Abstract
Tuberculous spondylitis is a very rare disease, but it can result in bone destruction, kyphotic deformity, spinal instability, and neurologic complications unless early diagnosis and proper management are done. Because the most common symptom of tuberculous spondylitis is back pain, it can often be misdiagnosed. Atypical tuberculous spondylitis can be presented as a metastatic cancer or a primary vertebral tumor. We must make a differential diagnosis through adequate biopsy. A 30-year-old man visited our clinic due to back and chest pain after a recent traffic accident. About 1 year ago, he had successfully recovered from tuberculous pleurisy after taking anti-tuberculosis medication. We performed epidural and intercostal blocks but the pain was not relieved. For the further evaluation, several imaging and laboratory tests were done. Finally, we confirmed tuberculous spondylitis diagnosis with the biopsy results.
Since tuberculous spondylitis is the most common and dangerous type of tuberculosis occurring in the musculoskeletal system, and it can lead to severe neurological complications and spinal deformity, an early diagnosis and medication of anti-tuberculosis agents are important. Tuberculous spondylitis usually starts in the vertebral body and infects adjacent tissue along the anterior longitudinal ligament. Hence, infection at two adjacent spines, a broken intervertebral disc between the two spines, and pus nearby the spines or at the iliopsoas muscle are commonly found. However, an atypical form of tuberculous spondylitis can cause much confusions regarding the diagnosis. We report our unexpected experience of early diagnosis of atypical tuberculous spondylitis during the pain treatment of a patient with a past history of complete recovery from tuberculous pleurisy by proper treatment.
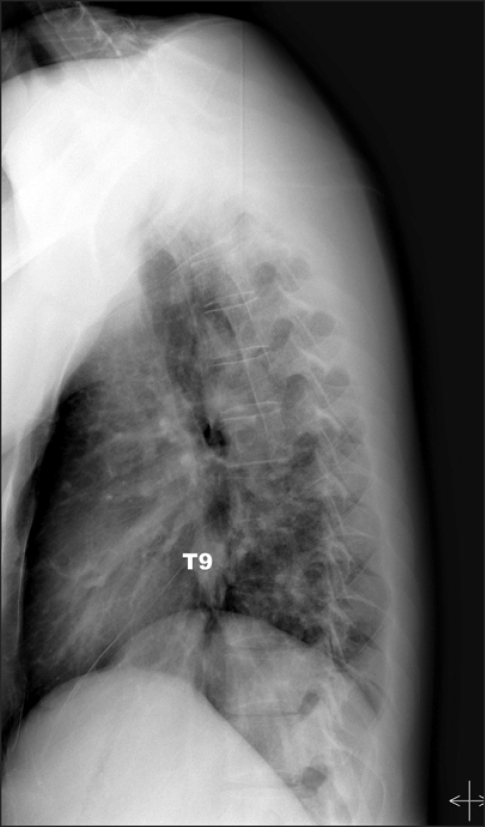
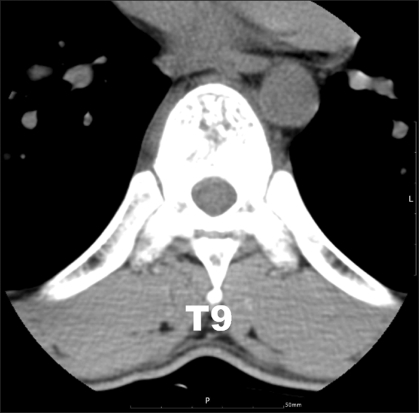
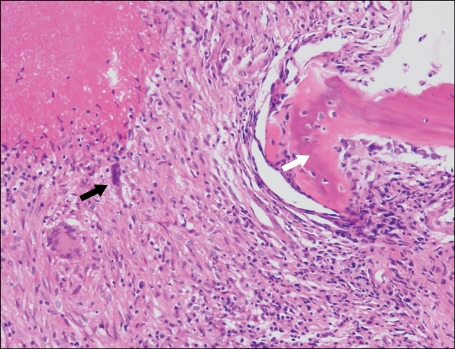
A 30-year-old male patient was brought to the emergency room and neurosurgery department with the chief complaints of pain at the right side chest and right side back, which had originated from a rear-end collision car accident that had happened one month before. The patient had been in the passenger's seat during the collision. Though he was given an NSAID, the condition was not improved and he was moved to the pain clinic. His height was 176 cm and his weight was 72 kg. In his medical history, he was announced to be fully recovered from tuberculous pleurisy one year ago, following 14 months of anti-tuberculousis medication. Neither fever nor loss of weight was found recently. The pain was like being stiff and broken, painful even when sitting motionlessly, but more severe during heavy breathing. The visual analogue scale (VAS) was an 8/10 score. According to diagnostic findings, the pain pattern was like putting a belt around the skin segment corresponding to the 9th thoracic vertebra. No special finding was discovered except the tender point located at the right side rib, which fell on the 10th rib. According to the plain X-ary of the chest region at that time, the finding was an old fibrocalcific tuberculosis scar involving both upper lobe apexes. The simple X-ray findings were normal at the thoracic vertebra and ribs (Fig. 1). The laboratory test results were WBC 6,980/mm3, ESR 18 mm/hr, CRP 14.97 mg/dl, total protein 7.92 g/dl, and albumin 4.51 g/dl. Since continued medication and injection at the tender point had no effect, an epidural block and intercostal block were performed suspecting sprain from experience, but no improvement was found. Magnetic resonance (MR) imaging at the thoracic vertebra region for a differential diagnosis showed an abnormal signal at the ninth thoracic vertebral body (Fig. 2). From the computed tomography (CT) result, trabeculae thickening, loss of tubular shape, and reduced bone density were found heterogeneously, as well as a seemingly abnormal fracture with the fracture line at the upper plate (Fig. 3). Suspecting a metastatic spine tumor, such as hemangioma or metastasis of a malignant tumor, the patient was transferred to the Oncology department and additional tests were performed. According to the bone scanning, extensive absorption increase at the 9th thoracic vertebra, and absorption increase at the 6th and 10th right ribs were found. A positron emission tomography (PET) showed FDG (fluorine-18 fluorodeoxyglucose) absorption increase at the 9th thoracic vertebral body and the 10th right rib. To check for the existence of other malignant tumors, lung computed tomography and blood tests, including a tumor maker and endoscope in the stomach and large intestine, were performed with no specific findings. Moreover, the AIDS test results were negative, the AFB (acid fast bacillus) smear test was negative, the MTB PCR was positive, and the AFB culture test was negative. By reviewing the biopsy, chronic granulomatous inflammation with caseous necrosis and multinucleated giant cells were found, so that the tuberculous spondylitis diagnosis was confirmed (Fig. 4). At present, the patient is visiting the Department of Internal Medicine and being given anti-tuberculosis agents and NSAID. The pain is maintained at the level of VAS 3-4/10 score.
