1. Chiang VW, Baskin MN. Uses and complications of central venous catheters inserted in a pediatric emergency department. Pediatr Emerg Care. 2000; 16:230–232. PMID:
10966338.

2. Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001; 286:700–707. PMID:
11495620.

3. Goetz AM, Wagener MM, Miller JM, Muder RR. Risk of infection due to central venous catheters: effect of site of placement and catheter type. Infect Control Hosp Epidemiol. 1998; 19:842–845. PMID:
9831940.

4. Joynt GM, Kew J, Gomersall CD, Leung VY, Liu EK. Deep venous thrombosis caused by femoral venous catheters in critically ill adult patients. Chest. 2000; 117:178–183. PMID:
10631217.

5. Trottier SJ, Veremakis C, O'Brien J, Auer AI. Femoral deep vein thrombosis associated with central venous catheterization: results from a prospective, randomized trial. Crit Care Med. 1995; 23:52–59. PMID:
8001386.
6. Deshpande KS, Hatem C, Ulrich HL, Currie BP, Aldrich TK, Bryan-Brown CW, et al. The incidence of infectious complications of central venous catheters at the subclavian, internal jugular, and femoral sites in an intensive care unit population. Crit Care Med. 2005; 33:13–20. PMID:
15644643.

7. Lorente L, Jiménez A, Santana M, Iribarren JL, Jiménez JJ, Martin MM, et al. Microorganisms responsible for intravascular catheter-related bloodstream infection according to the catheter site. Crit Care Med. 2007; 35:2424–2427. PMID:
17717493.

8. Parienti JJ, Thirion M, Mégarbane B, Souweine B, Ouchikhe A, Polito A, et al. Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial. JAMA. 2008; 299:2413–2422. PMID:
18505951.

9. Durbec O, Viviand X, Potie F, Vialet R, Martin C. Lower extremity deep vein thrombosis: a prospective, randomized, controlled trial in comatose or sedated patients undergoing femoral vein catheterization. Crit Care Med. 1997; 25:1982–1985. PMID:
9403746.
10. Sznajder JI, Zveibil FR, Bitterman H, Weiner P, Bursztein S. Central vein catheterization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986; 146:259–261. PMID:
3947185.

11. Jastremski MS, Matthias HD, Randell PA. Femoral venous catheterization during cardiopulmonary resuscitation: a critical appraisal. J Emerg Med. 1984; 1:387–391. PMID:
6599946.

12. Stone MB, Price DD, Anderson BS. Ultrasonographic investigation of the effect of reverse Trendelenburg on the cross-sectional area of the femoral vein. J Emerg Med. 2006; 30:211–213. PMID:
16567260.

13. Kim JT, Lee NJ, Na HS, Jeon Y, Kim HS, Kim CS, et al. Ultrasonographic investigation of the effect of inguinal compression on the cross-sectional area of the femoral vein. Acad Emerg Med. 2008; 15:101–103. PMID:
18211323.

14. Suk EH, Kim DH, Kil HK, Kweon TD. Effects of reverse Trendelenburg position and inguinal compression on femoral vein cross-sectional area in infants and young children. Anaesthesia. 2009; 64:399–402. PMID:
19317705.

15. Kim JT, Park CS, Kim HJ, Lee JM, Kim HS, Kim CS, et al. The effect of inguinal compression, Valsalva maneuver, and reverse Trendelenburg position on the cross-sectional area of the femoral vein in children. Anesth Analg. 2009; 108:1493–1496. PMID:
19372327.

16. Werner SL, Jones RA, Emerman CL. Effect of hip abduction and external rotation on femoral vein exposure for possible cannulation. J Emerg Med. 2008; 35:73–75. PMID:
17976787.
17. Junker JA, Totty WG, Stanley RJ, McClennan BL. Computed-tomographic confirmation of femoral vein distension with the Valsalva maneuver. Radiology. 1983; 147:275. PMID:
6828748.

