Abstract
Background
Conventional spinal saddle block is performed with the patient in a sitting position, keeping the patient sitting for between 3 to 10 min after injection of a drug. This amount of time, however, is long enough to cause prolonged postoperative urinary retention. The trend in this block is to lower the dose of local anesthetics, providing a selective segmental block; however, an optimal dose and method are needed for adequate anesthesia in variable situations. Therefore, in this study, we evaluated the question of whether only 1 min of sitting after drug injection would be sufficient and safe for minor anorectal surgery.
Methods
Two hundred and sixteen patients undergoing minor anorectal surgery under spinal anesthesia remained sitting for 1 min after completion of subarachnoid administration of 1 ml of a 0.5% hyperbaric bupivacaine solution (5 mg). They were then placed in the jack-knife position. After surgery, analgesia levels were assessed using loss of cold sensation in the supine position. The next day, urination and 11-point numeric rating scale (NRS) for postoperative pain were assessed.
Results
None of the patients required additional analgesics during surgical manipulation. Postoperative sensory levels were T10 [T8-T12] in patients, and no significant differences were observed between sex (P = 0.857), height (P = 0.065), obesity (P = 0.873), or age (P = 0.138). Urinary retention developed in only 7 patients (3.2%). In this group, NRS was 5.0 ± 2.4 (P = 0.014).
Spinal anesthesia for peri-anal surgery could be chosen variously with regard to the targeted range of sensory blockade, depending on the type of surgery, posture during surgery, or the property of the local anesthetic. In cases where a patient undergoes surgery in a jack-knife position, the saddle block can usually be performed using hyperbaric local anesthetics. Induction of anesthesia using this conventional saddle block is relatively easy; however, it also has several disadvantages. To prevent the occurrence of hypotension due to re-distribution of local anesthetics following posture change for the surgical procedure, patients are recommended to take a sitting position for several minutes after injection of anesthetic agents. This leads to a time delay in initiation of the surgical procedure and to the need for additional support during posture change due to extended motor blockade in the lower extremities [1]. Also, it results in a prolonged hospital stay owing to the increased frequency of postoperative urinary retention [2,3]. In addition, there is a possibility that bupivacaine might travel to dependent areas within the cerebrospinal fluid (CSF) in spite of maintenance of the same posture for a substantial period of time; this might result in an undesirably high level of spinal anesthesia accompanied by side effects [4,5].
Duration of spinal anesthesia is affected by the concentration of drugs around the nerve roots [6]. Hence, because drugs spread within CSF tend to be in relatively low concentrations, the duration of effects of local anesthetics is shortened if the posture was changed immediately after conducting the spinal anesthesia from the lateral decubitus to the supine. On the contrary, if posture was maintained in the sitting position during a substantial period of time after conducting anesthesia, the duration of anesthesia is prolonged. Besides, if diffusion of local anesthetics should occur to a smaller extent, this would reduce the area of drug absorption. This is one of the factors that can prolong the time of anesthetic maintenance [7].
Given the above background, we attempted to evaluate the influence of the method in which position is changed following maintenance of the sitting position only for 1-minute, a shorter-than-usual method, on the level of spinal anesthesia and on postoperative urinary retention after administration of hyperbaric bupivacaine at a dose of 5 mg, which is recommended for saddle block in patients undergoing peri-anal surgery in a jack-knife posture.
The study was conducted in patients whose physical status corresponded to Grade I or II, according to the American Society of Anesthesiologists (ASA) classification. These patients were given an explanation of the objectives of the study, and submitted written informed consent.
Premedication was not administered to any of the subject patients prior to anesthesia. Patients were placed in a sitting position under standard monitoring. Using a 25-G Quincke spinal needle (Hakko®, Chikuma-shi, Nagano-ken, Japan), subarachnoid puncture was performed between the third and the fourth lumbar vertebrae via a median approach and was confirmed by spontaneous clear CSF leakage through the needle. Following aspiration, CSF of 0.2 ml, a 0.5% high-density bupivacaine (Marcaine 0.5% Spinal Heavy®, AstraZeneca AB, Sodertalje, Sweden) 5 mg was injected into the intrathecal space at a rate of 1 ml/20 sec. Patients were then instructed to maintain a sitting position for one minute before changing to the prone position by themselves. They were placed in a jack-knife position, where the head region was tilted downward at an angle of 15° immediately after the prone position.
