Abstract
Objective
To evaluate the reliability and validity of Korean version of AST (K-AST) as a bedside screening test of apraxia in patients with stroke for early and reliable detection.
Methods
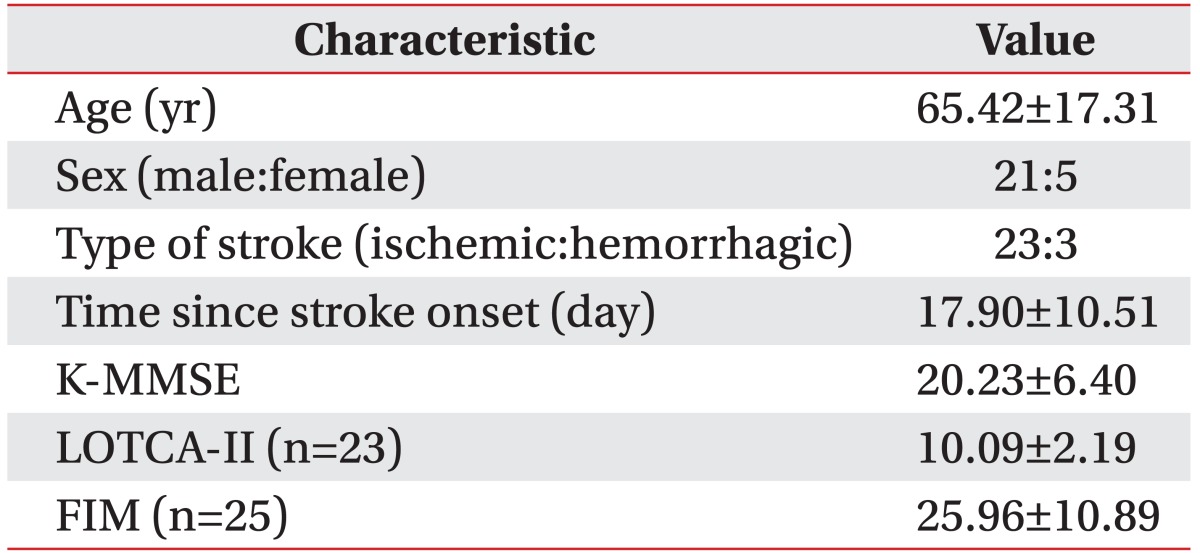
AST was translated into Korean, and the translated version received authorization from the author of AST. The performances of K-AST in 26 patients (21 males, 5 females; mean age 65.42±17.31 years) with stroke (23 ischemic, 3 hemorrhagic) were videotaped. To test the reliability and validity of K-AST, the recorded performances were assessed by two physiatrists and two occupational therapists twice at a 1-week interval. The patient performances at admission in Korean version of Mini-Mental State Examination (K-MMSE), self-care and transfer categories of Functional Independence Measure (FIM), and motor praxis area of Loewenstein Occupational Therapy Cognitive Assessment, the second edition (LOTCA-II) were also evaluated. Scores of motor praxis area of LOTCA-II was used to assess the validity of K-AST.
Results
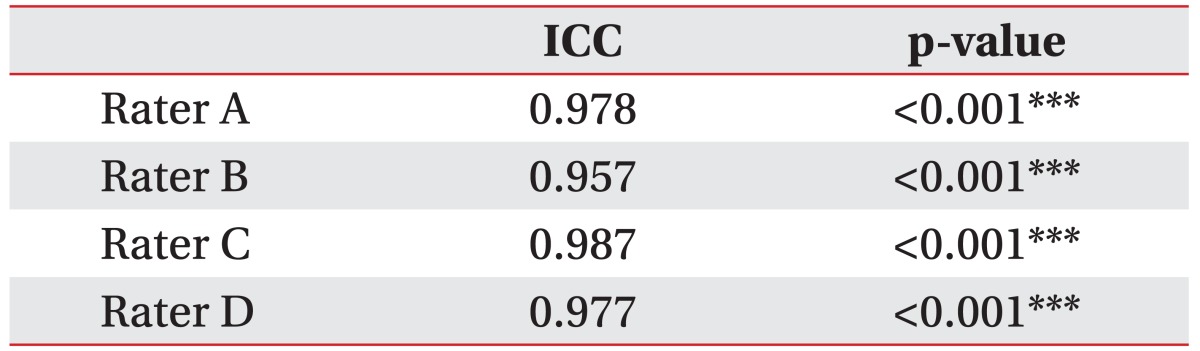
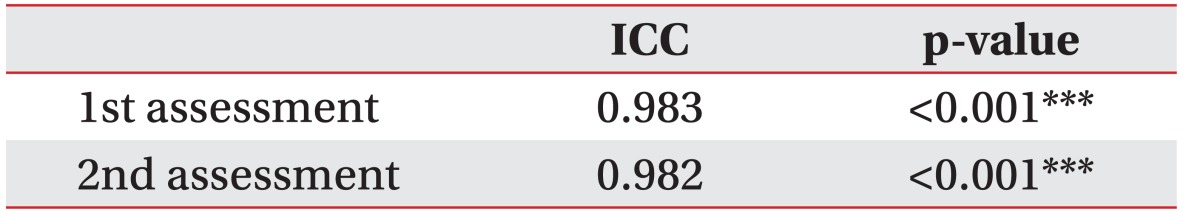
Inter-rater reliabilities were 0.983 (p<0.001) at the first assessment and 0.982 (p<0.001) at the second assessment. For intra-rater (test-retest) reliabilities, the values of four raters were 0.978 (p<0.001), 0.957 (p<0.001), 0.987 (p<0.001), and 0.977 (p<0.001). K-AST showed significant correlation (r=0.758, p<0.001) with motor praxis area of LOTCA-II test. K-AST also showed positive correlations with the total FIM score (r=0.694, p<0.001), the selfcare category of FIM (r=0.705, p<0.001) and the transfer category of FIM (r=653, p<0.001).
Apraxia is defined as the inability to correctly perform learned and/or skilled movements not attributable to primary motor and sensory impairments, or language comprehension difficulties [123]. Patients with apraxia know what to do, but not how, which manifests as specific spatial and temporal movement errors that interfere with efficient manipulation of objects [4]. Limb apraxia in patients with brain lesion(s) has considerable impact on activities of daily life and heralds a poorer outcome for independent living [5678]. Therefore, early and reliable detection of apraxia is important for evaluation of patients with brain injury.
Dovern et al. [9] reviewed assessment tools for diagnosis of apraxia in 2012. They found more than 20 assessments for upper limb apraxia having been published during the last four decades. However, many of these tests are not appropriate for clinical use, because some of them focus on only a single apraxic deficit, and some of them do not provide psychometric characteristics, and others are time-consuming. Because of these limitations, most of these assessments have not been widely used as a standard tool for assessment of upper limb apraxia.
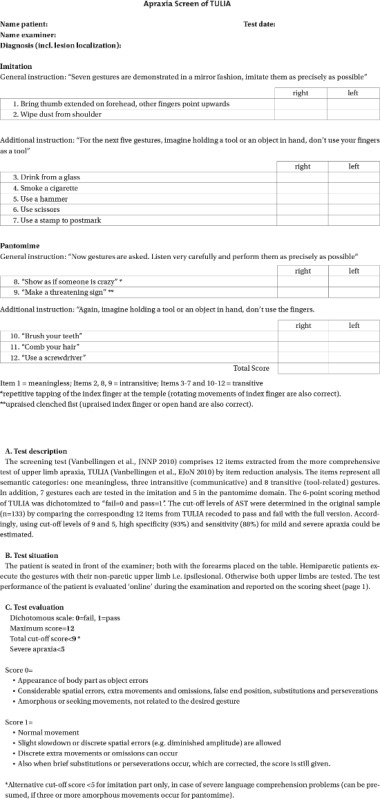
For clinical use, the assessment needs to provide quantifiable data and also assess all aspects of apraxia. In addition, the assessment should only take a short time to be used as a bedside screening for early detection. Among the assessments for, Apraxia Screen of TULIA (AST) constructed by Vanbellingen and his colleagues is regarded as an appropriate test for bedside screening of apraxia [9]. AST is based on a more comprehensive assessment of the same study group TULIA (Test for Upper-Limb Apraxia). TULIA consisted of 48 items, and it was designed not to be too time-consuming, but not designed to be used as a bedside assessment of apraxia. AST was constructed by reduction of TULIA to 12 items and also simplifying the scoring system [10] (see Appendix 1). The aim of this study was to evaluate the reliability and validity of the Korean version of AST (K-AST).
