front and back coverage aprons or front and back two–piece aprons are useful for protection from radiation. These styles of apron provide double–barrier thickness in the front area. If the lead equivalent thickness is 0.25 mm, the front side is equal to 0.5 mm lead equivalent thickness [3]. Radiation protective garments could crack or tear over time, and the ability to shield radiation could be reduced. Therefore, all garments should be checked regularly using fluoroscopy [6].
In addition, pain physicians tried to reduce radiation exposure time and frequency. Pulsed and low dose fluoroscopy can decrease radiation exposure time and radiation dose [71317]. Pain physicians could use collimation to reduce the radiation exposure dose and maintain a good image quality [813].
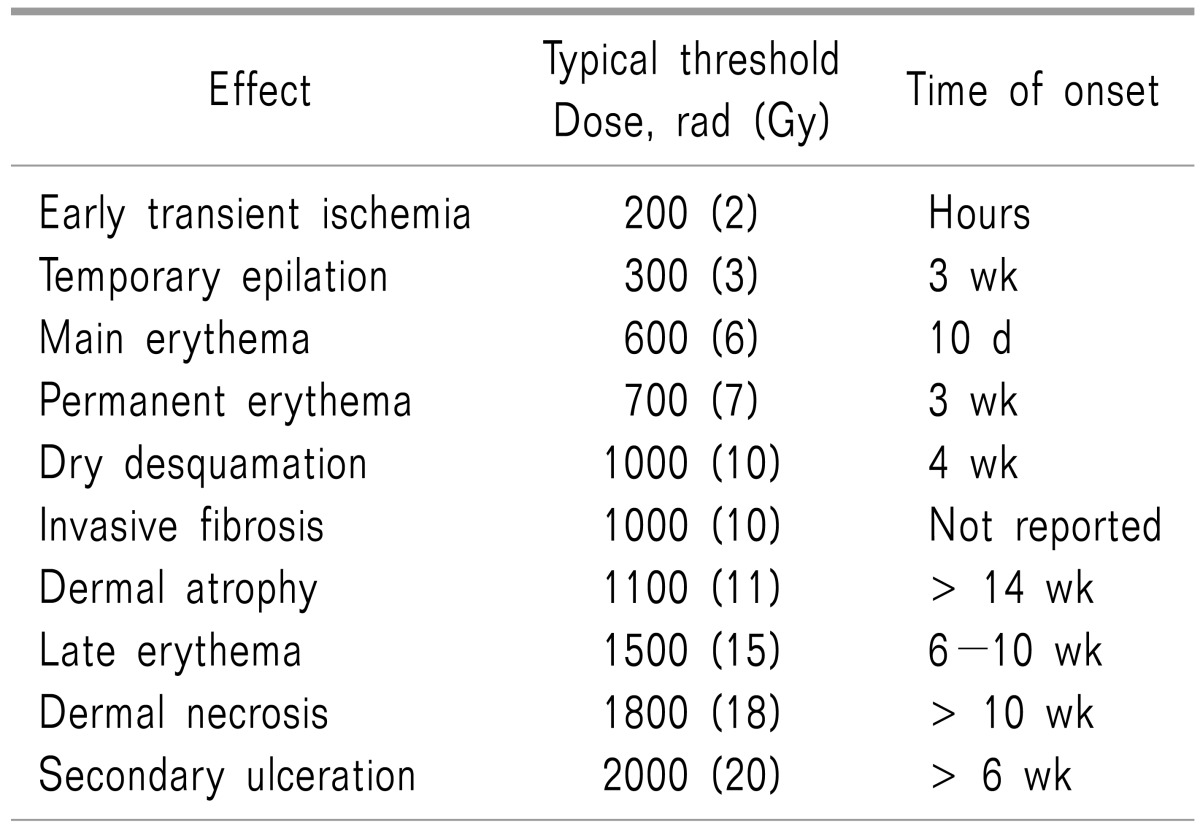
In comparing the 2011 and 2016 surveys, the degree of using low dose mode and pulsed mode was increased significantly in the 2016 survey (Table 5). And the number of pain physicians who know the major radiation exposure source had also significantly increased. Seventy-three percent of respondents found it is necessary to check for damage to radiation protective garments and the number of physicians who check was actually increased. Radiation can have a detrimental effect on pain physicians who use C-arm fluoroscopy. The extent of the adverse effects of radiation on the human body correspond to the amount of accumulated radiation [18]. Those adverse effects appeared in parenchymal cells, structural cells, and vascular tissue. Continuous radiation exposure to the skin can result in erythema, blistering, ulceration, and necrosis. The radiation threshold dose and skin manifestations are shown in the Table 6 [19]. However, physicians cannot see their accumulation of radiation exposure. The radiation can also induce cataracts and many types of cancer. Radiation-induced cancer occurs more in the skin, gastrointestinal tract, lungs, breast, and thyroid [2021]. Therefore, protection and checking radiation exposure are important to physicians. The percentage using a dosimeter increased significantly from 7% of physicians in 2011 to 39% in 2016. However, there was no significant difference in the various efforts at radiation protection and radiation safety knowledge.
In regard to radiation safety education, 9 (33%) out of 27 physicians had received it in 2011, and 19 (39%) out of 49 physicians in 2016. Respondents received radiation safety education at their working hospital and workshops put on by the Korean Pain Society. When the radiation safety education group and non-education group were compared, there was no significant difference in radiation safety knowledge and efforts to reduce radiation exposure (P > 0.05) (Table 4). This shows that education does not lead to the practice of radiation safety. So pain physicians appear not to have been attentive during their radiation safety education. Forty-two percent of educated pain physicians received radiation safety training at workshops of the Korean Pain Society, and 46% of educated physicians received radiation safety training at their working hospital. But there were no lectures on radiation safety during the 60th and 61st conferences of the Korean Pain Society held in 2015. At the workshop of the Korean Pain Society held in 2015, there was a C-arm fluoroscopy workshop which covered radiation protection equipment in only about 10 minutes, and their wearing demonstrations for a total of one hour of the lecture. The short time of the training may not influence the physician's practice of radiation safety. Pain physicians who are preparing to become experts in pain medicine should participate in the Cadaver Workshop, however there were no lectures about radiation safety in this workshop. Therefore, radiation safety related lectures should be prepared for the Cadaver Workshop, conference, or other workshops of the Korean Pain Society. If it is possible, a radiation safety manual should be created, and pain specialists should be able to implement this manual within the Korean Pain Society.
