1. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2021. Accessed September 30, 2021.
https://covid19.who.int/
.
3. Han MS, Choi EH, Chang SH, Jin BL, Lee EJ, Kim BN, et al. Clinical characteristics and viral RNA detection in children with coronavirus disease 2019 in the Republic of Korea. JAMA Pediatr. 2021; 175(1):73–80. PMID:
32857112.

4. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020; 145(6):e20200702. PMID:
32179660.

5. Borrelli M, Corcione A, Castellano F, Fiori Nastro F, Santamaria F. Coronavirus disease 2019 in children. Front Pediatr. 2021; 9:668484. PMID:
34123972.

6. Shekerdemian LS, Mahmood NR, Wolfe KK, Riggs BJ, Ross CE, McKiernan CA, et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020; 174(9):868–873. PMID:
32392288.

7. Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, et al. Multi-system inflammatory syndrome in children & adolescents (MIS-C): a systematic review of clinical features and presentation. Paediatr Respir Rev. 2021; 38:51–57. PMID:
32891582.
8. Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the COVID-19 pandemic in Paris, France: prospective observational study. BMJ. 2020; 369:m2094. PMID:
32493739.

11. Delahoy MJ, Ujamaa D, Whitaker M, O’Halloran A, Anglin O, Burns E, et al. Hospitalizations associated with COVID-19 among children and adolescents - COVID-NET, 14 States, March 1, 2020-August 14, 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(36):1255–1260. PMID:
34499627.
12. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013; 66(4):408–414. PMID:
23337781.

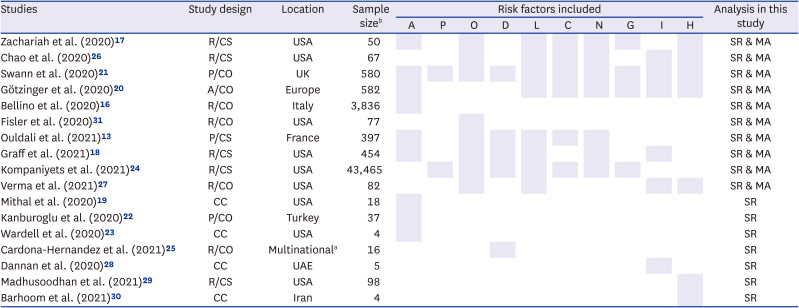
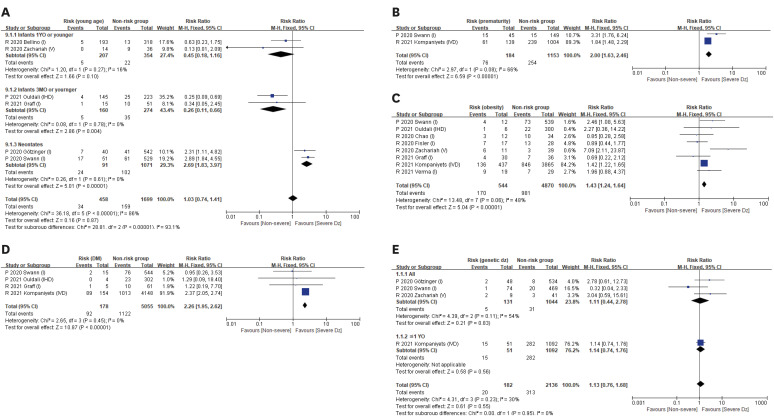
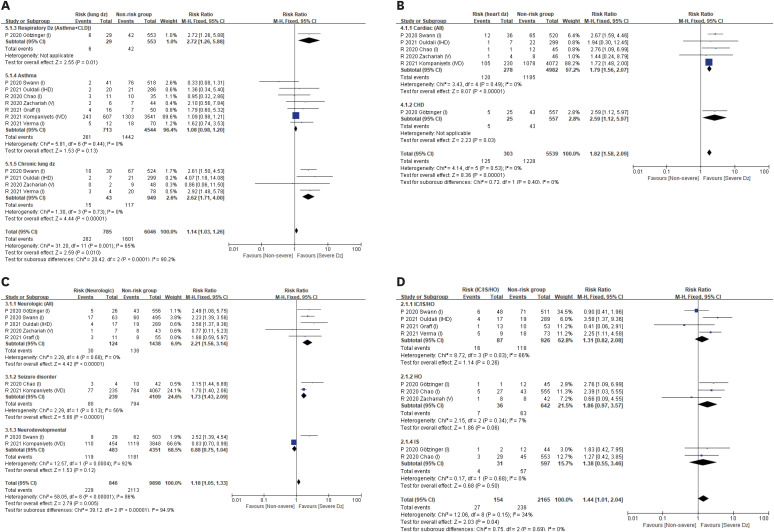
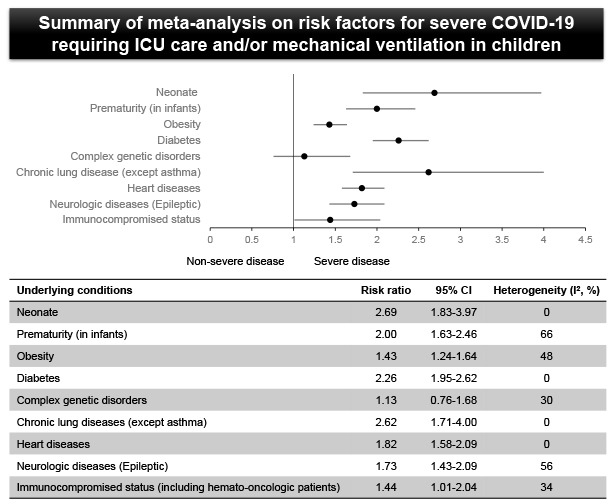
13. Ouldali N, Yang DD, Madhi F, Levy M, Gaschignard J, Craiu I, et al. Factors associated with severe SARS-CoV-2 infection. Pediatrics. 2021; 147(3):e2020023432. PMID:
33323493.