Though tuberculous spondylitis is not common, as it is only 2% of the total tuberculosis infection cases, it is the most frequent form found in the musculoskeletal tuberculosis cases. As overseas travel becomes more frequent, the number of immigrants and foreign residents is increasing, and the number of immune compromised patients, such as those with AIDS, is increasing, the incidence rate of tuberculous spondylitis is also recently increasing, even in developed countries [1]. Major symptoms are back pain, paralysis, fever, and paresthesia. The most frequently invaded parts are the lower thoracic vertebra and thoracolumbar spine. The laboratory test findings, such as an increase in ESR and CRP and a positive result of the tuberculin skin test, can provide partial information, but they do not provide decisive help [2]. A simple radiographic image has a disadvantage in that it can provide information only after considerable destruction of spinal body has progressed. Routine pain treatment, such as an epidural block, without confirmed diagnosis of tuberculous spondylitis but only in reference to simple radiographic images and laboratory tests, should be carefully decided since it can cause spread of the infection [3].
The MR Imaging, which shows hypointensity on the T1-weighted image and hyperintensity on the T2-weighted image, can provide useful information to decide whether the operation is necessary, as well as to determine an initial diagnosis, and to help with the differential diagnosis of other diseases such as cancer and pyogenic spondylitis. However, since it can be misunderstood as a spine tumor or cancer metastasis when only a single vertebral body was invaded, the final decision should be made by means of biopsy [4].
Atypical tuberculous spondylitis can be divided into three categories: Type 1 is the invasion only to neural arch; Type 2 is the invasion and destruction of a single vertebral body; and Type 3 is mass in the spinal cavity, not invading the bones [5].
The treatment of tuberculous spondylitis includes, first of all, proper anti-tuberculosis agent medication for 12 months or more. Surgical decompression, excision of dead tissue, and spinal fusion should be performed for patients with spinal instability [6]. In this case report, corresponding to Type 2, the tuberculous spondylitis did not progress to the severe vertebral body and spine thickening that may require surgery, since the disease was found early and a proper anti-tuberculosis agent was given.
Recurrent tuberculosis can be divided into two groups: One is the relapse of tuberculosis due to the failure of anti-tuberculosis treatment in sterilizing the host tissue, resulting in an infection by the same strain that may have caused the first infection, and the other is recurrence through reinfection by a new type of strain.
Where there is a higher risk of tuberculosis, the probability of reinfection after successful treatment is four times higher than that of the initial infection [7], and the reinfection is known to occur usually within 6-12 months [8]. The rate of simultaneous occurrence of tuberculous spondylitis and lung tuberculosis have been reported to be about 50% [9], but it is very unusual that atypical tuberculous spondylitis occurs after successful treatment as in this case report. When tuberculosis has recurred, whether by the same strain of the initial infection or by a different strain, it can be identified by DNA fingerprinting. However, no differentiation of relapse and reinfection has yet been performed in Korea [10]. The common parts of the body for lung tuberculosis, in addition to the lungs, are lymph nodes, bones and joints, intestine organs, the liver, genital organs, peritoneum and pericardium where cell-mediated immunology is involved and of which reported expectation factors are an invasion to both lungs without formation of cavities, and hypoalbuminemia [11].
The patient in this case report had already announced that his tuberculosis had been fully treated and he was young enough not to have specific symptoms that may cause suspicion of a lowered immune response or infection. In addition, since the simple X-ray of the thoracic spine showed no specific finding and the pain body part after the injury was the same as the parts of the underlying disease, tuberculous spondylitis could not be suspected from the beginning. We assume that the vertebral body that had been weakened by tuberculous spondylitis caused the pain through the injury, although the correlation with the injury is not very clear. In the cases where the patients who have tuberculosis history or signs complain of a back pain in areas where the incidence rate is high, such as in Korea, a thorough physical examination should be performed. Moreover, even if the laboratory test or plain X-ary results are normal, differential diagnosis of tuberculous spondylitis, which may cause serious complications, needs to be performed by means of CT and MR imaging, not excluding the possibility of tuberculous spondylitis occurrence.
References
1. Snider GL. Tuberculosis then and now: a personal perspective on the last 50 years. Ann Intern Med. 1997; 126:237–243. PMID: 9027277.