Radiation exposure dose is affected depending on the complexity of the procedure, the experience of the physician, and the degree of radiation safety training. Therefore, the need to receive radiation safety education is as important as learning fluoroscopic procedure for pain physicians. Regular education and practical training in radiation protection are most important in reducing radiation exposure [121317]. In general, American radiologists receive proper training in performing fluoroscopy, and are certified by the American Board of Radiology with the completion of their residency [22]. And interventional cardiologists must pass an examination which include radiation physics and radiation safety to obtain board certification in the USA [23]. And radiation safety regulation for physicians using fluoroscopy is done according to the capacity of the individual states in the USA. Some states require physicians who use fluoroscopy to obtain their credential to perform fluoroscopy. Depending on the state, the qualifications are slightly different, but physicians must receive radiation physics and radiation safety education and complete a test. And physicians should be trained regularly to maintain eligibility [22]. Similarly, radiation safety education and a radiation safety test should be mandatory for pain physicians who are preparing experts in pain medicine within the Korean Pain Society. Existing pain specialists should also be encouraged to be received radiation safety education. And pain specialists are also obligated to use a dosimeter and regularly check for doses radiation exposure.
There are some limitations to this study. In order to clearly compare the effect of radiation safety education, the survey should have included items asking if the respondent's hospital has adequate radiation protection equipment, such as goggles, thyroid collars, aprons, gloves, lead-acrylic protectors and dosimeters. The reason for low utilization of radiation protective equipment and dosimeters may be that the hospital was not fully equipped, and thus the equipment could not be used by respondents. If there are not enough radiation protective garments in a hospital, it is important to procure enough equipment for the safety of their physicians.
Most respondents in this survey were fellowship trainers. In the near future, similar research on general pain physicians, including the staff of university hospitals, will be helpful in recognizing the actual state of radiation safety awareness in Korea's pain physicians.
In conclusion, all pain physicians used C-arm fluoroscopy during pain intervention and worried about adverse effect due to radiation exposure. Nevertheless, they seem to lack knowledge of radiation safety. The rate of physicians receiving radiation safety education was low, and education does not lead to proper practice. Therefore, pain physicians should receive regular radiation safety education, and the education should be mandatory. At the Korean Pain Society, the number of lectures and education time related to radiation safety should be increased, and a radiation protection manual should be provided and implemented.
References
1. Sheyn DD, Racadio JM, Ying J, Patel MN, Racadio JM, Johnson ND. Efficacy of a radiation safety education initiative in reducing radiation exposure in the pediatric IR suite. Pediatr Radiol. 2008; 38:669–674. PMID: 18414841.