14. Tsabouri S, Makis A, Kosmeri C, Siomou E. Risk factors for severity in children with coronavirus disease 2019: a comprehensive literature review. Pediatr Clin North Am. 2021; 68(1):321–338. PMID:
33228941.
15. Williams N, Radia T, Harman K, Agrawal P, Cook J, Gupta A. COVID-19 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review of critically unwell children and the association with underlying comorbidities. Eur J Pediatr. 2021; 180(3):689–697. PMID:
32914200.

16. Bellino S, Punzo O, Rota MC, Del Manso M, Urdiales AM, Andrianou X, et al. COVID-19 disease severity risk factors for pediatric patients in Italy. Pediatrics. 2020; 146(4):e2020009399. PMID:
32665373.

17. Zachariah P, Johnson CL, Halabi KC, Ahn D, Sen AI, Fischer A, et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York city, New York. JAMA Pediatr. 2020; 174(10):e202430. PMID:
32492092.

18. Graff K, Smith C, Silveira L, Jung S, Curran-Hays S, Jarjour J, et al. Risk factors for severe COVID-19 in children. Pediatr Infect Dis J. 2021; 40(4):e137–e145. PMID:
33538539.

19. Mithal LB, Machut KZ, Muller WJ, Kociolek LK. SARS-CoV-2 infection in infants less than 90 days old. J Pediatr. 2020; 224:150–152. PMID:
32565095.
20. Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020; 4(9):653–661. PMID:
32593339.

21. Swann OV, Holden KA, Turtle L, Pollock L, Fairfield CJ, Drake TM, et al. Clinical characteristics of children and young people admitted to hospital with COVID-19 in United Kingdom: prospective multicentre observational cohort study. BMJ. 2020; 370:m3249. PMID:
32960186.

22. Kanburoglu MK, Tayman C, Oncel MY, Akin IM, Can E, Demir N, et al. A multicentered study on epidemiologic and clinical characteristics of 37 neonates with community-acquired COVID-19. Pediatr Infect Dis J. 2020; 39(10):e297–e302. PMID:
32932329.

23. Wardell H, Campbell JI, VanderPluym C, Dixit A. Severe acute respiratory syndrome coronavirus 2 infection in febrile neonates. J Pediatric Infect Dis Soc. 2020; 9(5):630–635. PMID:
32645175.

24. Kompaniyets L, Agathis NT, Nelson JM, Preston LE, Ko JY, Belay B, et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw Open. 2021; 4(6):e2111182. PMID:
34097050.

25. Cardona-Hernandez R, Cherubini V, Iafusco D, Schiaffini R, Luo X, Maahs DM. Children and youth with diabetes are not at increased risk for hospitalization due to COVID-19. Pediatr Diabetes. 2021; 22(2):202–206. PMID:
33205546.
26. Chao JY, Derespina KR, Herold BC, Goldman DL, Aldrich M, Weingarten J, et al. Clinical characteristics and outcomes of hospitalized and critically ill children and adolescents with coronavirus disease 2019 at a tertiary care medical center in New York city. J Pediatr. 2020; 223:14–19.e2. PMID:
32407719.

27. Verma S, Lumba R, Dapul HM, Gold-von Simson G, Phoon CK, Lighter JL, et al. Characteristics of hospitalized children with SARS-CoV-2 in the New York city metropolitan area. Hosp Pediatr. 2021; 11(1):71–78. PMID:
33033078.

28. El Dannan H, Al Hassani M, Ramsi M. Clinical course of COVID-19 among immunocompromised children: a clinical case series. BMJ Case Rep. 2020; 13(10):e237804.

29. Madhusoodhan PP, Pierro J, Musante J, Kothari P, Gampel B, Appel B, et al. Characterization of COVID-19 disease in pediatric oncology patients: The New York-New Jersey regional experience. Pediatr Blood Cancer. 2021; 68(3):e28843. PMID:
33338306.

