Abstract
Advantages of direct peroral cholangioscopy (POC) using an ultraslim endoscope include use of conventional endoscopy equipment, operation by a single endoscopist, and superior image quality of the biliary tree with easy application of enhanced endoscopy and a large working channel. The major diagnostic indications of this system are an evaluation of biliary strictures, filling defects, or unclear findings on cholangiogram or other imaging studies. Therapeutic application using a direct POC system can be broadened by a larger working channel. However, direct POC is difficult to apply in patients with a narrow diameter bile duct, far distal common bile duct lesion, or failed anchoring of the scope with accessories. An air embolism is a rare complication of direct POC but can be a fatal problem. Cholangitis can also occur during or after the procedure. Use of a CO2 system instead of room air during the POC procedure and administration of antibiotics before and after the procedure are strongly recommended. Continuous development of specialized endoscopes and accessories is expected to facilitate the diagnostic and therapeutic roles of direct POC.
Peroral cholangioscopy (POC) permits direct visualization of the biliary tree for diagnostic procedures and provides endoscopic guidance for therapeutic interventions. Three POC systems are available, including a mother-baby cholangioscopic system, the SpyGlass direct visualization system, and direct POC using an ultraslim upper endoscope.1 POC is traditionally conducted using a mother-baby scope system. However, POC using this system is cumbersome, labor-intensive, and difficult. A small caliber baby scope can be broken easily, is expensive, and difficult to handle with limited irrigation and suction, and it has a small working channel of 1.2-mm diameter. The mother-baby scope system is also operated by two skilled endoscopists using two endoscopic systems. Therefore, routine clinical application of this system has been limited. A single-operator cholangioscopic system has been developed as a new type of POC system, and preliminary results have been reported.2,3 An ultraslim upper endoscope can be advanced into the bile duct through the major papilla. Direct POC using an ultraslim endoscope has been proposed as a single-operator system for direct endoscopic examination of the biliary tree.4
The ultraslim upper endoscope was originally designed for transnasal applications. GIF-XP260NS (Olympus Co., Tokyo, Japan) is a dedicated ultraslim upper endoscope. It has a 5-mm outer diameter with a 2-mm working channel. Direct POC involves directly inserting of an ultraslim upper endoscope into the biliary tree through the papilla. The biliary tract can be visualized under direct POC using a conventional endoscope and controlled by a single operator. This system has three major advantages compared with other POC systems. Direct POC provides high quality endoscopic imaging with the ease of performance of enhanced endoscopy using narrow band imaging (NBI). A large, 2-mm diameter working channel can be extended for interventional procedures, including for tissue sampling, and permits 5-Fr