Abstract
Background
The precise knowledge of anatomy and the region of transverse process (TP) and superior articular processes (AP) and their distance from the skin are important in blocking and treating lumbar facet syndrome. Evaluation of these anatomic distances from 3rd and 5th lumbar vertebrae in both sides and in different body mass index (BMI) in healthy volunteers might improve knowledge of ultrasound (US) lumbar medial branch nerve blocks (LMBB).
Methods
Bilateral US in the 3rd and 5th lumbar vertebrae of 64 volunteers carried out and the distance between skin to TP and skin to AP was measured. These distances were compared on both sides and in different BMI groups. The analysis was done using SPSS 11. Analysis of variance was used to compare the means at three vertebral levels (L3-L5) and different BMI groups. P values less than 0.05 were considered statistically significant. The paired t-test was used to compare the mean distance between skin to TP and skin to AP on both sides.
Results
The distance between skin to TP and skin to AP of 3rd vertebrae to 5th vertebrae was increased in both right and left sides (P < 0.001) from up to down. The mean distance from skin to TP were greater on the left side compared to the right in all three vertebral levels from L3 to L5 (P values 0.014, 0.024, and 0.006 respectively). The mean distance from skin to TP and the skin to AP was statistically significant in different BMI groups (P < 0.001).
The precise knowledge of anatomy and the region of transverse process (TP) and articular processes (AP) and their distance from the skin are important in blocking and treating lumbar facet syndrome. Facet nerve block by anesthetizing the internal sub-branches of posterior branch of spinal nerve are a standard diagnostic method [1]. The nerve blockage of lumbar facet or medial branch nerve blocks (LMBB) is performed under fluoroscopy or computed tomography (CT) scan. In the early years, ultrasound (US) was used for facet joint injection [2]. US has a low risk and needs lesser time in comparison with computed tomography CT scan [3]. In 10-20% of the patients, the joint cannot be seen clearly due to hypertrophy and ossification of the joint, therefore facet nerve block is the preferred method that could be performed under guide of US. As the procedure is a low risk intervention, US is a good substitute for fluoroscopy, particularly because it does not involve any radiation exposure. Several papers have already shown that US can be used to perform these procedures at the level of the lower lumbar facet joints in patients with normal body mass index [2,3,4,5,6,7,8].
However, US is still in its early stages as an imaging modality for chronic back pain and its value has to be proven in diagnostic and standard treatment injections. There is no large survey to study sonanatomic distances of LMBB. There are only a few reports refer to these distances on cadaver and human [3,7,9]. The main objective of this study is to survey the distance of sonoanatomic landmarks for LMBB in healthy volunteers to improve this knowledge.
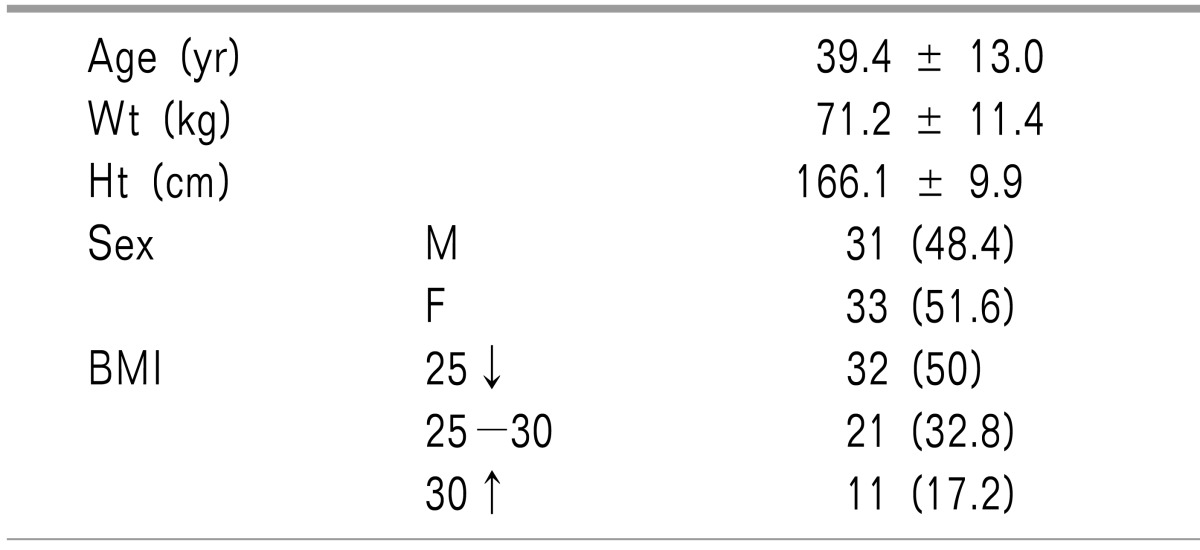
After acquiring ethics committee approval, 64 healthy volunteers were invited to participate in this study; oral informed patient consent has been getting from all the volunteers. Exclusion criteria included vertebrae deformity and maternal pregnancy. Weight, height and BMI were measured for all the participants.
