Abstract
Postherpetic neuralgia (PHN) is a debilitating complication of herpes zoster, especially in elderly and comorbid patients. Unfortunately, the currently available treatments have shown limited efficacy and some adverse events that are poorly tolerated in elderly patients. Scrambler Therapy, proposed as an alternative treatment for chronic neuropathic pain recently, is a noninvasive approach to relieve pain by changing pain perception at the brain level. Here, we report our clinical experiences on the effect of Scrambler Therapy for three patients with PHN refractory to conventional treatment.
Postherpetic neuralgia (PHN) is a chronically painful sequel of acute herpes zoster and one of the difficult neuropathic pain syndromes to treat. Because several distinct pathophysiological mechanisms contribute to the pain from PHN, many physicians have to make an effort for an individualized approach to its management [1]. However, unfortunately, currently available treatments offer only partial pain relief to some patients with PHN and may be associated with adverse events that limit their use [2]. Scrambler Therapy is a noninvasive approach to pain control that interferes with pain signal transmission by providing non-pain information via patient-specific cutaneous electrostimulation [3]. Although randomized controlled studies for this therapy are not well established, it has been shown to be effective in relieving refractory chronic pain in some clinical trials [3-8]. Thus, Scrambler Therapy can be a new option for treating PHN. Here, we report our clinical experiences on the Scrambler Therapy, using an electro-analgesic device (MC5-A Calmare®, Competitive TechnologiesInc, USA) (Fig. 1), for three patients with PHN whose pain was poorly controlled by previous conventional treatments.
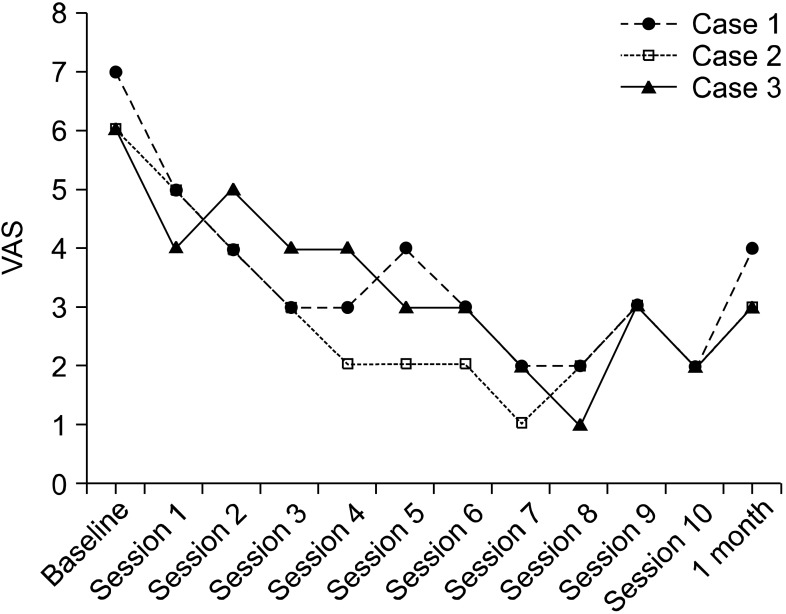
A 70-year-old woman visited our pain clinic with pain in the right scapular area around the T3 dermatome, which started 34 months ago. She suffered from constant burning and throbbing pain along with intermittent electric shock-like pain. She was diagnosed with PHN and began to take several oral medications including pregabalin 150 mg- and oxycodone 10 mg -twice a day, and nortriptyline 75 mg before sleep. Additionally, she had been treated with an epidural block, pulsed radiofrequency lesioning, intravenous lidocaine and ketamine infusion, etc. However, her symptoms were gradually aggravated in spite of all this and her pain was rated at an intensity of 7/10 on the visual analogue scales (VAS) from 0 (no pain) to 10 (worst pain imaginable). Thus, we considered the use of Scrambler Therapy for pain relief. With informed consent, we began to treat the patient (Fig. 2). It was programmed for a 50-minute daily treatment for 10 consecutive days. Before the Scrambler Therapy was initiated, the VAS score was 7/10 and total pain rating index (T-PRI) on the Short-Form Mcgill Pain Questionnaire (SF-MPQ) was 30/45. After the second treatment, the VAS score was 4/10 and T-PRI on the SF-MPQ was 20/45. Moreover, she reported that the electric shock-like pain decreased to a tolerable range. On the last day, the VAS score was 3/10 and T-PRI on the SF-MPQ was 19/45. In addition, the electric shock-like pain disappeared completely. During ten treatments, no side effects were reported. On the third day after the last treatment, she received one more therapeutic treatment for pain relief. From that day, the VAS score was maintained within the range of 3-4 for the next 2 weeks. Four weeks later, at the patient's follow up visit, the VAS score was 4.
