Abstract
Xanthogranulomatous inflammation (XGI) is a rare benign inflammatory disease characterized by aggregation of lipid-laden foamy macrophages. This disease entity has been described in various organs but most commonly in the kidney and gallbladder. The occurrence of this disease in the lower gastrointestinal tract is extremely rare. Its clinical importance is that it can be misdiagnosed as an infiltrative cancer. In this case report, a 52-year-old male complained of right lower quadrant abdominal pain for a period of 3 months. Abdominal computed tomography revealed appendiceal mass and colonoscopy revealed multiple erythematous nodular lesions in the terminal ileum and appendiceal orifice, mimicking appendiceal cancer. Right hemicolectomy was done and the pathological specimen revealed XGI of the terminal ileum. To our knowledge, this is the first case of XGI in terminal ileum presenting as abdominal pain and the appendiceal mass on radiologic findings.
Xanthogranulomatous inflammation (XGI) is a relatively rare chronic inflammatory process that is characterized by prominent histiocytic component with clusters of xanthoma-type cells.1 XGI can involve any organ, mainly occurring in the kidneys and gallbladder.2,3 Involvement of lower gastrointestinal (GI) tract has been rarely reported, but is confined to the appendix and colon.4 Especially, such lesion in the small bowel has never been reported. Also, it is generally difficult to differentiate XGI of GI involvement from infiltrative cancer because XGI may present as a focal mass-like lesion showing extension of fibrosis and inflammation to adjacent tissues.5 We firstly report a case of XGI in terminal ileum as an appendiceal mass.
A 52-year-old man visited our unit due to right lower quadrant abdominal pain for 3 months. His blood tests revealed a white blood cell count of 11,900 cells/µL with 82% neutrophils, hemoglobin of 12.8 g/dL, platelet count 389,000 cells/µL, C-reactive protein 7.53 mg/dL (range, 1.0 to 0.8), and carcinoembryonic antigen 4.0 ng/mL (range, 0 to 5.0). All other results were normal. Abdominal computed tomography (CT) demonstrated a 5-cm appendiceal mass with inhomogeneous enhancement, edematous bowel wall thickening of the terminal ileum, and multiple enlarged lymph nodes along the ileocolic mesentery (Fig. 1). Colonoscopy showed multiple erythematous nodular lesions in the terminal ileum and appendiceal orifice (Fig. 2). Multiple biopsies of these lesions were obtained, revealing ulcer with acute and chronic inflammation. However, radiological findings highly suggested appendiceal cancer, for which we decided to perform exploratory laparoscopy. A laparoscopy revealed a 5.5× 3 cm mass in the terminal ileum, and laparoscopic right hemicolectomy was performed. A macroscopic study showed a lobulated golden-yellowish mass-like lesion involving the ileal wall and adjacent mesentery. A brown-colored perpendicular lesion had the strong possibility of penetrating foreign material (Fig. 3). The colonic mucosa was relatively well-preserved, and the appendix was buried in an adjacent mass-like lesion without evidence of appendicitis. Microscopically, the mass-like lesion of the ileum showed nodular aggregation of lipid-laden foamy histiocytes and variable numbers of small lymphocytes, plasma cells, and eosinophils, which mainly involved the submucosa and muscle proper with extension into the mesenteric fat tissue (Fig. 4A). There were occasional foci of foreign body type giant cell reactions surrounding calcified food materials (Fig. 4B). These histological findings were compatible with XGI mainly involving the terminal ileum.
