Abstract
Background
Recently, there have been several case reports and retrospective studies about the incidence of intradiscal (ID) injection during transforaminal epidural steroid injection (TFESI). Inadvertent ID injection is not a rare complication, and it carries the risk of developing diskitis, although there has been no report of diskitis after TFESI. We prospectively evaluated the incidence of inadvertent ID injection during lumbar TFESI and analyzed the contributing factors.
Methods
Ten patients received 2-level TFESI, and the remaining 229 patients received 1-level TFESI. When successful TFESI was performed, 2 ml of contrast dye was injected under real-time fluoroscopy to check for any inadvertent ID spread. A musculoskeletal radiologist analyzed all magnetic resonance images (MRIs) of patients who demonstrated inadvertent ID injection. When reviewing MRIs, the intervertebral foramen level where ID injection occurred was carefully examined, and any anatomical structure which narrowing the foramen was identified.
Results
Among the 249 TFESI, we identified 6 ID injections; thus, there was an incidence of 2.4%. Four patients had isthmic spondylolisthesis, and the level of spondylolisthesis coincided with the level of ID injection. We further examined the right or left foramen of the spondylolisthesis level and identified the upward migrated disc material that was narrowing the foramen.
Transforaminal epidural steroid injection (TFESI) is one of the most widely used interventional treatment for the relief of radicular pain secondary to lumbar spinal stenosis, lumbar discogenic disease, or failed back surgery syndrome. The mechanism of treatment is believed to be the attenuation of inflammation around the irritated nerve root [1,2]. Moreover, TFESI has the benefit of delivering therapeutic medication closer to the ventral epidural space, which is known to have abundant pain substances [3,4]. In spite of these therapeutic advantages, inadvertent intradiscal (ID) injection can occur not infrequently during TFESI.
In our previous report [5], we demonstrated an incidence of inadvertent ID injection during TFESI of 2.3%, higher than the results reported by Candido et al. [6] and Plastaras et al. [7].
Inadvertent ID injection is not a rare complication, and it carries the risk of developing diskitis, although there has been no report of diskitis after TFESI. Therefore, a thorough understanding of contributing factors of inadvertent ID injection is important.
Plastaras et al. [7] reported that the most common findings in inadvertent ID injection cases were ipsilateral foraminal stenosis (60%), central stenosis (26.7%), and spondylolisthesis (20%). They suggested that ipsilateral foraminal stenosis is a factor associated with inadvertent ID injection. However, their study had a retrospective design covering the period July 2000 to May 2008, and they obtained data from electronic archives and databases of operation notes; thus, there was the risk of missing much relevant data. Moreover, in their review of radiographic findings for each ID injection, they used radiology reports and did not perform an independent review of the magnetic resonance imaging. For those reasons, although they found an association between inadvertent ID injection and ipsilateral foraminal stenosis, they could not suggest the exact cause of foramen narrowing. In contrast to Plastaras et al. [7], Cohen et al. [8] reported that far lateral disc herniation might be a cause of ID injection.
