Abstract
Spinal cord stimulation (SCS) has become an established clinical option for treatment of refractory chronic pain. Current hardware and implantation techniques for SCS are already highly developed and continuously improving; however, equipment failures over the course of long-term treatment are still encountered in a relatively high proportion of the cases treated with it. Percutaneous SCS leads seem to be particularly prone to dislocation and insulation failures. We describe our experience of lead breakage in the inserted spinal cord stimulator to a complex regional pain syndrome patient who obtained satisfactory pain relief after the revision of SCS.
Spinal cord stimulation, which was first introduced in 1967, is known to be an effective and minimally invasive method of treating intractable diseases, such as the complex regional pain syndrome and the post-spine-surgery syndrome [1]. Despite its high rate of success due to technical and instrumental advances, problems related to the spinal cord stimulator have been reported [2-5]. Reported here is a case in which a follow-up examination was performed on a patient, as an outpatient, after a spinal cord stimulator was implanted in him. A month after the implant, the stimulation did not occur due to the disconnection of the spinal cord stimulator lead.
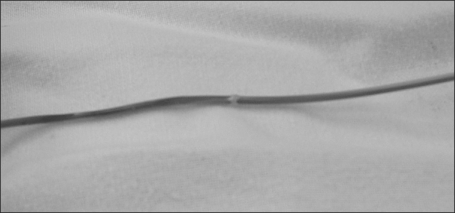
A 32-year-old man presented himself at the hospital with a complaint of numbness, causalgia, and paresthesia in the lateral region of his left ankle. Three years ago, his ankle was hit by a steel pipe, and the symptoms developed three months after open reduction and internal fixation of an ankle fracture. Based on the patient's history, traumatic partial peroneal nerve injury was suspected, and conservative treatment was started. Despite the treatment, the pain worsened and the patient received the adhesiolysis of the peroneal nerve a year before his visit to the hospital. However, the pain kept worsening, and spread below his ankle. Radiofrequency thermocoagulation and epidural patient control analgesia were performed without any improvement, so the patient presented himself again at the hospital. Based on the patient's history, he was receiving neuropsychiatric treatment for panic disorder, but he had no particular disease. When he first visited this hospital, he complained of the following subjective symptoms: pain similar to a knife cutting into his left ankle; a hot, burning feeling; an electric shock-like pain that radiated to his calf or the dorsum of his foot; a cold, tingling sensation; and decreased sensation in the regions below his knees. Based on the visual analog scale (VAS), his pain score was 9. Allodynia, hyperalgesia, body temperature asymmetry, change in sweating, and a reduced range of motion were observed in his left ankle. A three-phase bone scan revealed no particular findings, but an electromyography showed neuropathy of his superficial and deep peroneal nerve, and a digital infrared thermographic image showed that the painful site was up to 2.67℃ lower in temperature than the healthy areas of the patient's body. Pregabalin (150 mg), nortriptyline (15 mg), and Ultracet® were administered daily, and a lumbar epidural block, epidurography, and continuous ketamine infusion were performed. As the patient did not appear to respond to these treatments, we decided to try the spinal cord stimulation. A guide needle for an electrode was tunneled through the epidural space between the 1st and 2nd lumbar vertebrae, and the first electrode was placed in the middle of the 9th vertebral body. After the induced paresthesia was confirmed at the painful site, the lead and the extension cables were connected, fixed at the supraspinatus ligament while leaving a margin to avoid tension on the fixing area, and then guided out through the subcutaneous tunnel. After a test period of seven days, the pain decreased by more than 50%, and the dosage of Ultracet® was also decreased from three times to once daily, which allowed for the transplant of a permanent battery. The outpatient follow-up showed the VAS of 2-4, and a decreased dose of pregalin to 150 mg and of nortriptyline to 10 mg. One month after the operation, however, the patient reported a sudden cessation of stimulation, and accordingly, he was advised to visit the hospital. A simple lumbar X-ray was taken, and disconnection of the electrode was suspected (Fig. 1). The spinal cord stimulator was removed and inspected, which confirmed the disconnection (Fig. 2). As the patient wanted re-transplantation of the stimulator after a discussion, the lead was replaced. The patient reported a VAS score of 3 with sufficient electric stimulation and the stimulator has worked normally without particular problems as of now, four months after the operation.
The known causes of complications and failure of the spinal cord stimulator are the migration and disconnection of the lead, fibrosis, effluence of the cerebrospinal fluid, dermatitis, and meningitis due to infection of the tissues near the stimulating electrode. Most of these causes are related to the stimulator or the surgical techniques, with a reported incidence rate of 10-43% [6-10]. Based on 39 pieces of literature about device-related complications, Turner et al. [11] reported that more than one case of complications related to the stimulator device were found in over 30% of the patients. They reported the causes of the problems were related to the insulator (24%), the electrode itself (7%), and the permanent battery (2%). Besides, in a study by Taylor et al. [7], problems related to the stimulator device occurred in 43% of the patients who had a spinal cord stimulator implant for the post-spine-surgery syndrome, and their causes were the lead (27%), the extension cable (10%), and the implanted battery (6%). Cameron [10] reported a 34% prevalence rate of complications, among which problems related to the stimulator device, such as the migration or disconnection of the lead, accounted for 22%, and biological complications, such as an infection, accounted for 8%. Although few studies have investigated the time at which the stimulator device fails, reoperative surgery was required after an average of 15 months from the first implantation [12].
The damage to the electrode, as in the case in this study, can be inferred as occurring due to the following conditions: a small damage in the insulation coat of the lead because the lead that went through the needle may have been subjected to tension and pressure, which may have resulted in the disconnection of the insulator or the lead in the worst case. The damaged insulator may cause a short circuit, which may lead to malfunction of the lead. To prevent this damage, the needle and lead can be immersed in saline before the lead is inserted into the needle, so that the friction can be reduced, which can minimize the damage. In addition, repetitive folding and straightening of the lead may result in damage, or the lead may act like a hinge at the point of the spinal movement, which would reduce its surface area and can damage it through pressure. In this study, a simple radiography confirmed the disconnection of the lead near the area where it was fixed to the supraspinatus ligament in the body. The disconnection of the lead within the insulator indicates that the disconnection was due to the repetitive bending and straightening of the lead instead of damages sustained at the time of the transplant.
Based on experiments, Henderson et al. [13] suggested several measures to reduce mechanical damages to the spinal cord stimulator. They suggested that a needle should be introduced at a fairly low angle using the paramedian technique to minimize the bending angle between the supraspinatus ligament and the needle, and consequently, to minimize the tension on the lead. The entrance point of the needle should be close to the median line to make access to the epidural target point easier, reduce the lateral movement of the lead, and firmly fix the lead to the supraspinatus ligament. Since the influx of air or liquid into the epidural space will reduce contact between the lead and the epidural space and increase the possibility of lateral movement of the lead, it is discouraged. Selection of the least-moving spinal segment (the 1st to the 4th thoracic vertebra for the electrode for the cervical vertebra, and the 1st to the 4th lumbar vertebra for the electrode for the thoracolumbar) is desired to minimize the stress on the electrode caused by spinal movement. As the majority of the damages to the electrode are caused by fixation to less secure tissues, the electrode's fixation to the supraspinal ligament is desired. The extension cable should be loose enough to avoid tension on the lead at the anchor site due to body movement. Besides, percutaneous tunneling is less stressful to the lead than perforating it into the fascia, and the recently introduced silicon anchor is better than the rigid plastic anchor. It was also suggested that a neutral position of the patient during the implantation procedure could minimize the change caused by his flexion or extension, and placing the battery at the abdomen or the axilla could reduce tension more than placing it at the buttocks. Kumar et al. [2] reported that flexion and extension of the thoracolumbar vertebra caused a 9cm displacement of the lead between the upper buttocks and the thoracic vertebra, but placement of the battery at the anterior abdominal wall caused the lead to migrate by only 0.2 cm when the patient walked and by 1.7 cm when he twisted his body.
In this study, the disconnection of the lead, which is one of the mechanical problems of patients with a spinal cord stimulator implant, occurred only one month after the transplant, due to reasons other than initial failure; and consequently, the stimulation ceased. Mechanical problems, such as a damaged lead, should be considered when a patient who has a spinal cord stimulator complains of sudden cessation of the stimulation instead of a gradual decrease of the stimulation in time. Also, it is considered important that the needle be introduced at a fairly low angle using the paramedian technique, by placing the lead close to the median line, selecting the least-moving vertebra, fixing the lead to these vertebra, forming an unbent loop of the lead by incising more skin beneath the needle and sufficiently dissecting the subcutaneous tissues, tunneling percutaneously, and using a silicon anchor.
References
1. Kim WY, Moon DE, Choi JH, Park CM, Han SM, Kim SH. The effect of spinal cord stimulation in patients with complex regional pain syndrome. Korean J Pain. 2006; 19:152–158.