A 75-year-old woman visited our pain clinic with pain around the right T5 dermatome, which started 16 months ago. She suffered from constant dull aching pain along with intermittent electric shock-like pain. She was diagnosed with PHN and began to take oral medications including pregabalin 75 mg twice a day, andnortriptyline 25 mg before sleep in our clinic. She was also being treated for Parkinson's disease. She did not want any further medication and invasive procedures. Thus, we treated her conservatively with local intralesional injection, laser therapy and so on. However, her symptoms became aggravated and the VAS score was 6/10. With the patient's informed consent, we started the Scrambler Therapy with a 50-minute daily treatment for 10 consecutive days. At the beginning, the VAS score was 6/10 and T-PRI on the SF-MPQ was 22/45. After the third treatment, the VAS score was 3/10 and T-PRI on the SF-MPQ was 7/45. Moreover, she reported that the electric shock-like pain decreased to a tolerable range. On the last day, the VAS score was 2/10 and T-PRI on the SF-MPQ was 3/45. In addition, the electric shock-like pain disappeared completely. From that day, the VAS score was maintained within the range of 2-3 for the next 2 weeks. Four weeks later, at the patient's follow-up visit, the VAS score was 3.
A 70-year-old woman visited our pain clinic with pain around the right L1 dermatome. She suffered from constantly burning and intermittently electric shock-like pain for 15 months. She had been diagnosed with PHN and began to take oral medications including pregabalin 75 mg twice a day, and nortriptyline 25 mg before sleep in our clinic. She was also being treated with anticoagulant therapy for ischemic heart disease, and was afraid of receiving invasive treatment. Thus we tried the Scrambler Therapy for pain relief. With the patient's informed consent, we started the Scrambler Therapy with a 50-minute daily treatment for 10 consecutive days. At the beginning, the VAS score was 6/10 and T-PRI on the SF-MPQ was 18/45. After the fifth treatment, the VAS score was 3/10 and T-PRI on the SF-MPQ was 5/45. Moreover, she reported that the electric shock-like pain decreased to a tolerable range. On the last day, the VAS score was 2/10 and T-PRI on the SF-MPQ was 3/45. In addition, the electric shock-like pain disappeared completely. On the fourth day after her last treatment, she received one more therapeutic treatment for pain relief. Since that day, the VAS score was maintained within the range of 2-3 for the next 2 weeks. Four weeks later, at the patient's follow-up visit, the VAS score was 3.
Scrambler Therapy is a neuromodulatory approach using electro-cutaneous nerve stimulation forrelieving acute and chronic pain on the basis of information theory [6]. In this respect, Marineo [4] explained that the pain system consists of information content that is delivered by specific receptors includingmechanoceptors and multimodal receptors. Under healthy conditions, painful information returns to a silent state by the process of homeostatic equilibrium; however, in chronic neuropathic conditions, pain gradually tends to be changed in a refractory manner upon therapeutic modalities by the sensitization modifying the original information. Scrambler therapy synthesizes 16 different types of artificial nerve action potentials similar to normal nerve impulses, assembles them into sequences and transmits them to the patient's nociceptors. Finally, it modulates the pain information through patient-specific cutaneous electro-stimulation [3,6]. While transcutaneous electrical nerve stimulation (TENS) and implanted devices inhibit pain transmission through A-beta fiber excitation, Scrambler Therapy substitutes pain information with synthetic non-pain information with more complex processing [5]. MC5-A Calmare® consists of a multiprocessor with five channels capable of treating five painful areas in the same patient simultaneously. Additionally, each channel consists of 2 surface electrodes placed on the skin around the painful areas, but not in the painful areas [6]. Correct position of the electrodes depends on the response of the patient and an immediate sign is the disappearance of pain in the targeted areas. It is very important for a patient to feel a rippling sensation rather than pain during therapy [4,6].