AST was translated into Korean (Version 1) by two physiatrists fluent in English. Another physiatrist reviewed the first version of the translation and then these three physiatrists discussed Version 1. A reconciled version (Version 2) was achieved by consensus and was back-translated into English by two other translators who majored in English literature (Version 3). Version 3 was reviewed and compared to the original version by two physiatrists.
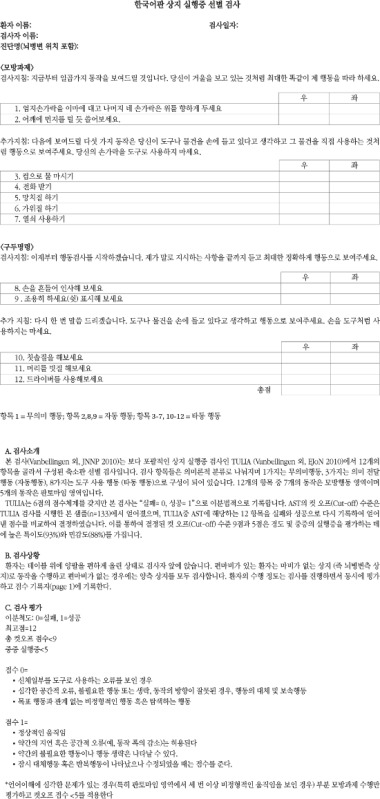
In Version 2, 4 of the 12 items of AST were modified because of the cultural differences. Three items (Items 4, 7 and 8) were substituted with other items in the same domain of TULIA. Item 4 ("smoke a cigarette") was changed to "pick up telephone". Item 7 ("use a stamp to postmark") was changed to "use a key" and Item 8 ("show me as if someone crazy") was changed to "wave goodbye." Item 9 ("make a threatening sign") was modified to "make a 'be quiet' sign," which was created by the translators considering the cultural background of respondents. The back-translated version (Version 3) was authorized by the author of AST. Version 2 was then used as Korean version of Apraxia of TULIA (K-AST) (see Appendix 2).
The subjects were 26 patients with stroke who were admitted or transferred to the rehabilitation unit of Konkuk University Medical Center from July 2013 to May 2014. The subjects were evaluated with K-AST at admission. Inclusion criteria were recent (<1 month) stroke and ability to perform at least a one-step obey command. Also, the motor power of at least one upper limb needed to be higher than a fair grade for the manual muscle test (MMT) on admission because fair and below fair motor grades could interfere with the AST task. Exclusion criteria were tetraplegia who could not move both sides of their body and limb pain that could affect movement of the limb. The subjects were also simultaneously assessed with Korean version of Mini-Mental State Examination (K-MMSE), self-care and transfer categories of Functional Independence Measure (FIM), and motor praxis area of Loewenstein Occupational Therapy Cognitive Assessment, the second edition (LOTCA-II).
Performances of K-AST for all 26 subjects were videotape-recorded. Two physiatrists and two occupational therapists assessed the videotaped performances twice at a 1-week interval to test the reliability and validity of the test. K-AST uses the same scoring system of AST, with a rating from 0 to 12, which is the summation of each item assessed by a pass (score 1) or a fail (score 0) grade. The same cut-off score for apraxia was used as in the original version. Same as the original version, the total cut-off score of <9 was used for K-AST, and the alternative cut-off score <5 for imitation part only was applied in case of severe language comprehension problems.
Patients were also evaluated with K-MMSE as cognition influences on performance of K-AST items. Self-care and transfer categories of FIM for the subjects were scored to assess independency in activities of daily life. Scores of motor praxis area of LOTCA-II was used to assess the validity of K-AST.
Statistical analyses were conducted using SPSS ver. 17.0 for Windows (SPSS Inc., Chicago, IL, USA). Intraclass correlation coefficient was used to analyze the intra-rater reliabilities and inter-rater reliabilities. Pearson correlation was used to evaluate the validity of K-AST.