30. Barhoom D, Mohseni R, Hamidieh AA, Mohammadpour M, Sharifzadeh M, Navaeian A, et al. Clinical effects of COVID-19 on hematopoietic stem cell transplant outcomes in pediatric patients. Exp Clin Transplant. 2021; 19(5):501–507. PMID:
34053422.

31. Fisler G, Izard SM, Shah S, Lewis D, Kainth MK, Hagmann SHF, et al. Characteristics and risk factors associated with critical illness in pediatric COVID-19. Ann Intensive Care. 2020; 10(1):171. PMID:
33340348.

32. Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late-preterm and term singleton infants in the United States, 1995-2002. J Pediatr. 2007; 151(5):450–456. –456.e1. PMID:
17961684.

33. Gunville CF, Sontag MK, Stratton KA, Ranade DJ, Abman SH, Mourani PM. Scope and impact of early and late preterm infants admitted to the PICU with respiratory illness. J Pediatr. 2010; 157(2):209–214.e1. PMID:
20338574.

34. Wu ZH, Tang Y, Cheng Q. Diabetes increases the mortality of patients with COVID-19: a meta-analysis. Acta Diabetol. 2021; 58(2):139–144. PMID:
32583078.

35. Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19 related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March - December 2020. MMWR Morb Mortal Wkly Rep. 2021; 70(10):355–361. PMID:
33705371.
36. Zhou Y, Chi J, Lv W, Wang Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19). Diabetes Metab Res Rev. 2021; 37(2):e3377. PMID:
32588943.

37. Knapp S. Diabetes and infection: is there a link?--A mini-review. Gerontology. 2013; 59(2):99–104. PMID:
23182884.
38. Yang JK, Feng Y, Yuan MY, Yuan SY, Fu HJ, Wu BY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006; 23(6):623–628. PMID:
16759303.

39. Banik GR, Alqahtani AS, Booy R, Rashid H. Risk factors for severity and mortality in patients with MERS-CoV: analysis of publicly available data from Saudi Arabia. Virol Sin. 2016; 31(1):81–84. PMID:
26826080.

40. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020; 323(16):1574–1581. PMID:
32250385.

41. Sarkar S, Das D, Borsingh Wann S, Kalita J, Manna P. Is diabetes mellitus a wrongdoer to COVID-19 severity? Diabetes Res Clin Pract. 2021; 178:108936. PMID:
34217771.

42. Checchia PA, Paes B, Bont L, Manzoni P, Simões EA, Fauroux B, et al. Defining the risk and associated morbidity and mortality of severe respiratory syncytial virus infection among infants with congenital heart disease. Infect Dis Ther. 2017; 6(1):37–56. PMID:
28070870.

43. Galleguillos C, Galleguillos B, Larios G, Menchaca G, Bont L, Castro-Rodriguez JA. Down’s syndrome is a risk factor for severe lower respiratory tract infection due to respiratory syncytial virus. Acta Paediatr. 2016; 105(11):e531–e535. PMID:
27537430.

44. Pham H, Thompson J, Wurzel D, Duke T. Ten years of severe respiratory syncytial virus infections in a tertiary paediatric intensive care unit. J Paediatr Child Health. 2020; 56(1):61–67. PMID:
31095832.

45. Castro-Rodriguez JA, Forno E. Asthma and COVID-19 in children: a systematic review and call for data. Pediatr Pulmonol. 2020; 55(9):2412–2418. PMID:
32558360.
46. Lovinsky-Desir S, Deshpande DR, De A, Murray L, Stingone JA, Chan A, et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020; 146(5):1027–1034.e4. PMID:
32771560.

47. Lee SC, Son KJ, Han CH, Jung JY, Park SC. Impact of comorbid asthma on severity of coronavirus disease (COVID-19). Sci Rep. 2020; 10(1):21805. PMID:
33311519.

48. Malle L, Gao C, Hur C, Truong HQ, Bouvier NM, Percha B, et al. Individuals with Down syndrome hospitalized with COVID-19 have more severe disease. Genet Med. 2021; 23(3):576–580. PMID:
33060835.

49. Newman AM, Jhaveri R, Patel AB, Tan TQ, Toia JM, Arshad M. Trisomy 21 and coronavirus disease 2019 in pediatric patients. J Pediatr. 2021; 228:294–296. PMID:
32861693.

50. Kantar A, Mazza A, Bonanomi E, Odoni M, Seminara M, Verde ID, et al. COVID-19 and children with Down syndrome: is there any real reason to worry? Two case reports with severe course. BMC Pediatr. 2020; 20(1):561. PMID:
33339516.

51. Bowen A, Miller AD, Zambrano LD, Wu MJ, Oster ME, Godfred-Cato S, et al. Demographic and clinical factors associated with death among persons <21 years old with multisystem inflammatory syndrome in children-United States, February 2020-March 2021. Open Forum Infect Dis. 2021; 8(8):ofab388. PMID:
34409123.

52. Lee H, Choi S, Park JY, Jo DS, Choi UY, Lee H, et al. Analysis of critical COVID-19 cases among children in Korea. J Korean Med Sci. 2022; 37(1):e13. PMID:
34981683.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download