Abstract
The Paraneoplastic syndromes include the disorders that accompany benign or malignant tumors but are not directly related to mass effects or invasion by the primary tumor or its metastases. Neoplastic cells can produce a variety of peptides that exert biologic actions at local and distant sites and can elicit responses that cause a variety of hormonal, hematologic, dermatologic and neurologic symptoms. Almost every type of malignancy has the potential to produce hormones or cytokines or to induce immunologic responses. Lung cancers, both non-small cell and small cell, are capable of producing a variety of paraneoplastic syndromes. The majority of such syndromes are caused by small cell carcinomas, including many endocrinopathies. Syndrome of inappropriate antidiuretic hormone (SIADH) has been commonly associated with small cell carcinoma and is often seen in these patients. However, SIADH associated with squamous cell carcinoma has rarely been reported on, and the mechanism for this rare association is still unknown. We present here a case of a 77-yr-old man who developed SIADH caused by squamous cell carcinoma of the nasopharynx.
Syndrome of inappropriate antidiuretic hormone (SIADH) is often associated with cancer. Approximately 67% of SIADH cases are reported to be caused by cancer, the majority of which (70%) are linked to small cell carcinoma of the lung (1). Head and neck cancers are responsible for only 1.5% of SIADH cases; however, the majority of these cases have the histology of small cell carcinoma (2). There have been scant reports of squamous cell carcinoma as a cause of SIADH and, even more rarely, squamous cell carcinoma of the head and neck. This report describes a patient who was found to have squamous cell carcinoma of the nasopharynx and later developed SIADH following neck dissection.
A 77-year-old Caucasian man presented to the ENT clinic with a 3 month history of progressive nonproductive cough. He had a social history of smoking, one pack a day for 50 yr. He denied a recent history of weight loss, fatigue, fever and chills. His regular check-up excludes any other possibility for unknown diseases, including renal failure or heart failure. He had a past surgical history of coronary artery bypass graft (CABG). Upon physical examination, the patient was found to have a tonsilar mass. A biopsy of the mass was ordered and the tissue sample demonstrated transformation to squamous cell carcinoma. The patient then underwent modified radical neck dissection without sacrificed internal jugular vein, which was carried out by our hospital's head and neck cancer team.
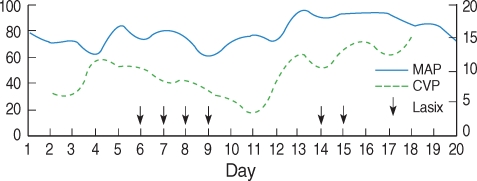
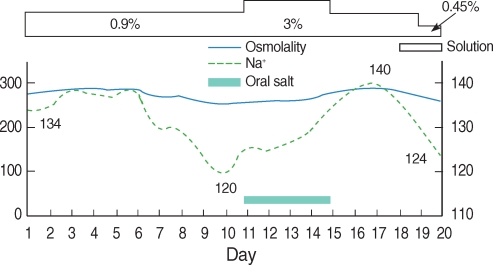
On post-operative day 2, a Doppler Ultrasound (US) detected deep vein thrombosis (DVT) in the patient's left arm which prompted us to start him on heparin (Lovenox). On post-operative day 6, the patient developed pulmonary edema, and a loop diuretic (furosemide, Lasix) was then added to his treatment. The echocardiography showed normal ventricular function. On post-operative day 10, he presented with lethargy, 2+ peripheral edema and a central venous pressure (CVP) of 6 mmHg (Fig. 1). The laboratory results included a serum Na+ of 120 mmol/L, a serum K+ level of 4.7 mmol/L, a serum osmolality of 265 mOsm/kg, a pH of 7.46, a pCO2 of 53 mmHg and HCO3- of 35 mmol/L. The urine analysis showed an osmolality of 390 mOsm/kg, a urinary Na+ of 142 mmol/L and fractional excretion of sodium >1%. This was followed by thyroid function tests and an ACTH stimulation test, the results of which were found to be within normal limits, eliminating hypothyroidism and adrenal insufficiency as possible causes for the patient's electrolyte disturbance (Fig. 2).
After an extensive work-up, a diagnosis of SIADH was established, and the patient was treated with 1 g/day of oral salt and 3% hypertonic saline. In addition to this, the diuretic was discontinued to avoid aggravating the hyponatremia. By his post-operative day 15, his serum Na+ had normalized. The oral salt was then placed on hold, and 0.9% normal saline was started. On the morning of post-operative day 20, the patient's blood pressure temporarily dropped from a normal range to 70/57 mmHg. However, it was quickly discovered that the patient was mistakenly receiving 0.45% hypotonic saline instead of 0.9% normal saline. At this point, the patient had already received approximately 1,320 mL of half-normal saline for 4 hr, and in addition to the drop in his blood pressure, he became confused and then started vomiting. The half-normal saline was instantly stopped and his serum Na+ was checked, and it was found to be 124 mmol/L. Unfortunately, his clinical condition deteriorated very quickly, with his blood pressure continuing to drop. Cardiopulmonary resuscitation (CPR) was then performed with no response and the patient finally expired. An autopsy was denied by the family.