During the surgical procedure, patients' vital signs were monitored by ECG, automatic blood pressure monitoring at 3-minute intervals, and pulse oximetry. Patients who developed nausea sensation or vomiting not related to the surgical maneuver, but concurrent with a low systolic blood pressure (lower than 90 mmHg or decreased by more than 20% compared to the previous measurement at wards), received intravenous administration of 5-10 mg ephedrine. Also, patients were requested to express subjectively any discomfort associated with the operation.
For the stapled hemorrhoidectomy, tiropramide 50 mg was injected intravenously in order to reduce intestinal peristalsis. In cases where postoperative bleeding was suspected to occur at the site, an absorbable material (SPONGOSTAN® Anal, Johnson & Johnson, Skipton, UK) was inserted for hemostasis.
The level of anesthesia was intermittently measured throughout the operation. However, for comparison, the level at completion of anesthesia was consistently selected. After patients' posture was converted to the supine position, a loss of cold sensation was checked using an alcohol swab on the bilateral anterior axillary lines and scores for the level of anesthesia were given to each segment from the first thoracic dermatomes.
Continuous infusion of fentanyl 20 µg/kg and ketorolac 1.5 mg/kg (basal rate; 2 ml/h, bolus; 0.5 ml, and lockout time; 15 minutes) was applied to all patients for postoperative pain control through a patient controlled analgesic device (Accufusor Plus®, Woo-Young, Jincheon, Chungcheongbuk-do, Korea). On the following day, each patient was visited for assessment of urinary retention and intensity of postoperative pain. Urinary retention was assumed in cases where a patient could not void spontaneously within 6 hours after surgery, requiring an indwelling catheter or intermittent urethral catheterization. An 11-point numeric rating scale (NRS) was used for assessment of the intensity of postoperative pain.
Statistical analyses were performed using SPSS (SPSS 12.0KO for windows®, SPSS Inc, Chicago, USA). In all subject patients, a stratified analysis was performed based on gender, height, index of obesity, and age. Data were expressed as mean ± SD, mean value [interquantile range], or frequencies. For parametric data, an analysis of variance (ANOVA) was applied to homoscedastic data; otherwise, the Welch two sample t-test was applied. Chi-square analysis was performed for qualitative data. Post-hoc analysis was performed using Bonferroni methods or Fisher's exact test. Statistical significance was set at P < 0.05.
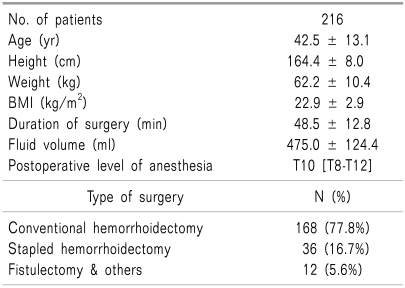
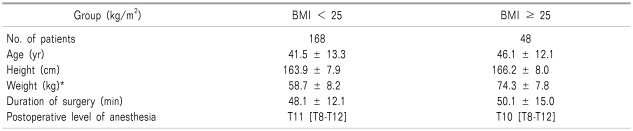
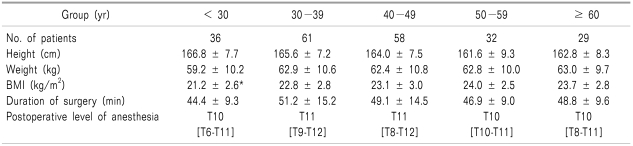
A total of 216 patients were enrolled in the present study. The characteristics of patients and the type of surgery are presented in Table 1. In all patients, a loss of cold sensation was revealed at the surgical site one minute after an intrathecal injection of 0.5% bupivacaine. Patients were able to assume the prone position by themselves. The mean value of the level of anesthesia after completion of anesthesia was found to be T10 [T8-T12], which was based on a loss of cold sensation checked in the supine position (Table 1).
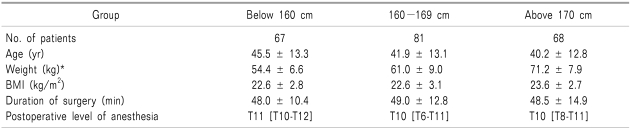
To evaluate the influence of posture change to prone after maintenance of the sitting position for only 1 minute on the level of anesthesia, patients were subdivided based on gender, height, index of obesity, and age for stratified analyses.
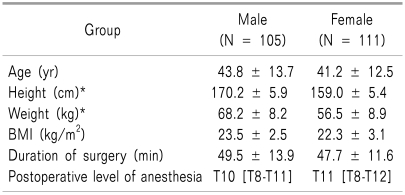
Although there were differences in height and weight, no difference in body mass index (BMI) was observed between genders. There was also no significant difference in the level of anesthesia, which was measured at completion of surgery (P = 0.857) (Table 2).
On the level of the fourth thoracic dermatome or higher, where there might be abnormal findings for vital signs due to a sympathetic nerve block, a loss of cold sensation occurred in a total of 10 patients (4.6%). Of these, one patient was given ephedrine due to a concurrent presence of hypotension, nausea sensation, and vomiting.
A feeling of discomfort associated with the surgical maneuver was found in a total of 7 patients. That is, there were 4 cases of lower abdominal discomfort during stapled hemorrhoidectomy and three cases of lower abdominal discomfort associated with the surgical posture due to a prolonged operation time during conventional hemorrhoidectomy. Compared with patients who did not complain of discomfort, only operation time was found to be prolonged (Table 6).
A total of 7 patients were affected by postoperative urinary retention (male = 3, female = 4, 3.2%). In these patients, NRS was significantly higher than in self voided patients (Table 6). Besides, it was also shown that the incidence of urinary retention increased following insertion of Spongostan for postoperative hemostasis (P = 0.003; odds ratio = 12.43).