In this study, we prospectively evaluated the incidence of inadvertent ID injection during lumbar TFESI and analyzed the contributing factors.
This study was approved by the ethics committee of our institution, and written informed consent was obtained from all patients after the risks, benefits, and goals of the study were explained to them. From October 2012 to July 2013, 239 consecutive patients were enrolled and received 249 fluoroscopically-guided TFESI.
Ten patients received 2-level TFESI, and the remaining 229 patients received 1-level TFESI. Inclusion criteria were patients who had low back pain with radicular leg pain from spinal stenosis, herniated nucleus pulposus, compression fracture, or failed back surgery syndrome. Exclusion criteria were patients with known allergies to contrast dye or local anesthetics or patients with active coagulopathy. Patients who received either interlaminar or caudal epidural injections were excluded.
TFESI was performed during outpatient care by one of the authors with more than 8 years of experience in interventional pain management. The patients were prepared and draped in a sterile fashion in a prone position. The TFESI was performed by targeting the six-o'clock position of the pedicle in the anteroposterior projection. The targeted segmental level was identified under intermittent fluoroscopy, and the inferior endplate was aligned by adjusting the C-arm angle craniocaudally. Then, the C-arm was rotated obliquely to visualize the neural foramen. Following strict sterile preparation, the skin entry site was infiltrated with 1% lidocaine. A 25-gauge Quincke spinal needle was advanced under fluoroscopic guidance toward the six-o'clock position of the pedicle. Lateral radiographic imaging was also used while advancing the needle toward the intervertebral foramen and superolateral to the exiting spinal nerve, and special care was taken to minimize the risk of ID puncture. Up to 2 ml of contrast dye (Omnipaque 300, GE Healthcare, Little Chalfont, Buckinghamshire, UK) was used to confirm successful epidural spread. Two ml of contrast dye was injected under real-time fluoroscopy to check for any inadvertent ID spread. All injections were assessed by another physician who did not perform the TFESI, and the findings were confirmed again immediately after the procedure by reviewing stored images.
With the appearance of successful epidural contrast spread without any inadvertent intravascular or ID spread, a mixture of 5 mg of dexamethasone and 3 ml of 0.5% mepivacaine was injected. In cases where inadvertent ID injection was observed, needle repositioning was repeated two or three times if necessary. If an ID contrast pattern still remained, the needle tip was withdrawn slowly and repositioned more superiorly within the neural foramen. Patients who showed ID dye appearance were given intravenous antibiotics (cefazolin, 1 gm). Once a satisfactory epidural spread pattern was observed, the treatment medication was injected. When an ID injection was unavoidable in spite of repeated attempts at needle repositioning, injecting any medication at that level was abandoned.
