Abstract
Objective
To compare the motor recovery following transverse myelitis in pediatric patients with and without spinal cord atrophy.
Method
From January 1995 through December 2009, twenty children (8 boys and 12 girls with an onset at 5.7±3.8 years) that were diagnosed with transverse myelitis at a Children's Hospital in Korea, and undertaken an initial and follow-up spine magnetic resonance image (MRI) were included. Medical records and spine MRI scans were reviewed retrospectively. An initial MRI was taken 5.1±8.7 days after the onset. The interval between an initial and follow-up MRIs was 33.4±23.0 days. The motor recovery differences between subjects with and without spinal cord atrophy on follow-up MRIs were determined. Motor recovery was defined as the elevation of one or more grades of manual muscle tests of the Medical Research Council.
Results
Eight patients had developed spinal cord atrophies and 12 patients had not. Of the 8 patients with spinal cord atrophy, 7 showed no motor improvement. Among the 12 patients without atrophy, 11 had motor improvement. Spinal cord atrophy on follow-up MRIs were related to the risk of no motor improvement (odds ratio=77.0, 95% confidence interval [4.114-1441.049], p-value=0.001).
Acute transverse myelitis (ATM), an inflammatory demyelinating myelopathy, usually presents with lower limb weakness, back pain, and sphincter disturbances in childhood.1 The incidence of ATM is between 1 to 8 per million populations in one year.2,3 Magnetic resonance imaging (MRI) shows local enlargement and increased signal intensity of the spinal cord in a T2-weighted image in ATM patients. The outcome of ATM has been studied and reported as variable in small populations be variable.4,5 Several clinical features such as complete paraplegia, shorter time to maximal deficit, supraspinal symptoms were suggested as prognostic factors of unfavorable outcomes.4 In one case series, spinal cord atrophy appeared in a late MRI was suggested as one of prognostic factors of grave outcome in spinal cord injury and transverse myelitis.6 In other cases with persistent neurologic deficits, spinal cord atrophy was confirmed in an autopsy.7 Nevertheless, there have been only a few cases reports on spinal cord atrophy following ATM. An investigation into the relationship of spinal cord atrophy and motor improvements has not been performed. In this study, we aimed to compare the improvement in motor weakness following transverse myelitis in children who had shown and those who had not shown spinal cord atrophies in follow-up spine MRIs.
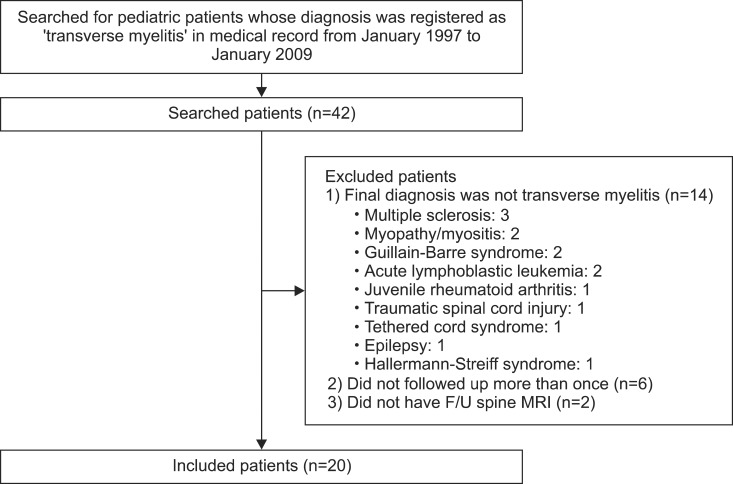
Patients diagnosed with transverse myelitis at one Children's Hospital (Seoul National University Children's Hospital, Seoul, South Korea) from January 1995 to January 2009 were investigated. Those who had initial and follow-up MRIs were included. Subjects were excluded when their final diagnosis was not transverse myelitis or they did not have a follow-up more than one time in our hospital. A flowchart of the subject inclusion criteria is illustrated in Fig. 1. Diagnostic criteria for the idiopathic ATM were used to discern idiopathic ATM (Table 1).8,9 Twenty patients with transverse myelitis had taken initial and late spine MRI scans (8 boys, age at diagnosis was 5.7±3.8 years). The initial MRI was taken 5.1±8.7 days after the onset. Interval between initial and follow-up MRIs was 33.4±23.0 days.