The present study was conducted in order to examine the question of whether anesthesia could be successfully performed by maintenance of the sitting position during a shorter period, compared with conventional types of saddle block, which are routinely attempted for peri-anal surgery. This study was of significance not only because it showed a relatively lower degree of incidence of urinary retention compared with previous reports, but also because safe administration of anesthesia could be performed to a substantial extent only by maintenance of a 1-minute sitting position.
The scope of nerve block during spinal anesthesia is determined by the distribution of local anesthetics, which were administered intrathecally. Since hyperbaric local anesthetics, which are commonly used for spinal anesthesia, have a higher density compared with CSF, they flow to the dependent area. Therefore, their distribution is greatly dependent on the posture of the patient. In addition, it can also be affected by height, weight, gender, posture, anatomy of the thecal cavity, location of drug administration, rate of drug administration, direction of drug administration, and the characteristics of local anesthetics, including density, concentration, and dose [8]. Particularly in cases in which a sitting position is maintained, the volume of CSF has been reported to have a great impact on the period of anesthesia [9].
Conversion to general anesthesia is difficult due to the characteristics of the jack-knife position for peri-anal surgery. Accordingly, for definite anesthesia at the surgical site and to prevent a high level of spinal anesthesia extended to the upper thoracic level, a sitting position is maintained during a long-term period following injection of local anesthetics. However, the time for initiation of a surgical procedure could be delayed; incidences of excessive motor blockade of lower extremities or postoperative urinary retention could be increased.
Since the latest trends in peri-anal surgery for treatment of benign legions are based on an outpatient setting or on very-day discharge, a small dose of local anesthetics is required for administration of selective segmental anesthesia. Yet, complications such as bleeding and increased pain can be incurred due to the extended scope of surgery. This may lead to a prolonged hospital stay, and patients may not be satisfied with the selective segmental anesthesia [10,11].
There have been several studies of the relationship between duration of the sitting position before posture change and distribution of intrathecally-administered local anesthetics. If patients should be placed in a supine position after continuous maintenance of a sitting position for ten minutes following saddle block, the areas of the sensory blockade are restricted to the sacral or lumbar spinal levels. In these cases, the volume of anesthetic agents was involved [8]. Compared to groups undergoing a position change to the supine immediately after intrathecal injection of a high-dose of bupivacaine, there were no significant differences in the maximal scope of anesthesia, the time to reach the maximal scope of anesthesia, and the time elapsed until recovery from anesthesia was achieved in groups who maintained a sitting position for 2 minutes [9]. Even in cases in which a sitting position was maintained for 3 minutes, there were no significant differences in the areas of maximal sensation blockade and those of a loss of cold sensation. In particular, it has also been reported that the motor blockade was strengthened after a sitting position was maintained for 3 minutes following saddle block [12]. Besides, according to a study conducted in elderly subjects, aged 60 years or older, although a sitting position was maintained for 20 minutes, the maximal scope of anesthesia appeared later, but showed no significant difference [13].
According to studies of fixation of intrathecally administered bupivacaine, a 10-minute period for maintenance of the lateral decubitus position would be sufficient for the unilateral motor blockade. However, for unilateral blockage of the sensory nerve and autonomic nervous systems, more than 30 minutes are required for a lateral decubitus position and a time period shorter than 15 minutes would be insignificant. Furthermore, a minimum length of 60 minutes would be required for intrathecal fixation of bupivacaine [14]. Since local anesthetics are continuously transferred within the CSF during that period, the maximal scope of sensory block would appear after approximately 20 minutes [15]. Even in cases in which a sitting position was maintained for 2 minutes and then converted to a supine position, the maximal scope of sensory block appeared 20-30 minutes later [16]. In the current study, despite a lack of statistical significance, blood pressure was slightly lowered within 10-15 minutes following conversion to a jack-knife position. Twenty minutes later, however, it was consistently maintained or recovered again. These findings are assumed to support the above reports.