SIADH was first described in two patients with bronchogenic small cell carcinoma in 1957 by Schwartz (3). At the time, Schwartz suggested that small cell carcinoma produced some quantity of antidiuretic hormone, which was later found to consist of arginine vasopressin (AVP) by Bleich HL in 1976. Bleich also discovered the AVP-regulated water channels in the kidneys that were later termed "aquaporins" (4). Schwartz's hypothesis was proven by detecting ectopic AVP in small cell carcinoma (5). This hypothesis was further confirmed by expression analysis of the AVP-NP II gene, which controls the production of AVP, in small cell carcinoma cells. These findings established the well accepted mechanism of action of SIADH caused by small cell carcinoma (6). In 1976, Moses was the first to describe SIADH in patients with sqamous cell carcinoma, but the mechanism by which it occurs was not discovered and it has not been demonstrated since (7). There has not been a proven or widely accepted theory explaining SIADH caused by squamous cell carcinoma.
Although many researchers have found AVP gene not only in small cell carcinoma but also in undifferentiated carcinoma (8) and anaplastic carcinoma (9), they have failed to find AVP gene in squamous cell carcinoma. However, some neuropeptides related to AVP have been detected in squamous cell carcinoma. AVP is secreted from the posterior pituitary gland after being synthesized in the hypothalamus. This course is stimulated by neuropeptides such as acetylcholine, histamine, bradykinin, angiotensin II and neuropeptide Y (10, 11). In 2004, Lee demonstrated a significant increase of neuropeptide Y in the hypothalamus of a mouse that was inoculated with human squamous cell carcinoma (11). These findings led him to suggest that squamous cell carcinoma produced neuropeptide Y, which stimulated production of endogenous AVP, while small cell carcinoma produced ectopic AVP directly. In addition, there has been more compelling evidence to support Lee's theory, such as the finding of increased AVP levels in 38% of SIADH patients with squamous cell carcinoma, despite no evidence of ectopic AVP (12). In the event that neuropeptide Y is detected in SIADH patients with squamous cell carcinoma, this hypothesis can be proven clinically.
In addition to SIADH association with a number of malignancies (most notably small-cell cancer of the lung), SIADH can also occur following head injury, surgery (following neck dissection and manipulation of the nervous system), drugs (such as morphine, NSAIDs, and oxytocin) and in a number of pulmonary (pneumonia, abscess, and tuberculosis) and endocrine disease states (hypothyroidism and glucocorticoid deficiency). It should be considered in patients who are euvolemic and hyponatremic with elevated urine sodium (usually greater than 20 mEq/L) and urine osmolality. AVP is an antidiuretic hormone that maintains homeostasis against hypotension and hypovolemia, which is sensed by the baroreceptors in the neck. These baroreceptors are present in the aorta and the internal carotid arteries. When these receptors are stimulated, e.g. via neck dissection, serum AVP will rise as a result of the signaling from the baroreceptors. In 1997, Mesko observed SIADH in 27% of those patients undergoing neck dissection (13). However, when SIADH develops in a cancer patient who has undergone neck dissection, it is uncertain whether the SIADH is a paraneoplastic syndrome or post-operative SIADH.
The mechanism by which patients with squamous cell carcinoma develop SIADH is still unknown. SIADH can be a paraneoplastic syndrome caused by squamous cell carcinoma or a post-operative SIADH caused by neck dissection. Therefore, we will conduct further research on the neuropeptides of squamous cell carcinoma, which may help to prevent SIADH post-neck dissection.
References
1. Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med. 1967; 5. 42(5):790–806. PMID: 5337379.