The collected data included patient demographics, dominant symptoms for TFESI, history of spine surgery, radiographic findings, presence of accidental ID injection based on real-time fluoroscopic images, patient perception of improvement, spinal levels at which TFESI was performed, and any other complications. A musculoskeletal radiologist analyzed all magnetic resonance images (MRIs) and simple lumbar spine X-rays of patients who demonstrated inadvertent ID injections. When reviewing MRIs, the intervertebral foramen level where ID injection occurred was carefully examined, and any anatomical structure which narrowing the foramen was identified. Also, the incidence of ID injection with lumbar TFESI was calculated.
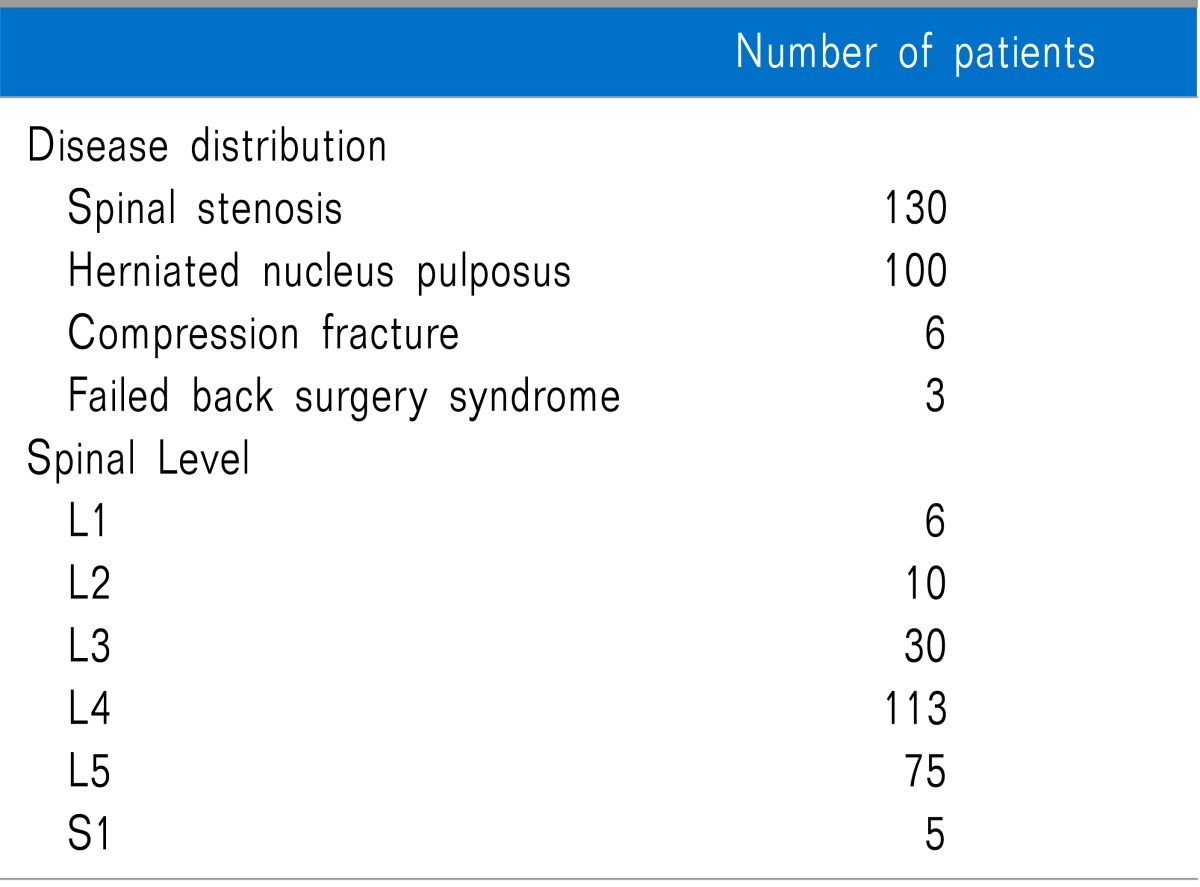
A total of 249 TFESI were performed with 239 patients having a mean age of 62.5 years (range: 26-90 years).
Ten patients received 2-level TFESI, and each injection was considered a separate procedure for our analyses; the remaining 229 patients received 1-level TFESI. Among those injections, 120 were on patients' right sides, and 129 were on the patients' left sides. One hundred thirty patients were diagnosed with spinal stenosis, 100 patients with herniation of the nucleus pulposus, 6 patients with compression fractures, and 3 patients with failed back surgery syndrome.
The sites of TFESI were between the L1 and S1 spinal levels. The most frequently injected levels were L4 (113 cases) and L5 (75 cases) (Table 1).
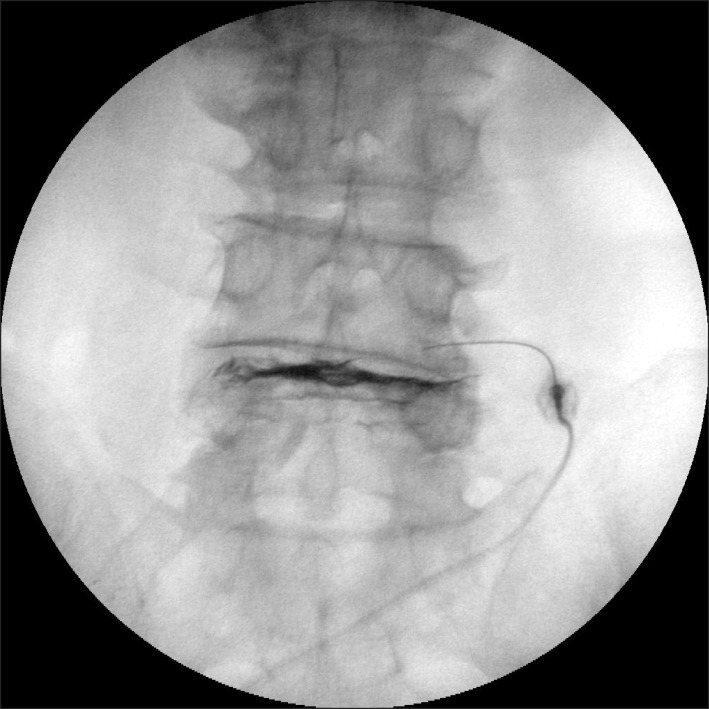
Among the 249 TFESI, we could identify 6 ID injections (Fig. 1), with an incidence of 2.4%.
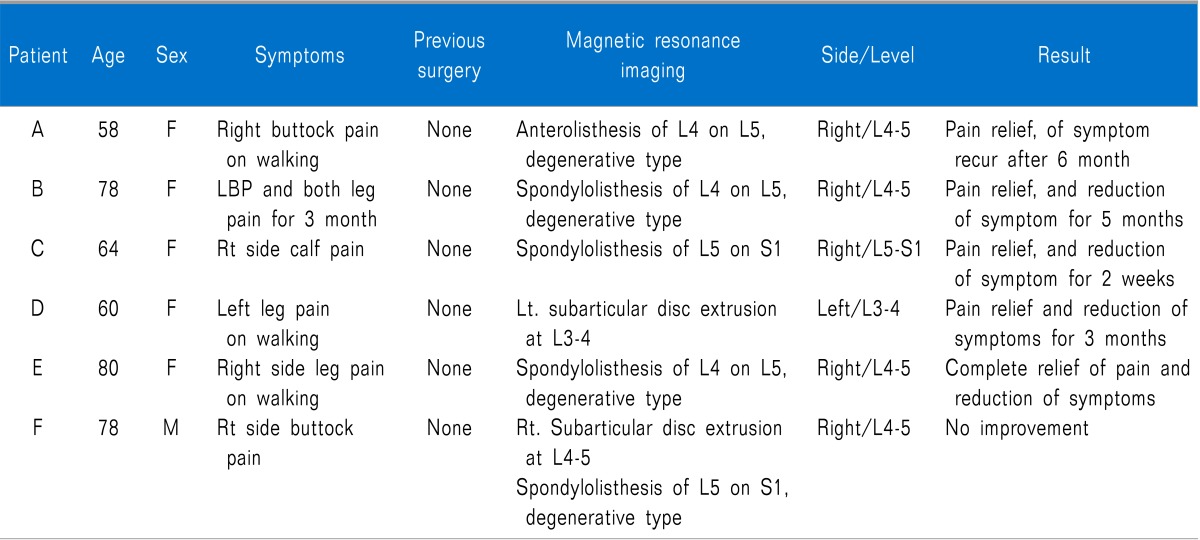
Among the six patients with ID injection, four had TFESI at the L4-5 level, and the remaining two had TFESI at the L5-S1 and L3-4 levels, respectively. No patients had a history of prior spine surgery.
We analyzed all MRIs of patients who showed ID injection. Four patients had isthmic spondylolisthesis and the level of spondylolisthesis coincided with the level of ID injection (Table 2). We further examined the right or left foramen of the spondylolisthesis level and identified the upward migrated disc material in each of the four patients (Fig. 2). The remaining two patients had subarticular disc herniation without spondylolisthesis.
In this prospective study, the overall incidence of ID injection was 2.4%, similar to our previous report [5]. Our incidence of ID injection is nearly 10 times higher than that reported by Candido et al. [6] (0.25%). This large discrepancy may be attributed to other studies' underestimation of the ID injection rate and the fact that retrospective studies are limited in their ability to probe complications uniformly. According to our study, inadvertent ID injection during TFESI is not very rare, and pain physicians performing TFESI must be aware of this potential complication and take steps to prevent and minimize the complication.