Postoperative urinary retention related to peri-anal surgery under spinal anesthesia has been reported with various risk factors as well as wide ranges between 7.9% and 20.3% [17-20]. In association with spinal anesthesia, the detrusor muscles of the bladder would achieve a voiding reflex when the scope of anesthesia was diminished to lower than the third sacral level [21]. According to a study of recovery from anesthesia using a high-dose bupivacaine, the sacral nerve block was strengthened, which would lead to delayed recovery of the functions of the urinary bladder in patients who are placed in a sitting position [3]. However, in cases in which 0.5% bupivacaine was administered at a volume of 1 ml and 2 ml, there was a significant difference in the time where patients could perform the ambulatory movement; however, there was no significant difference in the time point for voiding between the two groups [22].
In this study, to minimize the distribution of bupivacaine depending on the conversion of patient posture, local anesthetics were administered at a rate of 1 ml/20 sec. A high speed of administration of local anesthetics could affect its distribution due to the generation of vortex in the thecal cavity [23]; it has also been reported that intrathecal distribution of local anesthetic agents would be decreased at a lower rate of administration [24,25]. Besides, an infusion rate of 2 ml/min would be both appropriate and safe, considering the incidence and severity of hypotension, and the decreased dose of anti-hypertensive agents during cesarean section under spinal anesthesia [26].
Despite the definite presence of differences in height and weight between male and female patients in this study population, there was no significant difference in the scope of anesthesia. This might be due to the difference in the capacity for locomotion among individuals. Local anesthetics accumulated in the sacral region with the actions of gravity due to a lower rate of administration, which led to prompt onset of anesthesia. In addition, because of insufficient time (1 minute) for motor blockade, patients could assume a prone position for themselves. However, compared with adult males, more time is required for conversion of posture by women or elderly people; this might therefore affect the intrathecal distribution of local anesthetics. Based on the characteristics of a jack-knife position, it was speculated that increased abdominal pressure would affect the intrathecal distribution of local anesthetics; however, there were no effects on BMI.
A feeling of discomfort during surgery might be associated with increased intestinal peristalsis due to blockade of the sympathetic nervous system related to distribution of local anesthetics. A lower incidence of urinary retention in this study might be due to restricted replacement of fluid during surgery. However, it can also be inferred that local anesthetics were re-distributed without being fixed to the sacral region when a sitting position was maintained for only one minute. Even though postoperative urinary retention might occur due to reflective contracture of the internal urethral sphincter, which was induced from anal pain following surgery, it is presumed that the pain was aggravated due to the presence of urinary retention, not vice versa. Limitations of the current study are as follows: First, in conventional types of saddle block, where a sitting position is typically retained for more than three minutes, no control groups were served. Therefore, no definite comparisons were made for discomfort, incidence, and cause of urinary retention during peri-anal surgery. Second, all patients converted their posture individually. However, due to differences in methods for changing posture among patients, the discrepancy in motor function and the time elapsed until posture was converted could not be clarified. These deserve further controlled studies.
In conclusion, even though the posture of patients was changed to the prone position after maintenance of the sitting position for only 1 minute, spinal anesthesia for peri-anal surgery could be administered both safely and substantially in cases where local anesthetics were administered at a lower rate of 1 ml/20 sec. Use of this alternative method can shorten the onset of anesthesia and restore patients' motor function in order to reduce the risk for occurrence of trauma during posture change. Although a controlled study to compare to the conventional saddle block with regard to incidence of postoperative urinary retention will be needed in the future, a certain degree of the scope of anesthesia could be expected regardless of sex, height, obesity index and age.
References
1. Wassef MR, Michaels EI, Rangel JM, Tsyrlin AT. Spinal perianal block: a prospective, randomized, double-blind comparison with spinal saddle block. Anesth Analg. 2007; 104:1594–1596. PMID: 17513664.