By a 3-5 MHz curve probe (MicroMaxx, SonoSite, Inc, USA) bilateral US in the 3rd and 5th lumbar vertebrae was carried out. Patients had prone position and a pillow placed under the abdomen to lower the lumbar lordosis position. The L4 possible position marked by drawing a line between the two iliac crests. An adequate US gel applied on the skin and the lower and upper spinous process marked after careful palpation. (In cases, we could not find the spinous process through palpation, a US probe used in transverse position to identify the spinous process). A longitudinal scanning did from 3 cm of paramedian line of the spine. The numbers of TP counted from the highest mark to 5th vertebrae and sacrum. If it was three, all the marks confirmed and all the spinous process was marked. The probe rotated at 90 degrees and placed transversely on all 3 spinous processes. The TP and AP on both sides located by moving the probe in the caudal-capable position. We measured the distance between skin and AP from the skin to the most superficial aspect of the facet joint. Then the distance between the skin and TP and the possible location for blockade (at the bottom of the groove between the lateral surface of superior articular process and cephalic margin of the TP) measured. The same process repeated for every individual vertebra (Fig. 1, 2).
The analysis did by using SPSS 11. Volunteer's profiles were shown as median. A paired t-test used to compare the mean distance between skin to TP and skin to AP on both sides. Analysis of variance used to compare the means at three vertebral levels (L3-L5) and different BMI groups. P values less than 0.05 considered statistically significant.
Sixty four volunteers participated in this study. The demographic data are shown in Table 1. Para vertebrae US with a 3-5 MHz probe was possible in all patients (384 transverse views, 768 measurements). The distance between skin to TP and skin to AP from 3rd vertebrae to 5th vertebrae was increased on both sides from up to down (P < 0.001) (Fig. 3, Table 2).
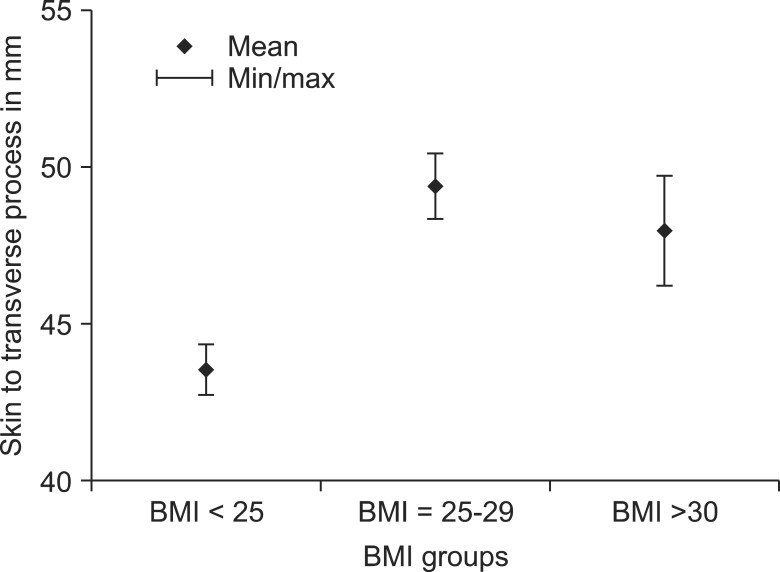
The mean distance from skin to TP were greater on the left side compared to the right in all three vertebral levels from L3 to L5 (P values are 0.014, 0.024, and 0.006 respectively) (Fig. 4). The mean distance from skin to TP and the skin to AP compared in different BMI groups. The difference was statistically significant (P < 0.001). The post hoc comparison using the Bonferroni method showed that the observed differences lie between the "less than 25" and the "25-29" (overweight) as well as the "less than 25" and the over 30 BMI (obese) groups. There was no significant difference between overweight and obese groups on either side (Fig. 5, Table 3). US quality was good in all. The US echogenic markers clearly show even in an obese patient with the BMI of 37.9.