2. Okuyama Y, Nakaoka Y, Kimoto K, Ozasa K. Tuberculous spondylitis (Pott's disease) with bilateral pleural effusion. Intern Med. 1996; 35:883–885. PMID: 8968802.

3. Chang DJ, Yoon DM, Kang YS, Yoon KB. Chronic back pain proven to be spinal tuberculosis: a report of 2 cases. Korean J Pain. 2008; 21:74–79.

4. Ahmadi J, Bajaj A, Destian S, Segall HD, Zee CS. Spinal tuberculosis: atypical observations at MR imaging. Radiology. 1993; 189:489–493. PMID: 8210378.

5. Naim-Ur-Rahman , Al-Arabi KM, Khan FA. Atypical forms of spinal tuberculosis. Acta Neurochir (Wien). 1987; 88:26–33. PMID: 3425410.

6. Nussbaum ES, Rockswold GL, Bergman TA, Erickson DL, Seljeskog EL. Spinal tuberculosis: a diagnostic and management challenge. J Neurosurg. 1995; 83:243–247. PMID: 7616269.

7. Verver S, Warren RM, Beyers N, Richardson M, van der, Borgdorff MW, et al. Rate of reinfection tuberculosis after successful treatment is higher than rate of new tuberculosis. Am J Respir Crit Care Med. 2005; 171:1430–1435. PMID: 15831840.

8. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American thoracic society/centers for disease control and prevention/infectious diseases society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003; 167:603–662. PMID: 12588714.

9. Schlesinger N, Lardizabal A, Rao J, Rao J, McDonald R. Tuberculosis of spine: experience in an inner city hospital. J Clin Rheumatol. 2005; 11:17–20. PMID: 16357692.
10. Yoo SS, Kwon JS, Kang YR, Lee JW, Cha SI, Park JY, et al. The clinical characteristics and outcomes of short-term treatment in patients with recurrent pulmonary tuberculosis. Tuberc Respir Dis. 2008; 64:341–346.

11. Kim MJ, Kim HR, Hwang SS, Kim YW, Han SK, Shim YS, et al. Prevalence and its predictors of extrapulmonary involvement in patients with pulmonary tuberculosis. J Korean Med Sci. 2009; 24:237–241. PMID: 19399264.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download