2. Gudaityte J, Marchertiene I, Pavalkis D, Saladzinskas Z, Tamelis A, Tokeris I. Minimal effective dose of spinal hyperbaric bupivacaine for adult anorectal surgery: a double-blind, randomized study. Medicina (Kaunas). 2005; 41:675–684. PMID: 16160416.
3. Rätsch G, Niebergall H, Hauenstein L, Reber A. Spinal anaesthesia in day-case surgery. Optimisation of procedures. Anaesthesist. 2007; 56:322–327. PMID: 17273833.
4. Bigat Z, Boztug N, Karsli B, Cete N, Ertok E. Comparison of hyperbaric ropivacaine and hyperbaric bupivacaine in unilateral spinal anaesthesia. Clin Drug Investig. 2006; 26:35–41.

5. Vicent O, Litz RJ, Hübler M, Koch T. Secondary cranial extension after spinal anesthesia with isobaric 0.5% bupivacaine following postural change. Anaesthesist. 2003; 52:1035–1038. PMID: 14992091.
6. Neigh JL, Kane PB, Smith TC. Effects of speed and direction of injection on the level and duration of spinal anesthesia. Anesth Analg. 1970; 49:912–918. PMID: 5534690.

7. Kitahara T, Kuri S, Yoshida J. The spread of drugs used for spinal anesthesia. Anesthesiology. 1956; 17:205–208. PMID: 13283361.
8. Wildsmith JAW, Rocco AG. Current concepts in spinal anesthesia. Reg Anesth. 1985; 10:119–124.
9. Higuchi H, Adachi Y, Kazama T. The influence of lumbosacral cerebrospinal fluid volume on extent and duration of hyperbaric bupivacaine spinal anesthesia: a comparison between seated and lateral decubitus injection positions. Anesth Analg. 2005; 101:555–560. PMID: 16037175.

