1. Bruce J, Huh YS, Cooney DR, Karp MP, Allen JE, Jewett TC Jr. Intussusception: evolution of current management. J Pediatr Gastroenterol Nutr. 1987; 6(5):663–674. PMID:
3320323.
2. Fischer TK, Bihrmann K, Perch M, Koch A, Wohlfahrt J, Kåre M, et al. Intussusception in early childhood: a cohort study of 1.7 million children. Pediatrics. 2004; 114(3):782–785. PMID:
15342854.

3. Yap Shiyi E, Ganapathy S. Intussusception in Children Presenting to the Emergency Department: an Asian Perspective. Pediatr Emerg Care. 2017; 33(6):409–413. PMID:
26555309.
4. Dias AR, Lopes RI, do Couto RC, Bonafe WW, D'Angelo L, Salvestro ML. Ileal duplication causing recurrent intussusception. J Surg Educ. 2007; 64(1):51–53. PMID:
17320807.

5. Kim KH, Kang KA, Lim JH, Lee KG, Kwon TJ. Inverted Meckel diverticulum as a lead point of small bowel intussusception: misinterpreting case as a lipoma. Clin Imaging. 2016; 40(5):840–842. PMID:
27179156.

6. Ntoulia A, Tharakan SJ, Reid JR, Mahboubi S. Failed intussusception reduction in children: correlation between radiologic, surgical, and pathologic findings. AJR Am J Roentgenol. 2016; 207(2):424–433. PMID:
27224637.

7. Siminas S, Qasem E, Shukla R, Turnock R. Inflammatory fibroid polyp: a rare benign tumor of the alimentary tract in children presenting as intussusception-case report and review of literature. European J Pediatr Surg Rep. 2014; 2(1):16–19.
8. Lee DH, Kim SJ, Lee HJ, Jang HJ. Identifying predictive factors for the recurrence of pediatric intussusception. Pediatr Gastroenterol Hepatol Nutr. 2019; 22(2):142–151. PMID:
30899690.

9. Bhisitkul DM, Todd KM, Listernick R. Adenovirus infection and childhood intussusception. Am J Dis Child. 1992; 146(11):1331–1333. PMID:
1415074.

10. Burnett E, Kabir F, Van Trang N, Rayamajhi A, Satter SM, Liu J, et al. Infectious etiologies of intussusception among children <2 years old in 4 Asian countries. J Infect Dis. 2020; 221(9):1499–1505. PMID:
31754717.

11. Lappalainen S, Ylitalo S, Arola A, Halkosalo A, Räsänen S, Vesikari T. Simultaneous presence of human herpesvirus 6 and adenovirus infections in intestinal intussusception of young children. Acta Paediatr. 2012; 101(6):663–670. PMID:
22296119.

12. Hsu HY, Kao CL, Huang LM, Ni YH, Lai HS, Lin FY, et al. Viral etiology of intussusception in Taiwanese childhood. Pediatr Infect Dis J. 1998; 17(10):893–898. PMID:
9802631.

13. Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020; 91(1):157–160. PMID:
32191675.
14. Caristia S, Ferranti M, Skrami E, Raffetti E, Pierannunzio D, Palladino R, et al. Effect of national and local lockdowns on the control of COVID-19 pandemic: a rapid review. Epidemiol Prev. 2020; 44(5-6):Suppl 2. 60–68. PMID:
33412795.
15. Park S, Kim B, Lee J. Social distancing and outdoor physical activity during the COVID-19 outbreak in South Korea: implications for physical distancing strategies. Asia Pac J Public Health. 2020; 32(6-7):360–362. PMID:
32667221.

16. Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020; 39(12):e423–e427. PMID:
32773660.

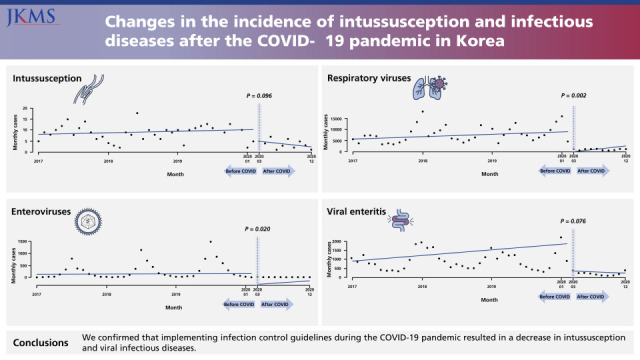
17. Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. 2021; 36(24):e180. PMID:
34155841.

18. Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the coronavirus disease-2019 pandemic on childhood obesity and vitamin D status. J Korean Med Sci. 2021; 36(3):e21. PMID:
33463095.

19. Noh JY, Seong H, Yoon JG, Song JY, Cheong HJ, Kim WJ. Social distancing against COVID-19: implication for the control of influenza. J Korean Med Sci. 2020; 35(19):e182. PMID:
32419400.

21. Seo S, Suda K, Kato H, Abe E, Kosaka S, Fujiwara K, et al. Decreased incidence of intussusception during the COVID-19 pandemic. Trends in pediatric surgical emergencies. Pediatr Surg Int. 2021; 37(12):1761–1764. PMID:
34471948.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download