2. Zohar Y, Talmi YP, Finkelstein Y, Nobel M, Gafter U. Syndrome of inappropriate antidiuretic hormone secretion in cancer of the head and neck. Ann Otol Rhinol Laryngol. 1991; 4. 100(4 Pt 1):341–344. PMID: 2018296.

3. Schwartz WB, Bennett W, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med. 1957; 10. 23(4):529–542. PMID: 13469824.

4. Bleich HL, Boro ES. Antidiuretic hormone. N Engl J Med. 1976; 9. 16. 295(12):659–665. PMID: 184385.

5. Amatruda TT Jr, Mulrow PJ, Gallagher JC, Sawyer WH. Carcinoma of the lung with inappropriate antidiuresis demonstration of antidiuretic-hormone-like activity in tumor extract. N Engl J Med. 1963; 9. 12. 269:544–549. PMID: 14043255.
6. Sausville E, Carney D, Battey J. The human vasopressin gene is linked to the oxytocin gene and is selectively expressed in a cultured lung cancer cell line. J Biol Chem. 1985; 8. 25. 260(18):10236–10241. PMID: 2991279.

7. Moses AM, Miller M, Streeten DH. Pathophysiologic and pharmacologic alterations in the release and action of ADH. Metabolism. 1976; 6. 25(6):697–721. PMID: 818477.

8. Kavanagh BD, Halperin EC, Rosenbaum LC, Shannon EM, Nilaver G. Syndrome of inappropriate secretion of antidiuretic hormone in a patient with carcinoma of the nasopharynx. Cancer. 1992; 3. 15. 69(6):1315–1319. PMID: 1540868.

9. Krmar RT, Ferraris JR, Ruiz SE, Dibar E, Morandi AA, Ramirez JA. Syndrome of inappropriate secretion of antidiuretic hormone in nasopharynx carcinoma. Pediatr Nephrol. 1997; 8. 11(4):502–503. PMID: 9260257.

10. Jacobson L. Hypothalamic-pituitary-adrenocortical axis regulation. Endocrinol Metab Clin North Am. 2005; 6. 34(2):271–292. PMID: 15850842.

11. Lee JH, Cha MJ, Choi SH, Hwang SJ, Kim DG, Jahng JW. Neuropeptide Y immunoreactivity and corticotropin-releasing hormone mRNA level are increased in the hypothalamus of mouse bearing a human oral squamous cell carcinoma. Neuropeptides. 2004; 12. 38(6):345–350. PMID: 15567470.

12. Talmi YP, Wolf GT, Hoffman HT, Krause CJ. Elevated arginine vasopressin levels in squamous cell cancer of the head and neck. Laryngoscope. 1996; 3. 106(3 Pt 1):317–321. PMID: 8614196.

13. Mesko TW, Garcia O, Yee LD, Villar MJ, Chan H. The syndrome of inappropriate secretion of antidiuretic hormone (SIADH) as a consequence of neck dissection. J Laryngol Otol. 1997; 5. 111(5):449–453. PMID: 9205607.





 Citation
Citation Print
Print


 XML Download
XML Download