Twenty-six subjects (21 males, 5 females) with stroke were evaluated. Table 1 summarizes their demographics and clinical characteristics. The mean age at assessment was 65.42±17.31 years. Most of the participants had ischemic stroke (n=23) with 3 having experienced hemorrhagic stroke. K-MMSE scores were obtained from all 26 patients (20.23±6.40), LOTCA-II scores were assessed from 23 patients (10.09±2.19), and FIM scores were obtained from 25 patients (25.96±10.89) on admission.
The intra-rater and inter-rater reliabilities of the K-AST was analyzed using intraclass correlation coefficient. The intra-rater (test-retest) reliabilities for the four raters were 0.978 (p<0.001), 0.957 (p<0.001), 0.987 (p<0.001), and 0.977 (p<0.001) (Table 2), which were all very high. The inter-rater reliabilities of the four raters were very high on both assessments; 0.983 (p<0.001) at the first assessment and 0.982 (p<0.001) at the second assessment (Table 3).
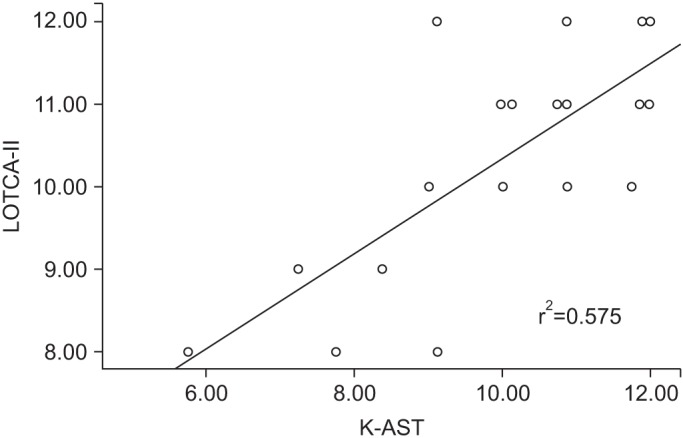
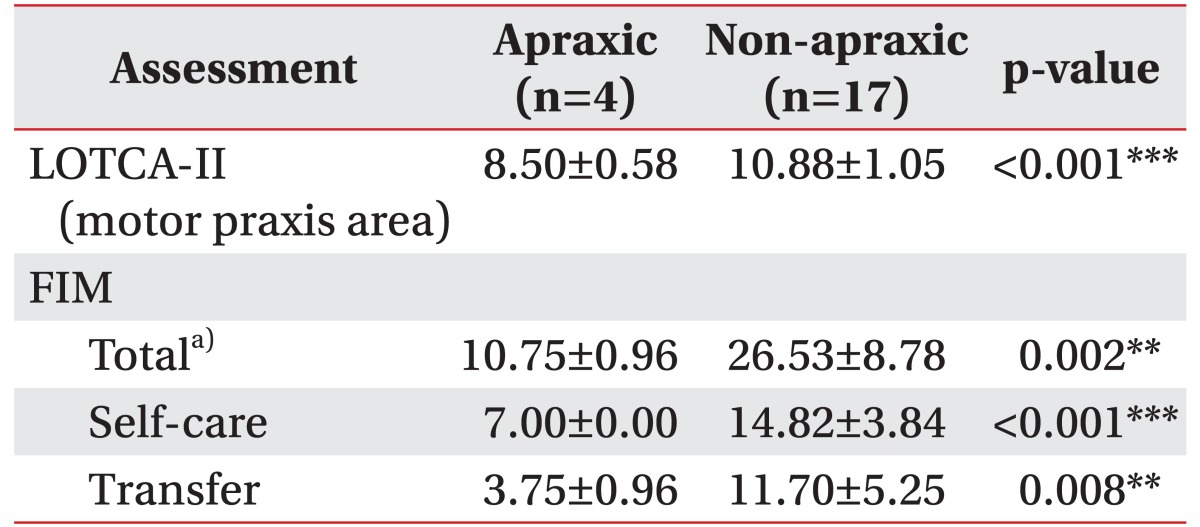
To assess the validity of K-AST, patients were grouped according to AST evaluation cut-off score into an apraxic group (K-AST score <9) and a non-apraxic group (K-AST score ≥9). Grouping assignment for apraxia was done among the subject (n=21) who had all scores for the three parts of the relevant tests (two categories of FIM, and motor praxis area of LOTCA-II). The scores of one patient with severe aphasia were excluded from this assignment. Score difference for LOTCA-II between the two groups was statistically significant (p<0.001). FIM scores between the two groups also showed significant difference (p<0.05) (Table 4). Also, K-AST showed significant positive correlation (r=0.758, p<0.001) (Fig. 1) with the motor praxis area of LOTCA-II. K-AST also showed positive correlations with total FIM score (r=0.694, p<0.001), self-care category of FIM (r=0.705, p<0.001) and transfer category of FIM (r=653, p<0.001).
Apraxia is increasingly recognized as a cognitive motor disorder of stroke with considerable impact on everyday life [567]. It is associated with poorer outcome for independent living [811] or returning to work [12]. However, until the development of TULIA in 2010, only a few standardized apraxia scales were available, and those did not cover all domains and semantic features of gesture production [1314]. TULIA was designed to be a comprehensive, but not a time-consuming test. However, it was still too long to be used as a bedside test [13]. Recognizing this limitation, AST based on TULIA was developed soon thereafter. The assessment time for AST for most patients is ≤2 minutes, making it suitable as a bedside test.
The aim of this study was to translate AST into Korean and validate it. To perform this goal, 26 stroke patients were assessed with K-AST. The original version of AST was developed in the West and had been verified in English [10]. The translated and modified version with adequate internal consistence was applied to Korean patients considering the language and cultural differences. Most of the sentences in the test were simply translated, while 4 items were modified based on context for the cultural differences. The modified version was also authorized by the author of AST. High intra-rater and interrater reliabilities of K-AST were evident and consistent with the original version, indicating the appropriateness in the Korean adaptation of the AST items.