10. Charuluxananan S, Sriprajittichai P, Sirichotvithyakorn P, Rodanant O, Kyokong O. Factors related to patient satisfaction regarding spinal anesthesia. J Med Assoc Thai. 2003; 86(Suppl 2):S338–S343. PMID: 12930008.
11. Gudaityte J, Marchertiene I, Pavalkis D. Anesthesia for ambulatory anorectal surgery. Medicina (Kaunas). 2004; 40:101–111. PMID: 15007268.
12. Stienstra R, van Poorten JF. Plain or hyperbaric bupivacaine for spinal anesthesia. Anesth Analg. 1987; 66:171–176. PMID: 3813061.

13. Veering BT, Immink-Speet TT, Burm AG, Stienstra R, van Kleef JW. Spinal anaesthesia with 0.5% hyperbaric bupivacaine in elderly patients: effects of duration spent in the sitting position. Br J Anaesth. 2001; 87:738–742. PMID: 11878525.

14. Povey HM, Jacobsen J, Westergaard-Nielsen J. Subarachnoid analgesia with hyperbaric 0.5% bupivacaine: effect of a 60-min period of sitting. Acta Anaesthesiol Scand. 1989; 33:295–297. PMID: 2655366.

15. Arai YC, Ueda W, Takimoto E, Manabe M. The influence of hyperbaric bupivacaine temperature on the spread of spinal anesthesia. Anesth Analg. 2006; 102:272–275. PMID: 16368842.

16. Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Helenius HY, Kirvelä OA. The use of bupivacaine and fentanyl for spinal anesthesia for urologic surgery. Anesth Analg. 2000; 91:1452–1456. PMID: 11093999.

17. Chik B, Law WL, Choi HK. Urinary retention after haemorrhoidectomy: impact of stapled haemorrhoidectomy. Asian J Surg. 2006; 29:233–237. PMID: 17098654.

18. Lingaraj K, Ruben M, Chan YH, Das SD. Identification of risk factors for urinary retention following total knee arthroplasty: a Singapore hospital experience. Singapore Med J. 2007; 48:213–216. PMID: 17342289.
19. O'Riordan JA, Hopkins PM, Ravenscroft A, Stevens JD. Patient-controlled analgesia and urinary retention following lower limb joint replacement: prospective audit and logistic regression analysis. Eur J Anaesthesiol. 2000; 17:431–435. PMID: 10964144.
20. Toyonaga T, Matsushima M, Sogawa N, Jiang SF, Matsumura N, Shimojima Y, et al. Postoperative urinary retention after surgery for benign anorectal disease: potential risk factors and strategy for prevention. Int J Colorectal Dis. 2006; 21:676–682. PMID: 16552523.

21. Kamphuis ET, Ionescu TI, Kuipers PW, de Gier J, van Venrooij GE, Boon TA. Recovery of storage and emptying functions of the urinary bladder after spinal anesthesia with lidocaine and with bupivacaine in men. Anesthesiology. 1998; 88:310–316. PMID: 9477049.

22. Tarkkila P, Huhtala J, Tuominen M. Home-readiness after spinal anaesthesia with small doses of hyperbaric 0.5% bupivacaine. Anaesthesia. 1997; 52:1157–1160. PMID: 9485968.

23. Bourke DL, Sprung J, Harrison C, Thomas P. The dribble speed for spinal anesthesia. Reg Anesth. 1993; 18:326–327. PMID: 8268125.
24. Atchison SR, Wedel DJ, Wilson PR. Effect of injection rate on level and duration of hypobaric spinal anesthesia. Anesth Analg. 1989; 69:496–500. PMID: 2782650.

25. Horlocker TT, Wedel DJ, Wilson PR. Effect of injection rate on sensory level and duration of hypobaric bupivacaine spinal anesthesia for total hip arthroplasty. Anesth Analg. 1994; 79:773–777. PMID: 7943791.

26. Simon L, Boulay G, Ziane AF, Noblesse E, Mathiot JL, Toubas MF, et al. Effect of injection rate on hypotension associated with spinal anesthesia for cesarean section. Int J Obstet Anesth. 2000; 9:10–14. PMID: 15321104.

Table 6
Patient Characteristics and Performed Surgical Procedures in the Intraoperative Discomfort Group and in the Postoperative Urinary Retention Developed Group
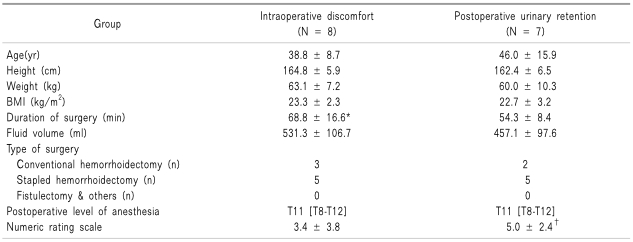
Data for age, height, weight, BMI, duration of surgery, administered fluid volume, and 11-point verbal rating scale are expressed as mean ± SD, and as median [interquartile range] for postoperative level of anesthesia. BMI: body mass index, T: thoracic dermatome. *P < 0.01 (compared with non-discomfort patients), †P = 0.014 (compared with self voiding patients).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download