Among the six patients with ID injections, four had isthmic spondylolisthesis at the level of TFESI, and we tried to determine why ID injection is easily observed in patients with spondylolisthesis. Lumbar degenerative spondylolisthesis is typically characterized by the forward slippage of a vertebra causing spinal instability and stenosis [9]. Significant morphological and anatomical changes can occur to the spinal canal and intervertebral foramen due to the slippage of superior vertebrae to below vertebra. This leads to symptoms of spinal stenosis, which induces low back pain, radicular lower leg pain and neurogenic claudication [10]. It is well known that the pathognomonic change of degenerative spondylolisthesis starts with disc degeneration, followed by ligamentum flavum hypertrophy and facet laxity, which results in severe spinal stenosis with or without intervertebral disc herniation at the level of spondylolisthesis [9,10]. In isthmic spondylolisthesis, pseudodisc bulging is easily identified, and central canal stenosis is rare. As the slippage occurs mostly at the L4-5 intervertebral disc level, the disc material often protrudes to the intervertebral foramen of the spondylolisthesis level [10,11]. Kim et al. [11] reported that 38 out of 120 (31.7%) patients with isthmic spondylolisthesis had pseudodisc bulging with disc herniation, and among those 38 patients, 25 (65.8%) had foraminal and extraforaminal disc herniation.
Natarajan et al. [12] proposed that the stress loaded on the annulus fibrosus increases as the degree of the slippage increases in spondylolisthesis and this results in disc degeneration with reduction in the stiffness of the annuls fibrosus. In the upright position, the maximal stress usually occurs near the outer edge of the annulus. Therefore, abnormal loading with increased disc stress at the posterolateral part of the annulus and decreased disc stiffness might be one cause of foraminal disc herniation in isthmic spondylolisthesis. The foraminal disc herniation frequently found in isthmic spondylolisthesis might contribute to inadvertent ID injection during lumbar TFESI.
Moon et al. [13] reported 2 cases of inadvertent discogram during lumbar TFESI, and both cases had foraminal disc herniation. The authors concluded that ID injection may have occurred due to intervertebral disc herniation into the superior foramen where the needle was advancing. Cohen et al. [8] suggested that inadvertent ID injection is most likely attributable to far lateral disc herniation and that the degenerated annular fiber may make a neighboring pathway to the epidural space, allowing the contrast agent or medication to move in intradiscally. Plastaras et al. [7] proposed that as the severely degenerated vacuum disc generates the negative pressure of ID space, ultimately, this pressure gradient between ID space and the epidural space might pull the contrast dye from the epidural space into the disc.