2. Kumar K, Wilson JR, Taylor RS, Gupta S. Complications of spinal cord stimulation, suggestions to improve outcome, and financial impact. J Neurosurg Spine. 2006; 5:191–203. PMID: 16961079.

3. North RB, Wetzel FT. Spinal cord stimulation for chronic pain of spinal origin: a valuable long-term solution. Spine. 2002; 27:2584–2591. PMID: 12435997.

4. Oakley JC. Spinal cord stimulation: patient selection, technique, and outcomes. Neurosurg Clin N Am. 2003; 14:365–380. PMID: 14567138.

5. Quigley DG, Arnold J, Eldridge PR, Cameron H, McIvor K, Miles JB, et al. Long-term outcome of spinal cord stimulation and hardware complications. Stereotact Funct Neurosurg. 2003; 81:50–56. PMID: 14742964.

6. North RB, Kidd DH, Zahurak M, James CS, Long DM. Spinal cord stimulation for chronic, intractable pain: experience over two decades. Neurosurgery. 1993; 32:384–394. PMID: 8455763.
7. Taylor RS, Van Buyten JP, Buchser E. Spinal cord stimulation for chronic back and leg pain and failed back surgery syndrome: a systematic review and analysis of prognostic factors. Spine. 2005; 30:152–160. PMID: 15626996.

8. ten Vaarwerk IA, Staal MJ. Spinal cord stimulation in chronic pain syndromes. Spinal Cord. 1998; 36:671–682. PMID: 9800271.

9. Turner JA, Loeser JD, Deyo RA, Sanders SB. Spinal cord stimulation for patients with failed back surgery syndrome or complex regional pain syndrome: a systematic review of effectiveness and complications. Pain. 2004; 108:137–147. PMID: 15109517.

10. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004; 100(3 Suppl):254–267. PMID: 15029914.

11. Turner JA, Loeser JD, Bell KG. Spinal cord stimulation for chronic low back pain: a systematic literature synthesis. Neurosurgery. 1995; 37:1088–1095. PMID: 8584149.
12. Rainov NG, Heidecke V. Hardware failures in spinal cord stimulation (SCS) for chronic benign pain of spinal origin. Acta Neurochir Suppl. 2007; 97:101–104. PMID: 17691363.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download