The most important finding of this investigate is that distance from skin to TP and skin to AP was increased from L3 to L5 from up to down; by the way, this increase was not seen in 19 of 64 patients. Although the mean measured distance in overweight patients was more than average patients, there was no significant difference between overweight and obese groups. And, though the mean BMI was up to 37.9 in one patient, the quality of the image was good, it seems there are exceptions in some obese and echogenic markers are more superficial and therefore US images have good quality.
Studies had confirmed US guided paravertebrae intervention but locating the specific part can not be done without fluoroscope and contrast dye injection [5]. A US view of facet nerve block is able by essential echogenic markers of TP and AP. These structures must be seen during US guided block as we studied [10,11,12]. Despite other US nerve blockage that the nerve can be seen superficially, direct view of the facet nerve is not possible in the depth of 5 cm. The target point is 3 cm lateral to the midline and the most superficial part of the joint process is 1.5 cm closer to skin compare to target point. The depth of the target point had a little different on each side and increased from 3rd lumbar vertebrae (3.5 cm) to 5th vertebrae (5 cm) as our study [6].
According to Shim et al. [9] one hundred one needles were placed by US toward the lumbar segment under fluoroscope control, 96 needles were placed in the correct position and 2 injections had an IV distribution of the contrast agent. Pain score (VAS) dropped from 25 to 16. According to Rauch et al. [11] US was performed in overweight people, 84 blocks were performed in 20 people with BMI of over 30, the success rate was 60%. The distance between the skins to target point in TP was 76 mm. He also mentioned the depth difference of the skin in L4 and L5 as our study but in contrast to our study, he said that tracking of the needle was not possible and overall, LMBB cannot be performed in overweight people by the US. According to Greher et al. [6] US signs in 19 cases were good and in one case had not sufficient quality (maybe because the patient's BMI was 36). The distance from the skin to AP and skin to TP from L3 to L5 was gradually increased on both sides like our study, but he studied 20 cases compare with 64 cases of us and there was no discussion about left and right differences or the exceptions that we found. They approved US as a valuable tool and comparable with CT scan. The depth of skin to AP and skin to TP was measured and it was close to our data, in right side P = 0.027 and in the left was P = 0.005.
Greher [10] confirmed this method by CT scan and named the upper groove of TP below the facet as the target point. The injection was done in 45 cases at the target point. There were 5 cases in the external side of target point, 7 cases beside the foramen, 5 cases epidural and 2 cases intravenous, although all the needles were in target point by fluoroscopic imaging. This study showed that the US technique is valuable method and can be compared on the misdistributions of contrast agent with fluoroscopy. Moon et al. [12] confirmed availability of this method by magnetic resonance tomography (MRT).
According to Galiano et al. [3] CT scans and US was compared for LMBB on only 5 cadavers in contrast to our study in 64 normal volunteers, his study showed that these two techniques can be compared to availability. Longitudinally distance from skin to the spinous process and spinous process to facet joint was measured. However, he measured the distance between the spinous process to middle of facet in contrast to our study that we measured the distance between the skin and TP and the possible location for blockade.
Our hypothesis was that sonoanatomic distances could give us a clear understanding of how guiding needle and until which distances from skin, up to down in lumbar region. The outcomes of this study were compared sonoanatomic distances that are needed for MBB from L3 to L5 up to dawn and in left and right sides and comparing it in different BMI groups. It seems there are no limitations for this study because all the sonographies were performed by one person and by the same instrument.In summary, US guided LMBB has no limits in weight, it has even better quality in obese. Our result can improve awareness during the performance of US guided LMBB. The distance between the skin and TP in right and left side were differences in our study that is a new subject. Although the mean distance from skin to AP and skin to TP increased from L3-5, but this is not always expected and it is not a rule during the blockage. In obese patients although it is expected the blockage to be done deeper there are also some expectations and being obese is not a reason for poor quality.