Migration of extruded disc material within the spinal canal can take place in any direction, rostrally or caudally into the lateral recess and foraminal or extraforaminal in the horizontal plane. In the horizontal plane, central, paracentral, subarticular, foraminal, and extraforaminal migrations were reported in 17.3%, 74.2%, 4.3%, 2.5%, and 1.8% of patients, respectively [14]. If epidural injection via the transforaminal technique is planned, pain physicians must pay close attention to subarticular, foraminal, and extraforaminal disc herniation, and perform strict evaluation of the intervertebral foramen by reviewing the MRI film. In addition, adjustments in needle location and direction should be considered according to the extent and location of the herniated disc after reviewing the MRI. Considering the interlaminar technique rather than the transforaminal technique might be one method to reduce inadvertent ID injection. According to Candido et al. [6], the incidence of ID injection was significantly lower with the interlaminar technique than with the transforaminal technique.
Many pain physicians choose the transforaminal technique rather than the interlaminar technique due to its advantage of easy delivery of medication to the anterior epidural space. However, parasagittal interlaminar epidural injection is effective in delivering medication to the anterior epidural space and has proven therapeutic efficacy. Candido et al. [15] reported that 100 % (29/29) of patients in a parasagittal interlaminar group and 75% (21/29) of patients in a transforaminal group demonstrated anterior epidural spreading. Ghai et al. [16] reported that the lateral parasagittal technique was significantly more effective than the midline approach for pain relief and improvement in disability in the management of low back pain with radicular leg pain.
Carragee et al. [17] demonstrated that modern discography techniques with limited pressurization resulted in accelerated disc degeneration, disc herniation, loss of disc height, and loss of signal intensity compared to matched control group. The most serious complication following inadvertent ID injection is diskitis, which poses the problems of refractoriness to management and the potential for permanent neurological sequelae [18]. No studies have examined the development of diskitis after inadvertent disc entry during TFESI. In our study, none of the six inadvertent ID injections resulted in infection. The prophylactic use of antibiotics in discography has been supported [18], and in cases of inadvertent ID injection during TFESI, preventive use of antibiotics is recommended.
Our study has several limitations. As there were only six cases of inadvertent ID injections during TFESI in our study, concluding that spondylolisthesis a contributing factor is difficult. Although these six patients did not show any sign of infection, long-term follow up was not performed.
In conclusion, inadvertent ID injections during TFESI is not infrequent. Before pain physicians perform TFESI, they must pay close attention to the type and location of disc herniation. If TFESI is planned in patients with spondylolisthesis, pain physicians should confirm whether foraminal disc herniation is also present.
References
1. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013; 38:175–200. PMID: 23598728.
2. McCormick Z, Plastaras C. Lumbosacral transforaminal epidural steroid injections are equally effective for treatment of lumbosacral radicular pain in the obese compared to non-obese population: a pilot study. J Back Musculoskelet Rehabil. 2013; 26:183–188. PMID: 23640320.