Vanbellingen et al. validated AST with TULIA and reported a highly significant correlation between them [10]. The authors validated TULIA using the De Renzi test, but this scale has not been widely used for assessment of apraxia. We used the score of motor praxis area of LOTCA-II (the second edition of LOTCA) for validating K-AST as a further evaluation. This assessment tool identifies a broad range of cognitive dysfunctions in orientation, visual and spatial perception, motor praxis, visuomotor organization, and thinking operation [151617]. Among these six areas, the motor praxis area of LOTCA-II consists of three subsets (motor imitation, use of object, and symbolic action). Each subset is rated from 1 to 4 points for a total subset score of 12, and increasing score indicates better performances [16]. Presently, K-AST positively correlated with motor praxis of LOTCA-II, indicating the appropriateness of K-AST in evaluating apraxia.
Significant differences were evident between the apraxic and non-apraxic groups in the motor praxis scores of LOTCA-II, self-care and transfer categories of FIM, and the summation of the two categories of FIM. These findings support that the cut-off value of K-AST is appropriate for determining apraxia.
FIM is a widely used method for measuring the level of disability and indicates how much assistance is required for the individual to carry out activities of the daily living [18]. FIM is composed of 18 items, classified in 6 categories. The 18 items of FIM were designed to evaluate the degree of assistance in performing each item, with rating on a 7-point ordinal scale that ranges from total assistance (score 1) to complete independence (score 7). We selected self-care and transfer categories of FIM, which are related to limb movements. The scores of self-care and transfer categories showed significant differences, as predicted.
For the analysis of the apraxic and non-apraxic groups, we excluded one patient with severe aphasia because the different cut-off value was applied to patients with severe language comprehension problems. The original version of AST suggested a patient with language comprehension problems "can be presumed, if three or more amorphous movements occur for pantomime" [10]. For the patient with aphasia in our study who had Wernicke's aphasia, we applied cut-off score <5 for determining apraxia. Further analysis for aphasic subjects will require recruitment of a sufficient number of patients.
Among inclusion criteria, ability to perform at least a one-step obey command was used because AST consisted of basic task instructions. All patients included this study were able to perform more than partially two-step obey command tasks. Also, all the tasks did not require upper limb motor power against gravity with significant resistance. Thus, we used "at least higher than a fair grade for one upper limb" as an inclusion criterion. However, all the patients in this study had at least a good grade or higher in one upper limb.
In conclusion, the Korean version of AST displayed significant intra- and inter-rater reliabilities, and correlated significantly to the motor praxis area of LOTCA-II. K-AST showed significant differences for K-MMSE, the motor praxis area of LOTCA-II, and self-care and transfer items of FIM scores between apraxic and non-apraxic groups, based on cut-off value of AST. Therefore, K-AST can be useful as a bedside assessment for early detection of apraxia in Korean patients.
References
2. Heilman KM, Maher LM, Greenwald ML, Rothi LJ. Conceptual apraxia from lateralized lesions. Neurology. 1997; 49:457–464. PMID: 9270577.