US is used in early stages of chronic spinal pain management and has to prove its place in diagnose and treatments standard injections. This study may be used with clinical relevance and has potential to increase practicability while avoiding radiation.
References
1. Saal JS. General principles of diagnostic testing as related to painful lumbar spine disorders: a critical appraisal of current diagnostic techniques. Spine (Phila Pa 1976). 2002; 27:2538–2545. PMID: 12435989.

2. Fujiwara Y, Komatsu T, Gofeld M. Ultrasound-guided lumbar (L1-L4) zygapophysial medial branch and L5 dorsal ramus block. In : Bigeleisen P, Orebaugh S, Moayeri N, Groen G, Breneman S, Chelly J, editors. Ultrasound-guided regional anesthesia and pain medicine. Philadelphia (PA): Lippincott Williams & Wilkin;2010. p. 240–251.
3. Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med. 2007; 32:317–322. PMID: 17720116.

4. Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med. 2005; 24:33–38. PMID: 15615926.

5. Kirchmair L, Entner T, Wissel J, Moriggl B, Kapral S, Mitterschiffthaler G. A study of the paravertebral anatomy for ultrasound-guided posterior lumbar plexus block. Anesth Analg. 2001; 93:477–481. PMID: 11473883.

6. Greher M, Scharbert G, Kamolz LP, Beck H, Gustorff B, Kirchmair L, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004; 100:1242–1248. PMID: 15114223.
7. Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Ultrasound guidance for facet joint injections in the lumbar spine: a computed tomography-controlled feasibility study. Anesth Analg. 2005; 101:579–583. PMID: 16037179.

8. Irwin DM, Gofeld M. Ultrasound-guided lumbar zygapophysial (Facet) nerve block. In : Narouze SN, editor. Atlas of ultrasound-guided procedures in interventional pain management. New York (NY): Springer;2011. p. 149–156.
9. Shim JK, Moon JC, Yoon KB, Kim WO, Yoon DM. Ultrasound-guided lumbar medial-branch block: a clinical study with fluoroscopy control. Reg Anesth Pain Med. 2006; 31:451–454. PMID: 16952818.

10. Greher M, Kirchmair L, Enna B, Kovacs P, Gustorff B, Kapral S, et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology. 2004; 101:1195–1200. PMID: 15505456.
11. Rauch S, Kasuya Y, Turan A, Neamtu A, Vinayakan A, Sessler DI. Ultrasound-guided lumbar medial branch block in obese patients: a fluoroscopically confirmed clinical feasibility study. Reg Anesth Pain Med. 2009; 34:340–342. PMID: 19585701.
Fig. 1
Skin to articular process distance. SP: spinous process, AP: superior articular process, TP: transvers process.
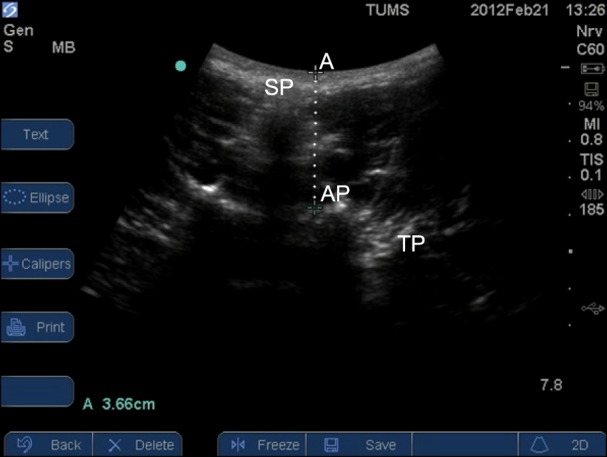
Fig. 2
Skin to transverse process distance. SP: spinous process, AP: superior articular process, TP: transvers process. *Site of injection.