2. Kim S, Shin JH, Lee JW, Kang HS, Lee GY, Ahn JM. Factors affecting radiation exposure during lumbar epidural steroid injection: a prospective study in 759 patients. Korean J Radiol. 2016; 17:405–412. PMID: 27134528.

3. Fishman SM, Smith H, Meleger A, Seibert JA. Radiation safety in pain medicine. Reg Anesth Pain Med. 2002; 27:296–305. PMID: 12016604.

4. Broadman LM, Navalgund YA, Hawkinberry DW 2nd. Radiation risk management during fluoroscopy for interventional pain medicine physicians. Curr Pain Headache Rep. 2004; 8:49–55. PMID: 14731383.

5. Schueler BA. Operator shielding: how and why. Tech Vasc Interv Radiol. 2010; 13:167–171. PMID: 20723831.

6. Ryu JS, Baek SW, Jung CH, Cho SJ, Jung EG, Kim HK, et al. The survey about the degree of damage of radiation-protective shields in operation room. Korean J Pain. 2013; 26:142–147. PMID: 23614075.

7. Cho JH, Kim JY, Kang JE, Park PE, Kim JH, Lim JA, et al. A study to compare the radiation absorbed dose of the C-arm fluoroscopic modes. Korean J Pain. 2011; 24:199–204. PMID: 22220241.

8. Baek SW, Ryu JS, Jung CH, Lee JH, Kwon WK, Woo NS, et al. A randomized controlled trial about the levels of radiation exposure depends on the use of collimation C-arm fluoroscopic-guided medial branch block. Korean J Pain. 2013; 26:148–153. PMID: 23614076.

9. Kim AN, Chang YJ, Cheon BK, Kim JH. How effective are radiation reducing gloves in C-arm fluoroscopy-guided pain interventions? Korean J Pain. 2014; 27:145–151. PMID: 24748943.

10. Park PE, Park JM, Kang JE, Cho JH, Cho SJ, Kim JH, et al. Radiation safety and education in the applicants of the final test for the expert of pain medicine. Korean J Pain. 2012; 25:16–21. PMID: 22259711.

11. Cousins C, Sharp C. Medical interventional procedures-reducing the radiation risks. Clin Radiol. 2004; 59:468–473. PMID: 15145716.

12. Ploussi A, Efstathopoulos EP. Importance of establishing radiation protection culture in radiology department. World J Radiol. 2016; 8:142–147. PMID: 26981223.

13. Mahajan A, Samuel S, Saran AK, Mahajan MK, Mam MK. Occupational radiation exposure from C arm fluoroscopy during common orthopaedic surgical procedures and its prevention. J Clin Diagn Res. 2015; 9:RC01–RC04.

14. Wagner M, Duwenkamp C, Ludwig W, Dresing K, Bott OJ. An approach to simulate and visualize intraoperative scattered radiation exposure to improve radiation protection training. Stud Health Technol Inform. 2010; 160:625–628. PMID: 20841762.
15. Yamashita K, Higashino K, Wada K, Morimoto M, Abe M, Takata Y, et al. Radiation exposure to the surgeon and patient during a fluoroscopic procedure: how high is the exposure dose? A cadaveric study. Spine (Phila Pa 1976). 2016; 41:1254–1256. PMID: 26953671.
16. Meisinger QC, Stahl CM, Andre MP, Kinney TB, Newton IG. Radiation protection for the fluoroscopy operator and staff. AJR Am J Roentgenol. 2016; [in press].

17. Zhou Y, Singh N, Abdi S, Wu J, Crawford J, Furgang FA. Fluoroscopy radiation safety for spine interventional pain procedures in university teaching hospitals. Pain Physician. 2005; 8:49–53. PMID: 16850042.
18. Nicol AL, Benzon HT, Liu BP. Radiation exposure in interventional pain management: we still have much to learn. Pain Pract. 2015; 15:389–392. PMID: 26037659.

19. Frazier TH, Richardson JB, Fabré VC, Callen JP. Fluoroscopy-induced chronic radiation skin injury: a disease perhaps often overlooked. Arch Dermatol. 2007; 143:637–640. PMID: 17515515.
20. Mettler FA Jr, Koenig TR, Wagner LK, Kelsey CA. Radiation injuries after fluoroscopic procedures. Semin Ultrasound CT MR. 2002; 23:428–442. PMID: 12509113.

22. Killewich LA, Singleton TA. Governmental regulations and radiation exposure. J Vasc Surg. 2011; 53:44S–46S. PMID: 20875710.

23. Chambers CE, Fetterly KA, Holzer R, Lin PJ, Blankenship JC, Balter S, et al. Radiation safety program for the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 2011; 77:546–556. PMID: 21254324.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download