3. De Renzi E, Motti F, Nichelli P. Imitating gestures: a quantitative approach to ideomotor apraxia. Arch Neurol. 1980; 37:6–10. PMID: 7350907.
4. Wu AJ, Burgard E, Radel J. Inpatient rehabilitation outcomes of patients with apraxia after stroke. Top Stroke Rehabil. 2014; 21:211–219. PMID: 24985388.

5. Buxbaum LJ, Haaland KY, Hallett M, Wheaton L, Heilman KM, Rodriguez A, et al. Treatment of limb apraxia: moving forward to improved action. Am J Phys Med Rehabil. 2008; 87:149–161. PMID: 18209511.
6. Hanna-Pladdy B, Heilman KM, Foundas AL. Ecological implications of ideomotor apraxia: evidence from physical activities of daily living. Neurology. 2003; 60:487–490. PMID: 12578932.
7. Sunderland A, Shinner C. Ideomotor apraxia and functional ability. Cortex. 2007; 43:359–367. PMID: 17533759.

8. Sundet K, Finset A, Reinvang I. Neuropsychological predictors in stroke rehabilitation. J Clin Exp Neuropsychol. 1988; 10:363–379. PMID: 3403700.

9. Dovern A, Fink GR, Weiss PH. Diagnosis and treatment of upper limb apraxia. J Neurol. 2012; 259:1269–1283. PMID: 22215235.