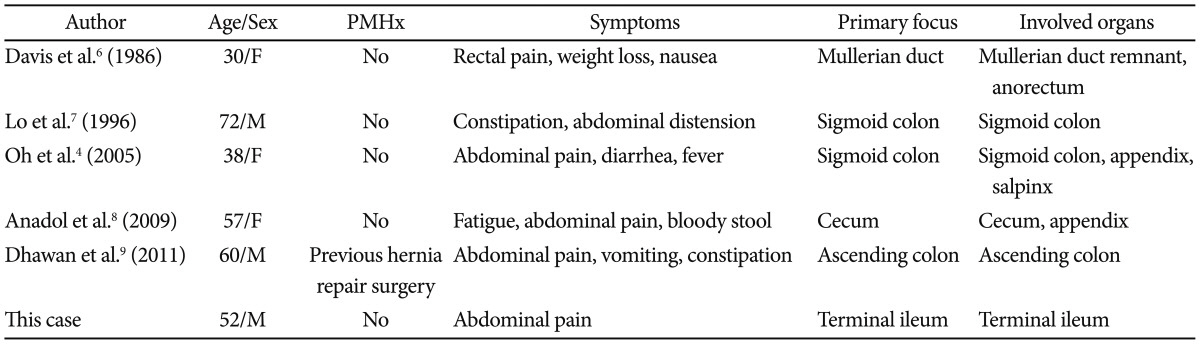
XGI is a rare chronic inflammatory disease characterized by a focal or diffuse destructive inflammatory process, with accumulation of lipid-laden fibrous tissue, and acute and chronic inflammatory cells.1 It may involve any organ, but the most common sites are known as the gallbladder and kidney.2,3 XGI involving lower GI tract is rare, but five cases of XGI involving the large bowel have been reported, which are summarized in Table 1 as compared with the present case.4,6-9 However, involvement of terminal ileum has not been reported. Clinically, it can be difficult to differentiate from infiltrative cancer because features of XGI are represented in the form of an irregular mass-like lesion with fibrosis and inflammation extending the surrounding tissue.5 Therefore, the appropriate surgical approach for pathologic diagnosis is needed.5 In the present case, noninvasive diagnostic process revealed that the appendiceal mass was consistent with invasive cancer, for which we performed laparoscopic exploration for definitive diagnosis and then confirmed XGI in terminal ileum.
Although the exact pathogenesis of XGI is not well established, several mechanisms have been suggested, including chronic recurrent infection, obstruction, immunologic disorders, and defective lipid transport.9 Unlike the obstructive hypothesis related to xanthogranulomatous cholecystitis, pyelonephritis, and appendicitis, XGI in the GI tract has the possibility of ongoing process in chronic suppurative inflammation with tissue destruction and localized proliferation of lipid rich macrophage.9 Interestingly, in our case, the cecum and appendix had no evidence of inflammation, but a brown-colored perpendicular lesion regarded as penetrated foreign material was observed on frozen specimen and microscope in terminal ileum. This may suggest that the mechanism of XGI is a prolonged inflammation associated with tissue damage and microscopic perforation caused by foreign material.
XGI of the lower GI tract has symptoms such as abdominal pain, fever, and mass-like lesion (Table 1). According to the histologic findings, bright yellow or golden yellow mass-like lesion was associated with abscess cavities, microabscesses, and lipid-rich macrophage.1 In the presence of soft tissue around the lesion, adjacent tissue is accompanied by severe infiltration, and the inflammatory mass is formed. Therefore, it can be difficult to differentiate from malignant tumors in radiologic findings.1 This case has symptoms of abdominal pain and mass, and the strong possibility of appendiceal malignancy. Preoperative endoscopic biopsy showed acute and chronic inflammation, which provided no information that can avoid surgical diagnosis. Laparoscopic right hemicolectomy was performed because there was a strong clinical suspicion of malignancy and the possibility of cancer could not be ruled out. The ileal wall and adjacent mesentery was involved by XGI, and the appendix with normal appearance was buried in mass-like lesion, probably misdiagnosed as appendiceal cancer on abdominal CT.
The diagnosis is usually confirmed by histological examination of the resected lesion. There is no existence in biochemical or hematological findings to help the diagnosis. Imaging studies, fine needle aspiration cytology, and clinical endoscopy may be suggestive, but no reports on their usefulness exist. Especially, fine needle aspiration and biopsy can lead to fistula formation and cannot exclude coexisting malignancy.10 Confirmatory diagnosis and definitive treatment of XGI are made only at surgery. Because of the inflammatory and invasive nature of XGI, a complete resection of adjacent adhesive tissues should be attempted. We performed an extensive resection involving the ascending colon and cecum.
