1. Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018; 392(10158):1662–1671. PMID:
30496081.
2. Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004; 86(5):963–974. PMID:
15118039.
3. Badley EM, Crotty M. An international comparison of the estimated effect of the aging of the population on the major cause of disablement, musculoskeletal disorders. J Rheumatol. 1995; 22(10):1934–1940. PMID:
8991994.
4. Yoo JI, Jang SY, Cha Y, Choy WS, Koo KH. Comparison of mortality, length of hospital stay and transfusion between hemiarthroplasty and total hip arthroplasty in octo- and nonagenarian patients with femoral neck fracture: a nationwide study in Korea. J Korean Med Sci. 2021; 36(45):e300. PMID:
34811975.
5. Swarup I, Shields M, Mayer EN, Hendow CJ, Burket JC, Figgie MP. Outcomes after total hip arthroplasty in young patients with osteonecrosis of the hip. Hip Int. 2017; 27(3):286–292. PMID:
28165595.
6. Lee WY, Hwang DS, Noh CK. Descriptive epidemiology of patients undergoing total hip arthroplasty in Korea with focus on incidence of femoroacetabular impingement: single center study. J Korean Med Sci. 2017; 32(4):581–586. PMID:
28244282.
7. Rothman RH, Cohn JC. Cemented versus cementless total hip arthroplasty. A critical review. Clin Orthop Relat Res. 1990; (254):153–169.
8. Loppini M, Grappiolo G. Uncemented short stems in primary total hip arthroplasty: the state of the art. EFORT Open Rev. 2018; 3(5):149–159. PMID:
29951251.
9. Yoon PW, Lee YK, Ahn J, Jang EJ, Kim Y, Kwak HS, et al. Epidemiology of hip replacements in Korea from 2007 to 2011. J Korean Med Sci. 2014; 29(6):852–858. PMID:
24932089.
10. Lim JY, Park HJ, Lee YK, Ha YC, Koo KH. Comparison of bone preservation in elderly patients with femoral neck fracture after bipolar hemiarthroplasty using shorter femoral stem and standard femoral stem. Indian J Orthop. 2020; 54(6):868–878. PMID:
33133410.
11. Won SH, Park JW, Lee YK, Ha YC, Koo KH. No clinically important differences in thigh pain or bone loss between short stems and conventional-length stems in THA: a randomized clinical trial. Clin Orthop Relat Res. 2021; 479(4):767–777. PMID:
33009239.
12. Sluimer JC, Hoefnagels NH, Emans PJ, Kuijer R, Geesink RG. Comparison of two hydroxyapatite-coated femoral stems: clinical, functional, and bone densitometry evaluation of patients randomized to a regular or modified hydroxyapatite-coated stem aimed at proximal fixation. J Arthroplasty. 2006; 21(3):344–352. PMID:
16627141.
13. Ferguson RJ, Broomfield JA, Malak TT, Palmer AJ, Whitwell D, Kendrick B, et al. Primary stability of a short bone-conserving femoral stem: a two-year randomized controlled trial using radiostereometric analysis. Bone Joint J. 2018; 100-B(9):1148–1156. PMID:
30168759.
14. Nakaya R, Takao M, Hamada H, Sakai T, Sugano N. Reproducibility of the Dorr classification and its quantitative indices on plain radiographs. Orthop Traumatol Surg Res. 2019; 105(1):17–21. PMID:
30594598.
15. Schilcher J, Ivarsson I, Perlbach R, Palm L. No difference in periprosthetic bone loss and fixation between a standard-length stem and a shorter version in cementless total hip arthroplasty. A randomized controlled trial. J Arthroplasty. 2017; 32(4):1220–1226. PMID:
27993496.
16. Freitag T, Hein MA, Wernerus D, Reichel H, Bieger R. Bone remodelling after femoral short stem implantation in total hip arthroplasty: 1-year results from a randomized DEXA study. Arch Orthop Trauma Surg. 2016; 136(1):125–130. PMID:
26613788.