10. Vanbellingen T, Kersten B, Van de Winckel A, Bellion M, Baronti F, Muri R, et al. A new bedside test of gestures in stroke: the apraxia screen of TULIA (AST). J Neurol Neurosurg Psychiatry. 2011; 82:389–392. PMID: 20935324.

11. Wetter S, Poole JL, Haaland KY. Functional implications of ipsilesional motor deficits after unilateral stroke. Arch Phys Med Rehabil. 2005; 86:776–781. PMID: 15827931.

12. Saeki S, Hachisuka K. The association between stroke location and return to work after first stroke. J Stroke Cerebrovasc Dis. 2004; 13:160–163. PMID: 17903969.

13. Vanbellingen T, Kersten B, Van Hemelrijk B, Van de Winckel A, Bertschi M, Muri R, et al. Comprehensive assessment of gesture production: a new test of upper limb apraxia (TULIA). Eur J Neurol. 2010; 17:59–66. PMID: 19614961.

14. Zwinkels A, Geusgens C, van de Sande P, Van Heugten C. Assessment of apraxia: inter-rater reliability of a new apraxia test, association between apraxia and other cognitive deficits and prevalence of apraxia in a rehabilitation setting. Clin Rehabil. 2004; 18:819–827. PMID: 15573839.

15. Jang Y, Chern JS, Lin KC. Validity of the Loewenstein Occupational Therapy Cognitive Assessment in people with intellectual disabilities. Am J Occup Ther. 2009; 63:414–422. PMID: 19708470.

16. Itzkovich M, Elazar B, Averbuch S, Katz N. Loewenstein Occupational Therapy Cognitive Assessment (LOTCA) battery. 2nd ed. Pequannock: Maddak;2000.
17. Lund K, Oestergaard LG, Maribo T. Danish translation and adaptation of Loewenstein Occupational Therapy Cognitive Assessment 2nd edition (LOTCA-II). Scand J Occup Ther. 2013; 20:302–305. PMID: 23600885.

18. Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996; 77:1226–1232. PMID: 8976303.

Fig. 1
Correlation of K-AST with motor praxis area of LOTCA-II. The scatterplots show the positive correlation of K-AST with motor praxis area of LOTCA-II. The squared correlation coefficient (r2) is 0.575, which means that approximately 58% of the patient score for K-AST is directly accounted for by their motor praxis area of LOTCA-II score and vice versa. K-AST, Korean version of AST; LOTCA-II, Loewenstein Occupational Therapy Cognitive Assessment 2nd edition.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download