3. Kaufmann TJ, Geske JR, Murthy NS, Thielen KR, Morris JM, Wald JT, et al. Clinical effectiveness of single lumbar transforaminal epidural steroid injections. Pain Med. 2013; 14:1126–1133. PMID: 23895182.

4. Ploumis A, Christodoulou P, Wood KB, Varvarousis D, Sarni JL, Beris A. Caudal vs transforaminal epidural steroid injections as short-term (6 months) pain relief in lumbar spinal stenosis patients with sciatica. Pain Med. 2014; 15:379–385. PMID: 24341966.

5. Hong JH, Kim SY, Huh B, Shin HH. Analysis of inadvertent intradiscal and intravascular injection during lumbar transforaminal epidural steroid injections: a prospective study. Reg Anesth Pain Med. 2013; 38:520–525. PMID: 24141875.

6. Candido KD, Katz JA, Chinthagada M, McCarthy RA, Knezevic NN. Incidence of intradiscal injection during lumbar fluoroscopically guided transforaminal and interlaminar epidural steroid injections. Anesth Analg. 2010; 110:1464–1467. PMID: 20418306.

7. Plastaras CT, Casey E, Goodman BS, Chou L, Roth D, Rittenberg J. Inadvertent intradiscal contrast flow during lumbar transforaminal epidural steroid injections: a case series examining the prevalence of intradiscal injection as well as potential associated factors and adverse events. Pain Med. 2010; 11:1765–1773. PMID: 20807341.

8. Cohen SP, Maine DN, Shockey SM, Kudchadkar S, Griffith S. Inadvertent disk injection during transforaminal epidural steroid injection: steps for prevention and management. Pain Med. 2008; 9:688–694. PMID: 18657222.

9. Miao J, Wang S, Park WM, Xia Q, Fang X, Torriani MP, et al. Segmental spinal canal volume in patients with degenerative spondylolisthesis. Spine J. 2013; 13:706–712. PMID: 23541448.

10. Sengupta DK, Herkowitz HN. Degenerative spondylolisthesis: review of current trends and controversies. Spine (Phila Pa 1976). 2005; 30:S71–S81. PMID: 15767890.
11. Kim KS, Chin DK, Park JY. Herniated nucleus pulposus in isthmic spondylolisthesis: higher incidence of foraminal and extraforaminal types. Acta Neurochir (Wien). 2009; 151:1445–1450. PMID: 19499170.

12. Natarajan RN, Garretson RB 3rd, Biyani A, Lim TH, Andersson GB, An HS. Effects of slip severity and loading directions on the stability of isthmic spondylolisthesis: a finite element model study. Spine (Phila Pa 1976). 2003; 28:1103–1112. PMID: 12782976.

13. Moon HS, Shin BC, Im HS, Song BH, Cha YD. Inadvertent discogram during transforaminal epidural injection in patients with lumbar disc herniation -A report of 2 cases-. Korean J Anesthesiol. 2010; 58:104–108. PMID: 20498821.

14. Daghighi MH, Pouriesa M, Maleki M, Fouladi DF, Pezeshki MZ, Mazaheri Khameneh R, et al. Migration patterns of herniated disc fragments: a study on 1,020 patients with extruded lumbar disc herniation. Spine J. 2013; in press.

15. Candido KD, Raghavendra MS, Chinthagada M, Badiee S, Trepashko DW. A prospective evaluation of iodinated contrast flow patterns with fluoroscopically guided lumbar epidural steroid injections: the lateral parasagittal interlaminar epidural approach versus the transforaminal epidural approach. Anesth Analg. 2008; 106:638–644. table of contents. PMID: 18227326.

16. Ghai B, Vadaje KS, Wig J, Dhillon MS. Lateral parasagittal versus midline interlaminar lumbar epidural steroid injection for management of low back pain with lumbosacral radicular pain: a double-blind, randomized study. Anesth Analg. 2013; 117:219–227. PMID: 23632053.

17. Carragee EJ, Don AS, Hurwitz EL, Cuellar JM, Carrino JA, Herzog R. 2009 ISSLS Prize Winner: does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine (Phila Pa 1976). 2009; 34:2338–2345. PMID: 19755936.

18. Cohen SP, Larkin TM, Barna SA, Palmer WE, Hecht AC, Stojanovic MP. Lumbar discography: a comprehensive review of outcome studies, diagnostic accuracy, and principles. Reg Anesth Pain Med. 2005; 30:163–183. PMID: 15765459.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download