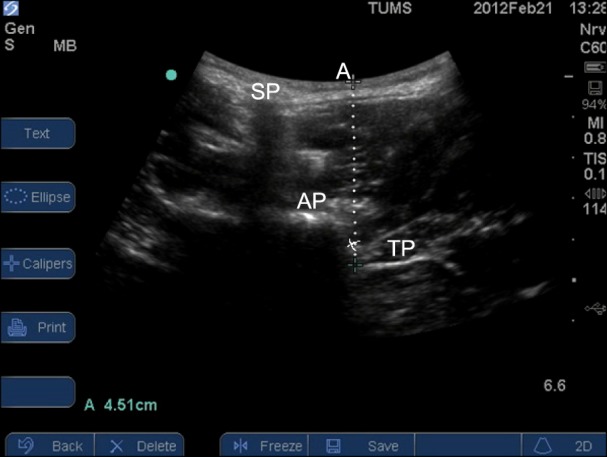
Fig. 3
Mean distances (mm) between skin and transverse processes (TPR &TPL) and skin and articular processes (APR & APL) by vertebral level (TPR: skin to transverse process at the right side, TPL: skin to transverse process at the left side, APR: skin to articular process at the right side. APL: skin to articular process at the left side).
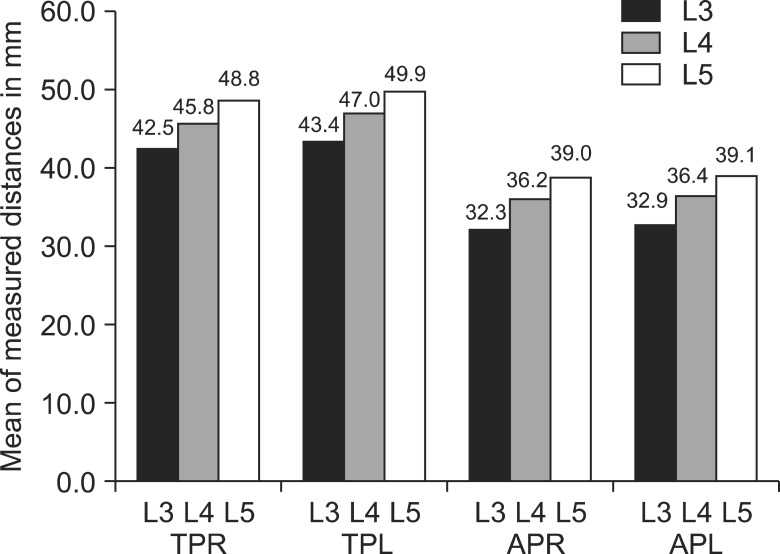
Fig. 4
Mean distances between skin and transverse processes (TPR &TPL) and skin and articular processes (APR & APL) by vertebral level highlighting the difference between left and right sides.
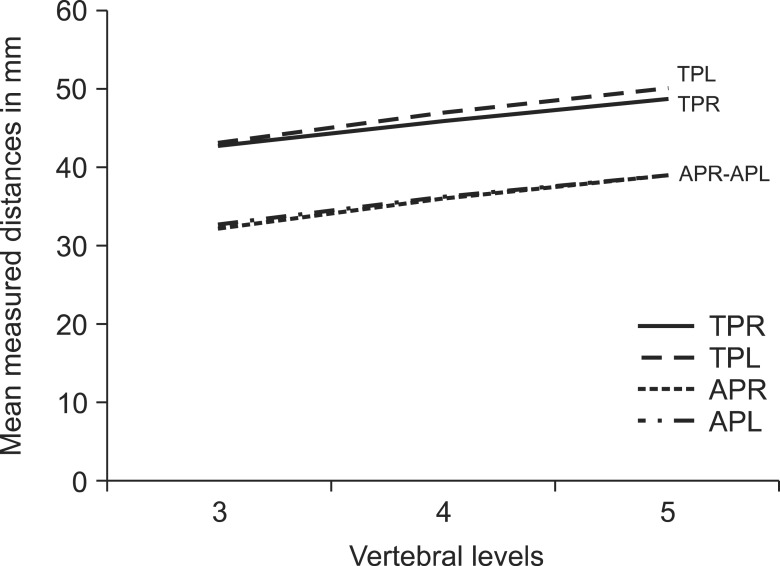
Table 2