instruments. The direct POC system uses a con ventional endoscope with a standard endoscopic set up by a single operator. Thus, it is an economical solution for POC. The major obstacle for direct POC using an ultraslim endoscope is the relatively acute angle that must be maneuvered from the second part of the duodenal lumen into the biliary system. Therefore, specialized accessories or techniques are necessary to advance an ultraslim endoscope into the proximal biliary system and to improve the success rate of direct POC. An intraductal balloon through the scope permits access, stability, and positioning of the ultraslim endoscope within the biliary system. Direct POC using an intraductal 5-Fr balloon catheter that can be anchored and fixed via ballooning within a branch of the intrahepatic duct or proximal portion of a strictured segment has a high success rate.5
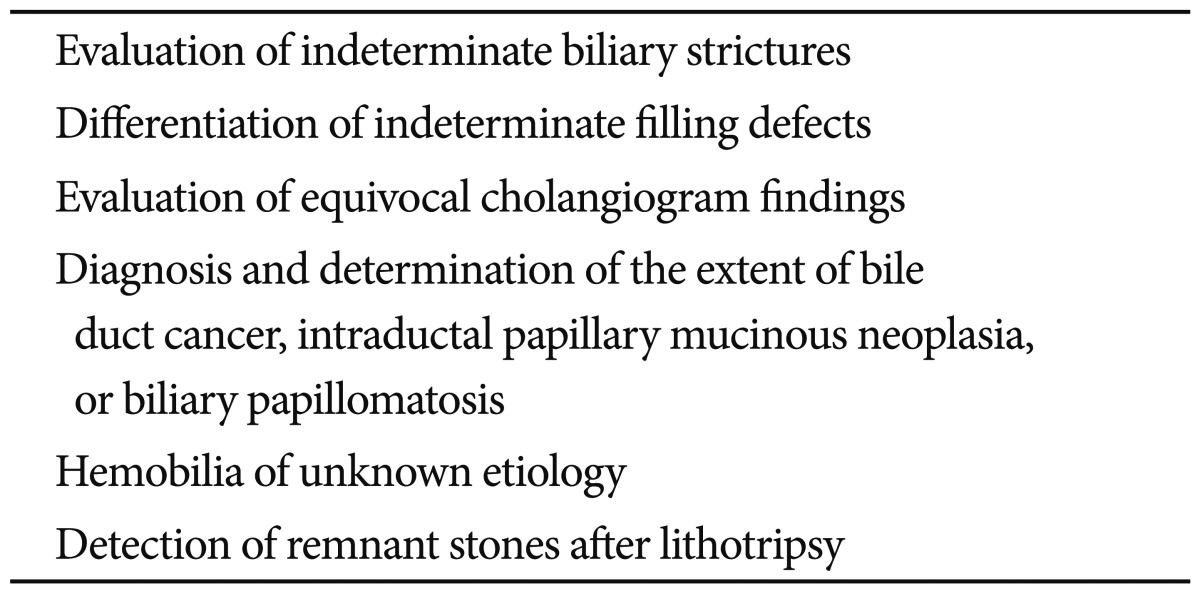
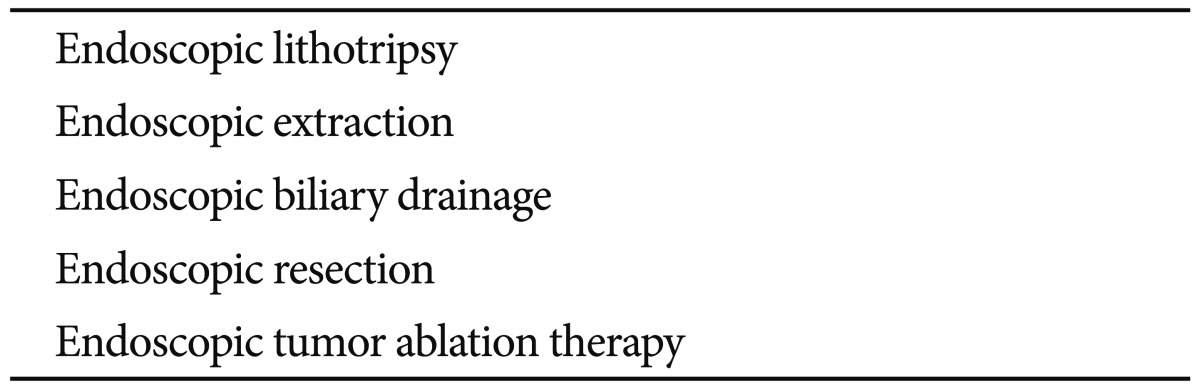
Important diagnostic indications for direct POC are listed in Table 1. Direct intraductal visualization with image-enhanced cholangioscopy and targeted biopsy can provide clues for intraductal biliary lesions. Tissue sampling under direct visualization is a major advantage of direct POC because larger biopsy forceps can be used compared with other POC systems. Enhanced endoscopy can be performed easily with an ultraslim endoscope. NBI shows detailed images of the surface structure and of the mucosal microvessels. Emphasizing mucosal structures by NBI improves the utility of endoscopic images, and it can be used to distinguish neoplastic from normal biliary tract.6 Therapeutic interventions with direct POC can be expanded over those possible with the current mother-baby POC and the SpyGlass system by using a large working channel (Table 2). Intraductal lithotripsy, tumor ablation with photodynamic therapy, or argon plasma coagulation under direct POC is feasible procedures for patients with biliary tract diseases that are not amenable to conventional endoscopy. Endoscopic lithotripsy with electrohydraulic lithotripsy or laser lithotripsy is the most common therapeutic intervention with a high success rate under direct POC.7,8 Endoscopic extraction can be performed by direct POC using a 5-Fr dormia basket or snare. Direct POC is also useful for evaluating residual stones after mechanical lithotripsy for retained common bile duct (CBD) stones. Not only detection of small fragmented stones, but endoscopic removal of stones or fragments can be accomplished under direct visualization using 5-Fr dormia baskets.9 Direct POC can be used to identify other additional pathology, not only fragmented stones. Endoscopic drainage can be performed by direct POC using a 5-Fr catheter or stent, particularly for patients who need selective guidewire access, such as for the orifice of the cystic duct or major intrahepatic branches.10,11