In our cases, all had been treated with conventional modalities for more than a year but still complained of severe pain. For the purpose of providing pain relief, they received Scrambler Therapy for 50 minutes daily for 10 consecutive days based on some clinical trials [3,4,6-8]. All 3 patients did not complain of any previously experienced severe aching pain and tactile allodyniawhen they received the Scrambler Therapy. Marineo [3] suggested that this reason may be due to the feeling of new sensations around the dermatome related to the spread of non-pain information along the lines of nerve transmission, the so called "pain scramble". In the early sessions of the treatment, the effects ofthe Scrambler Therapy lasted only for 3 to 6 hours in all. However, the effects had lasted all days long after 2 sessions in one patient, after 3 sessions in another patient and after 5 sessions in the last patient, respectively. At the same time, constant aching pain and tactile allodyniadecreased to a tolerable range. When the-tenth session was finished, constant aching pain decreased by 50% compared with the previous state and tactile allodynia had gone away (Fig. 3). Two of the three patients were given one more treatment for a transient aggravation. Since then, all patients have been well managed with oral medications and do not complain of any undesirable side effects. In addition to pain relief, the fact that tactile allodynia disappeared is also worthy of notice. We think that the disappearance of allodynia may be associated with central reorganization, but do not know exactly what this mechanism is. Thus, further studies will be required to investigate this phenomenon. Several preliminary studies on the efficacy of Scrambler Therapy for cancer and refractory neuropathic pain have been introduced recently and reported good outcomes like in our cases [3-8].
In conclusion, through this report, we show that Scrambler Therapy can be a good option for the treatment of patients with PHN, who respond poorly to previous conventional treatments or have a fear of receiving other invasive treatments due to one's own comorbidity. However, we suggest that more extensive investigations with a large number of patients are necessary to provide well established guidelines for Scrambler Therapy of PHN.
References
2. Galluzzi KE. Management strategies for herpes zoster and postherpetic neuralgia. J Am Osteopath Assoc. 2007; 107:S8–S13. PMID: 17488885.
3. Marineo G, Iorno V, Gandini C, Moschini V, Smith TJ. Scrambler therapy may relieve chronic neuropathic pain more effectively than guideline-based drug management: results of a pilot, randomized, controlled trial. J Pain Symptom Manage. 2012; 43:87–95. PMID: 21763099.

4. Marineo G. Untreatable pain resulting from abdominal cancer: new hope from biophysics? JOP. 2003; 4:1–10. PMID: 12555009.
5. Sabato AF, Marineo G, Gatti A. Scrambler therapy. Minerva Anestesiol. 2005; 71:479–482. PMID: 16012423.
6. Ricci M, Pirotti S, Scarpi E, Burgio M, Maltoni M, Sansoni E, et al. Managing chronic pain: results from an open-label study using MC5-A Calmare® device. Support Care Cancer. 2012; 20:405–412. PMID: 21394458.

7. Marineo G, Spaziani S, Sabato AF, Marotta F. Artificial neurons in oncological pain: the potential of Scrambler Therapy to modify a biological information. Int Congr Ser. 2003; 1255:381–388.

8. Smith TJ, Coyne PJ, Parker GL, Dodson P, Ramakrishnan V. Pilot trial of a patient-specific cutaneous electrostimulation device (MC5-A Calmare®) for chemotherapy-induced peripheral neuropathy. J Pain Symptom Manage. 2010; 40:883–891. PMID: 20813492.

Fig. 1
MC5-A Model. Calmare® consists of a multiprocessor with five channels capable of treating five painful areas in the same patient simultaneously.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download