17. Amendola RL, Goetz DD, Liu SS, Callaghan JJ. Two- to 4-year followup of a short stem THA construct: excellent fixation, thigh pain a concern. Clin Orthop Relat Res. 2017; 475(2):375–383. PMID:
27417852.
18. Kim YH, Choi Y, Kim JS. Comparison of bone mineral density changes around short, metaphyseal-fitting, and conventional cementless anatomical femoral components. J Arthroplasty. 2011; 26(6):931–940.e1. PMID:
21130598.
19. Namba RS, Keyak JH, Kim AS, Vu LP, Skinner HB. Cementless implant composition and femoral stress. A finite element analysis. Clin Orthop Relat Res. 1998; (347):261–267.
20. Salemyr M, Muren O, Ahl T, Bodén H, Eisler T, Stark A, et al. Lower periprosthetic bone loss and good fixation of an ultra-short stem compared to a conventional stem in uncemented total hip arthroplasty. Acta Orthop. 2015; 86(6):659–666. PMID:
26134386.
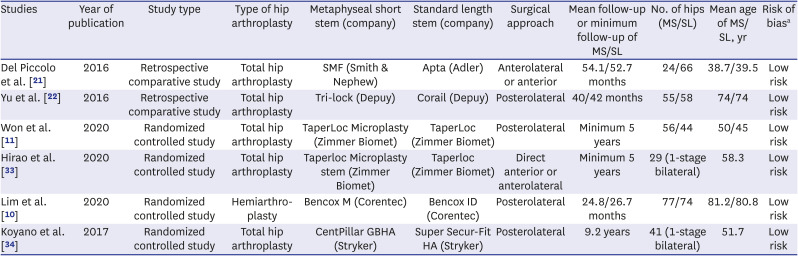
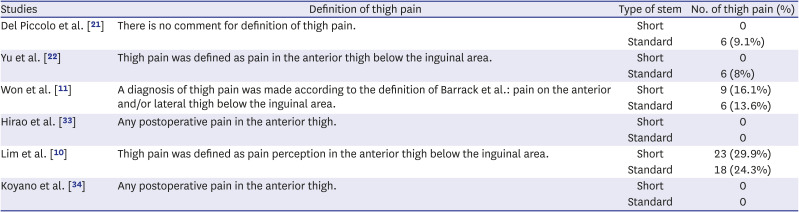
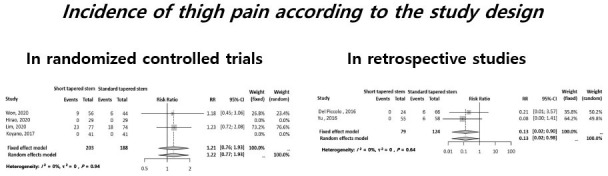
21. Del Piccolo N, Carubbi C, Mazzotta A, Sabbioni G, Filanti M, Stagni C, et al. Return to sports activity with short stems or standard stems in total hip arthroplasty in patients less than 50 years old. Hip Int. 2016; 26(Suppl 1):48–51. PMID:
27174064.
22. Yu H, Liu H, Jia M, Hu Y, Zhang Y. A comparison of a short versus a conventional femoral cementless stem in total hip arthroplasty in patients 70 years and older. J Orthop Surg. 2016; 11(1):33.
23. Khanuja HS, Banerjee S, Jain D, Pivec R, Mont MA. Short bone-conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am. 2014; 96(20):1742–1752. PMID:
25320202.
24. Liang HD, Yang WY, Pan JK, Huang HT, Luo MH, Zeng LF, et al. Are short-stem prostheses superior to conventional stem prostheses in primary total hip arthroplasty? A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2018; 8(9):e021649.