Mean Distances (mm) between Skin to Transverse Processes (TPR &TPL) and Skin to Articular Processes (APR & APL) at Different Vertebral Levels
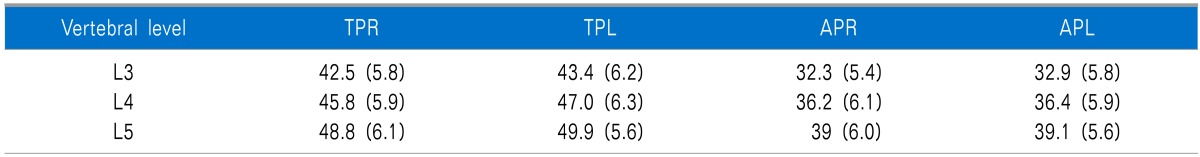
Table 3
Correlation between Distances and Body Mass Index at Different Vertebral Levels (L3 to L5)
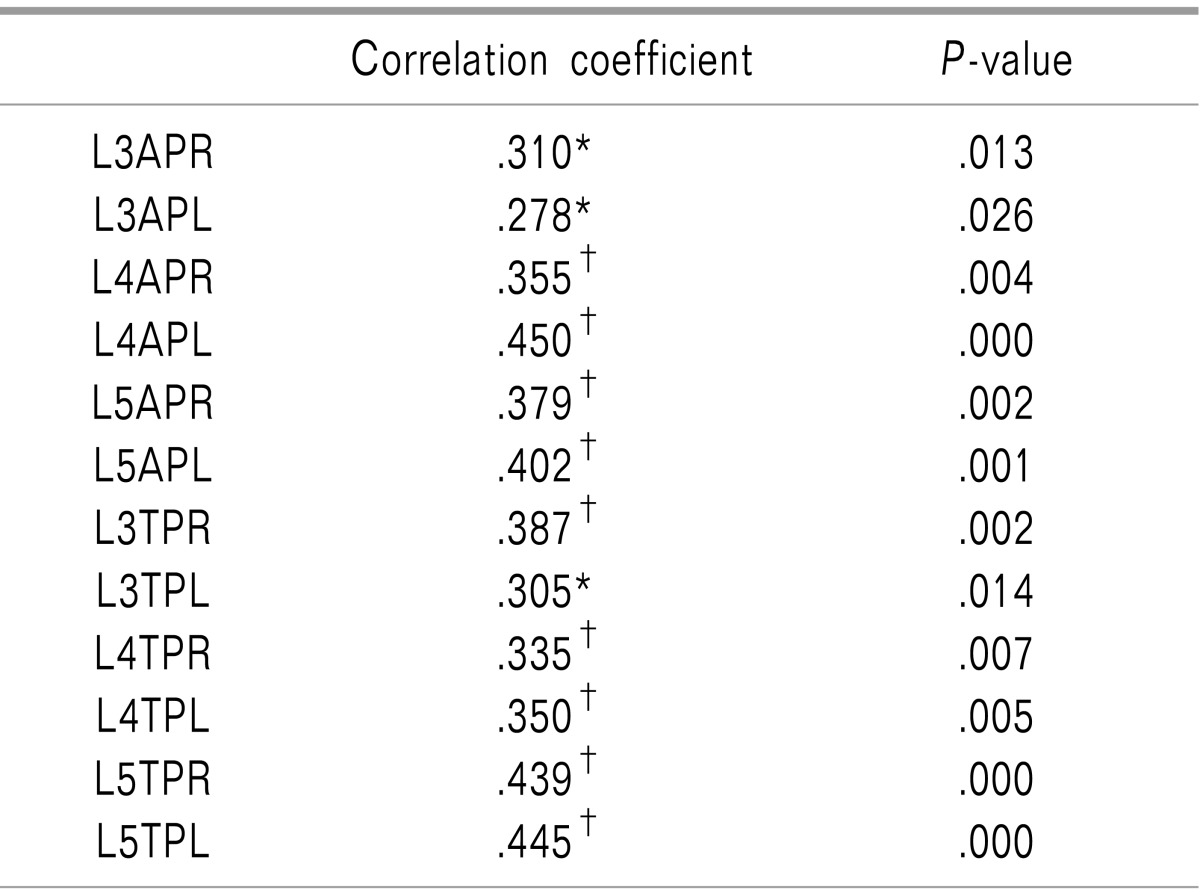
TPR: skin to transverse process at the right side, TPL: skin to transverse process at the left side, APR: skin to articular process at the right side, APL: skin to articular process at the left side. *Correlation is significant at the 0.05 level (2-tailed). †Correlation is significant at the 0.01 level (2-tailed).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download