This case is differentiated from others in that it suggests a possible pathogenesis of XGI. Until now, there has been no definitive evidence of pathogenesis of XGI among the reported cases involving the lower GI tract. In this case, food material, suspected to be a fish bone, in the terminal ileum seemed to have created a microscopic perforation, followed by foreign body giant cell reaction. Therefore, it can be presumed that XGI can develop due to recurrent inflammation by microperforation.
In summary, XGI of the lower GI tract is extremely rare and its pathogenesis is unknown. This report presents a possible hypothesis for the pathogenesis of XGI in the GI tract.
References
1. Cozzutto C, Carbone A. The xanthogranulomatous process. Xanthogranulomatous inflammation. Pathol Res Pract. 1988; 183:395–402. PMID: 3054826.
2. Franco V, Aragona F, Genova G, Florena AM, Stella M, Campesi G. Xanthogranulomatous cholecystitis. Histopathological study and classification. Pathol Res Pract. 1990; 186:383–390. PMID: 2377572.
3. Antonakopoulos GN, Chapple CR, Newman J, et al. Xanthogranulomatous pyelonephritis. A reappraisal and immunohistochemical study. Arch Pathol Lab Med. 1988; 112:275–281. PMID: 3345125.
4. Oh YH, Seong SS, Jang KS, et al. Xanthogranulomatous inflammation presenting as a submucosal mass of the sigmoid colon. Pathol Int. 2005; 55:440–444. PMID: 15982221.

5. Maeda T, Shimada M, Matsumata T, et al. Xanthogranulomatous cholecystitis masquerading as gallbladder carcinoma. Am J Gastroenterol. 1994; 89:628–630. PMID: 8147372.
6. Davis M, Whitley ME, Haque AK, Fenoglio-Preiser C, Waterman R. Xanthogranulomatous abscess of a mullerian duct remnant. A rare lesion of the rectum and anus. Dis Colon Rectum. 1986; 29:755–759. PMID: 3769695.
7. Lo CY, Lorentz TG, Poon CS. Xanthogranulomatous inflammation of the sigmoid colon: a case report. Aust N Z J Surg. 1996; 66:643–644. PMID: 8859170.
8. Anadol AZ, Gonul II, Tezel E. Xanthogranulomatous inflammation of the colon: a rare cause of cecal mass with bleeding. South Med J. 2009; 102:196–199. PMID: 19194269.
9. Dhawan S, Jain D, Kalhan SK. Xanthogranulomatous inflammation of ascending colon with mucosal involvement: report of a first case. J Crohns Colitis. 2011; 5:245–248. PMID: 21575889.

10. Krishnani N, Dhingra S, Kapoor S, Pandey R. Cytopathologic diagnosis of xanthogranulomatous cholecystitis and coexistent lesions. A prospective study of 31 cases. Acta Cytol. 2007; 51:37–41. PMID: 17328493.
Fig. 1
Computed tomography (CT) findings. Abdominal CT images showed an approximately 5-cm appendiceal mass.

Fig. 2
Endoscopic findings. Colonoscopy showed multiple erythematous nodular lesions in (A) the terminal ileum and (B) appendiceal orifice.
Fig. 3
Macroscopic findings. Cut section reveals (A) irregular golden-yellow mass-like lesion of the terminal ileum wall and mesentery (B) with a focus of mucosal lesion of the ileum.
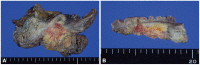
Fig. 4
Microscopic findings. Histologic findings of xanthogranulomatous inflammation showing (A) nodular aggregation of lipid-laden foamy histiocytes (H&E stain, ×400), and (B) foreign body giant cell reaction surrounding food material (H&E stain, ×400), and (C) calcified needle-shaped foreign material (H&E stain, ×400).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download