The current direct POC system has several disadvantages. A widely opened ampulla of Vater orifice with a major sphincterotomy is needed. Some cases should be combined with papillary balloon dilation for easy and smooth insertion of the ultraslim scope into the biliary tree. Adverse effects can occur due to the wide opening of the papilla using sphincterotomy with or without a dilated balloon. Direct POC can only be performed with a bile duct dilated >8 mm. Thus, patients with diffused strictures, such as primary sclerosing cholangitis, can be difficult to operate on using direct POC. Anchoring of an intraductal balloon catheter is not always successful. In particular, anchoring and maintaining the balloon is technically very challenging in patients without strictured biliary segment or impacted stones. The 5.0 mm insertion diameter of the ultraslim scope is still thicker than the 3.4 mm of the new baby scope. The current ultraslim scope is not designed for use as a cholangioscope, as it is too flexible, and it is easy to make a loop in the gastric fundus or third portion of the duodenum. The current form of intraductal balloon catheter is cumbersome to use. Anchoring the balloon can make direct POC appear to be a complex procedure. All accessories supporting the scope, such as an intraductal balloon catheter, including the guidewire should be removed from the working channel of the scope to use interventional instruments. This can cause instability in the scope position. The distal tip of the scope can easily dislocate on the distal CBD or fall into the duodenum. The slim POC scope should be exchanged with an duodenoscope during ERCP. New accessories or scopes must be developed to overcome the technical disadvantages of current direct POC. Access balloon catheters for cholangioscopy have been developed for easy exchange of a duodenoscope with a slim endoscope and provide stability and positioning of a slim endoscope in the bile duct.12 A peroral direct cholangioscope prototype is being developed by Olympus with improved performance as a dedicated cholangioscope such as longer working length, two accessory channels, and a short distal bending section.13 A second-generation prototype of the peroral direct cholangioscope with multibending functions for free hand insertion into the bile duct has been evaluated clinically.14
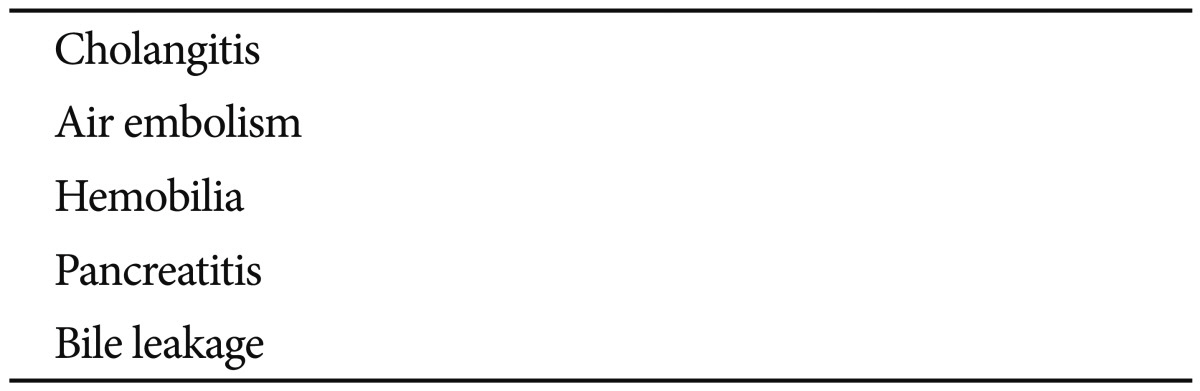
Complications of the POC system are shown in Table 3. The most common complication is cholangitis, which occurs in up to 14% of cases.15 The administration of prophylactic antibiotics is mandatory to minimize the incidence of cholangitis. Irrigated normal saline should be suctioned as much as possible. CO2 insufflation is recommended in cases of purulent bile, rather than large amounts of normal saline. An air embolism is a rare but fatal complication associated with direct POC.16 CO2 insufflation is strongly recommended rather than room air to prevent an air embolism.17 Only minimal air insufflation is required during a biliary examination with POC even with CO2. Irrigation with normal saline instead of air is recommended for good vision. The air supply can be stopped to prevent an air embolism in patients susceptible to an air embolism, such as those with liver cirrhosis.
References
1. Moon JH, Terheggen G, Choi HJ, Neuhaus H. Peroral cholangioscopy: diagnostic and therapeutic applications. Gastroenterology. 2013; 144:276–282. PMID: 23127575.

2. Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006; 63:853–857. PMID: 16650553.

3. Chen YK, Parsi MA, Binmoeller KF, et al. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc. 2011; 74:805–814. PMID: 21762903.

4. Choi HJ, Moon JH, Ko BM, et al. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos). Gastrointest Endosc. 2009; 69:935–940. PMID: 19327480.

5. Moon JH, Ko BM, Choi HJ, et al. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos). Gastrointest Endosc. 2009; 70:297–302. PMID: 19394010.

6. Itoi T, Sofuni A, Itokawa F, et al. Peroral cholangioscopic diagnosis of biliary-tract diseases by using narrow-band imaging (with videos). Gastrointest Endosc. 2007; 66:730–736. PMID: 17905015.

7. Moon JH, Ko BM, Choi HJ, et al. Direct peroral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol. 2009; 104:2729–2733. PMID: 19623165.

8. Kim HI, Moon JH, Choi HJ, et al. Holmium laser lithotripsy under direct peroral cholangioscopy by using an ultra-slim upper endoscope for patients with retained bile duct stones (with video). Gastrointest Endosc. 2011; 74:1127–1132. PMID: 21963070.

9. Lee YN, Moon JH, Choi HJ, et al. Direct peroral cholangioscopy using an ultraslim upper endoscope for management of residual stones after mechanical lithotripsy for retained common bile duct stones. Endoscopy. 2012; 44:819–824. PMID: 22791587.

10. Waxman I, Chennat J, Konda V. Peroral direct cholangioscopic-guided selective intrahepatic duct stent placement with an ultraslim endoscope. Gastrointest Endosc. 2010; 71:875–878. PMID: 19922912.

11. Shin JU, Lee JK, Kim KM, Lee KH, Lee KT. Endoscopic naso-gallbladder drainage by using cholangioscopy for acute cholecystitis combined with cholangitis or choledocholithiasis (with video). Gastrointest Endosc. 2012; 76:1052–1055. PMID: 23078929.

12. Waxman I, Dillon T, Chmura K, Wardrip C, Chennat J, Konda V. Feasibility of a novel system for intraductal balloon-anchored direct peroral cholangioscopy and endotherapy with an ultraslim endoscope (with videos). Gastrointest Endosc. 2010; 72:1052–1056. PMID: 20855066.

13. Itoi T, Sofuni A, Itokawa F, et al. Initial experience with a prototype peroral direct cholangioscope to perform intraductal lithotripsy (with video). Gastrointest Endosc. 2011; 73:841–843. PMID: 21067741.

14. Itoi T, Sofuni A, Itokawa F, et al. Free-hand direct insertion ability into a simulated ex vivo model using a prototype multibending peroral direct cholangioscope (with videos). Gastrointest Endosc. 2012; 76:454–457. PMID: 22078105.

15. Sethi A, Chen YK, Austin GL, et al. ERCP with cholangiopancreatoscopy may be associated with higher rates of complications than ERCP alone: a single-center experience. Gastrointest Endosc. 2011; 73:251–256. PMID: 21106195.

16. Efthymiou M, Raftopoulos S, Antonio Chirinos J, May GR. Air embolism complicated by left hemiparesis after direct cholangioscopy with an intraductal balloon anchoring system. Gastrointest Endosc. 2012; 75:221–223. PMID: 21470606.

17. Doi S, Yasuda I, Nakashima M, et al. Carbon dioxide insufflation vs. conventional saline irrigation for peroral video cholangioscopy. Endoscopy. 2011; 43:1070–1075. PMID: 21971925.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download