18. Bellazzini MA, Rankin PM, Gangnon RE, Bjoernsen LP. Ultrasound validation of maneuvers to increase internal jugular vein cross-sectional area and decrease compressibility. Am J Emerg Med. 2009; 27:454–459. PMID:
19555617.

19. Clenaghan S, McLaughlin RE, Martyn C, McGovern S, Bowra J. Relationship between Trendelenburg tilt and internal jugular vein diameter. Emerg Med J. 2005; 22:867–868. PMID:
16299195.

20. Gwak MJ, Park JY, Suk EH, Kim DH. Effects of head rotation on the right internal jugular vein in infants and young children. Anaesthesia. 2010; 65:272–276. PMID:
20105152.

21. Verghese ST, Nath A, Zenger D, Patel RI, Kaplan RF, Patel KM. The effects of the simulated Valsalva maneuver, liver compression, and/or Trendelenburg position on the cross-sectional area of the internal jugular vein in infants and young children. Anesth Analg. 2002; 94:250–254. PMID:
11812678.

22. Ryu HG, Lee SJ, Kwon JE, Choi JY, Yoon SZ, Jeon Y, et al. Influence of the head posture on central venous catheter position during right subclavian catheterization. Korean J Anesthesiol. 2007; 52:627–629.

23. Fortune JB, Feustel P. Effect of patient position on size and location of the subclavian vein for percutaneous puncture. Arch Surg. 2003; 138:996–1000. PMID:
12963658.

24. Rodriguez CJ, Bolanowski A, Patel K, Perdue P, Carter W, Lukish JR. Classical positioning decreases the cross-sectional area of the subclavian vein. Am J Surg. 2006; 192:135–137. PMID:
16769291.

25. Williams JF, Seneff MG, Friedman BC, McGrath BJ, Gregg R, Sunner J, et al. Use of femoral venous catheters in critically ill adults: prospective study. Crit Care Med. 1991; 19:550–553. PMID:
2019143.
26. Raad I, Darouiche R, Dupuis J, Abi-Said D, Gabrielli A, Hachem R, et al. The Texas Medical Center Catheter Study Group. Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections. A randomized, double-blind trial. Ann Intern Med. 1997; 127:267–274. PMID:
9265425.
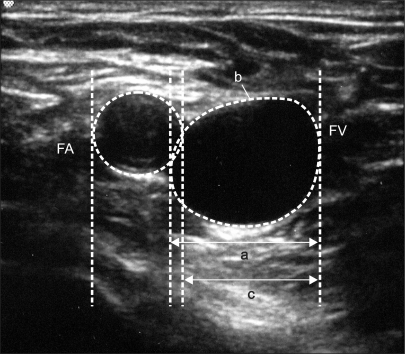
27. Baum PA, Matsumoto AH, Teitelbaum GP, Zuurbier RA, Barth KH. Anatomic relationship between the common femoral artery and vein: CT evaluation and clinical significance. Radiology. 1989; 173:775–777. PMID:
2813785.

28. Warkentine FH, Clyde Pierce M, Lorenz D, Kim IK. The anatomic relationship of femoral vein to femoral artery in euvolemic pediatric patients by ultrasonography: implications for pediatric femoral central venous access. Acad Emerg Med. 2008; 15:426–430. PMID:
18439197.

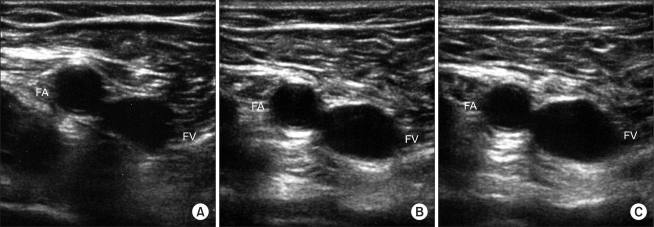
29. Hopkins JW, Warkentine F, Gracely E, Kim IK. The anatomic relationship between the common femoral artery and common femoral vein in frog leg position versus straight leg position in pediatric patients. Acad Emerg Med. 2009; 16:579–584. PMID:
19519804.





 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download