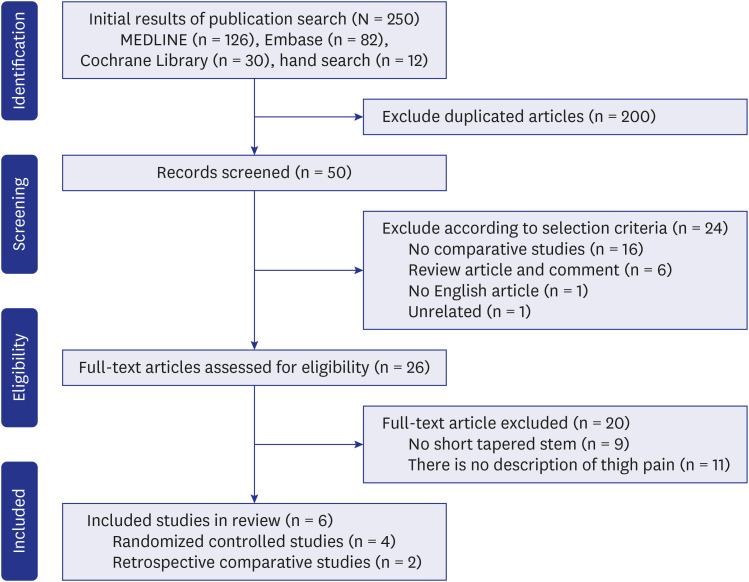
25. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009; 62(10):e1–34. PMID:
19631507.
26. Beaudet K. The Cochrane Collaboration and meta-analysis of clinical data. Am Orthopt J. 2010; 60(1):6–8. PMID:
21061877.
27. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327(7414):557–560. PMID:
12958120.
28. Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007; 335(7626):914–916. PMID:
17974687.
29. Mittlböck M, Heinzl H. A simulation study comparing properties of heterogeneity measures in meta-analyses. Stat Med. 2006; 25(24):4321–4333. PMID:
16991104.
30. Duval S, Tweedie R. A nonparametric “Trim and Fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000; 95(449):89–98.
31. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. PMID:
22008217.
33. Hirao M, Miyatake K, Koga D, Takada R, Koyano G, Okawa A, et al. Comparison of 5-year postoperative results between standard-length stems and short stems in one-stage bilateral total hip arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol. 2021; 31(4):743–753. PMID:
33169175.
34. Koyano G, Jinno T, Koga D, Yamauchi Y, Muneta T, Okawa A. Comparison of bone remodeling between an anatomic short stem and a straight stem in 1-stage bilateral total hip arthroplasty. J Arthroplasty. 2017; 32(2):594–600. PMID:
27554784.
35. Hu H, Liu Z, Liu B, Ding X, Liu S, Wu T, et al. Comparison of clinical outcomes, radiological outcomes and bone remodeling outcomes between proximal coated single-wedge new stem and full coated dual-wedge classic stem in 1-stage bilateral total hip arthroplasty. Med Sci Monit. 2020; 26:e921847. PMID:
32001666.
36. Brown TE, Larson B, Shen F, Moskal JT. Thigh pain after cementless total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2002; 10(6):385–392. PMID:
12470040.
37. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987; 69(1):45–55. PMID:
3818732.
38. Burkart BC, Bourne RB, Rorabeck CH, Kirk PG. Thigh pain in cementless total hip arthroplasty. A comparison of two systems at 2 years’ follow-up. Orthop Clin North Am. 1993; 24(4):645–653. PMID:
8414430.
39. Moreland JR, Bernstein ML. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995; (319):141–150.
40. Bourne RB, Rorabeck CH, Ghazal ME, Lee MH. Pain in the thigh following total hip replacement with a porous-coated anatomic prosthesis for osteoarthrosis. A five-year follow-up study. J Bone Joint Surg Am. 1994; 76(10):1464–1470. PMID:
7929493.
41. Nam D, Nunley RM, Sauber TJ, Johnson SR, Brooks PJ, Barrack RL. Incidence and location of pain in young, active patients following hip arthroplasty. J Arthroplasty. 2015; 30(11):1971–1975. PMID:
26067707.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download