A Retrospective case-control study was performed. We reviewed medical records and spine MRI scans to find out whether clinical improvements in motor weakness had occurred and the spinal cord atrophies had developed on follow-up MRIs.
Spinal cord atrophy in the follow-up MRI was defined as: an abnormal thinning of the spinal cord in the sagittal plane in two segments or more beyond the limits of vertebral injury; or a reduction in the spinal cord area 50% or greater in more than two consecutive transverse planes. Spinal cord atrophy was confirmed by two board-certified radiologists. Atrophic changes were also measured in cross-sectional areas (CSA) using an image processing program, Marosis M-view 5.4 (Marotech Inc., Seoul, Korea) (Fig. 2). Improved motor power was defined as elevation of one or more grades in Medical Research Council (MRC) grades. If a child could not obey the physician's commands, his or her spontaneous movements were observed to assume degrees of motor power.
All twenty children had presented with sudden weakness that fulfilled the classic criteria for acute transverse myelitis. Initial spine MRIs showed high signal intensity lesions in T2-weighted images. The patients received steroid therapy and had their neurologic status before and after the therapy investigated (Table 2). The onset age was not different between children with and without spinal cord atrophy (p-value>0.05). The mean interval between the initial and late MRI was 33.4±23.0 days and also not significantly different between two groups (p-value>0.05).
Eight patients had developed and 12 patients had not developed spinal cord atrophies (an example is presented in Fig. 3). Among 8 patients with spinal cord atrophy, 7 showed no motor recovery. A decrease in the atrophied segment CSA as compared to the initial measurement was 43.0±18.1%. One patient who showed motor improvement despite spinal cord atrophy was a 19-month-old girl whose motor power of the lower extremities improved to MRC grade 3. She had a thinning spinal cord, but the decrement in CSA was 72.8% of the initial one. Among the 12 patients without atrophy, 11 had motor improvement except one (Table 3). There was a statistically significant difference in the chances of motor improvement between groups with and without spinal cord atrophy (odds ratio=77.0, 95% C.I. [4.114-1441.049], p-value=0.001).
This was the first study to investigate relationship between spinal cord atrophy and motor improvement in pediatric transverse myelitis. Of our subjects, 7 out of 20 (35.0%) had no motor power improvement. A poor recovery rate was in concordance with previous reports, also, previous reports noted 44% mild to severe sequelae.4,10 There have been several research studies on prognostic factors of transverse myelitis. An unfavorable outcome was associated with complete paraplegia and a shorter time to maximal deficit.4 However, there was no mention of MRI findings with outcomes. In another study, symptoms associated with poor outcome were back pain as an initial complaint, with a rapid progression to maximal symptoms within hours of onset, spinal shock, and sensory disturbance up to the cervical level.1 It is also known that the presence of 14-3-3 protein, a marker of neuronal injury, in the CSF during the acute phase may also predict a poor outcome.11
Known MRI findings of ATM were edema, single or multiple high signal intensity lesions on T2-weighted sequence and postgadolinium enhancement. Although changes in an MRI following the acute phase were not well known, there was an observation that in 2 out of 3 patients, a follow-up MRI showed a return to normal and the remaining patient had a persistent high signal intensity lesion after 4 months.4 Spinal cord atrophies were detected after 33.4±23.0 days following the initial MRI, and were associated with poor improvement in motor power. It may be an indicator for persistent neurologic impairment in children with acute transverse myelitis.
Due to the limitation as a retrospective study, and difficulty in measuring accurate motor power in children, motor improvement was only classified as good, which was defined as any motor power improvements, or poor. A second limitation is the MRC grade. It could be inappropriate for young children under age 4, because of the short attention span and potential lack of cooperation or understanding. A modified scale is recommended instead, in which grade 4 and 5 are put together as grade 4.12 This could not be used in this study, however, only one young child (patient 15, Table 2) was evaluated as MRC grade 5, and as having had meaneaful motor power improvement was defined as elevation of one or more grades, no difference in the results might happen even if the modified scale were applied. In other studies, the outcomes of transverse myelitis were estimated as good, fair and poor according to the sequelae of motor, sensory and autonomic signs.10
Activities of daily living (ADL) could not be evaluated in this study, because there had been no well-established evaluation tool for ADL in young children with myelopathy, which was validated in Korean.
Spinal cord atrophies can be measured in various ways, but only CSA of the spinal cord segments were used in our study to assume spinal cord atrophies. Atrophies could be better defined as reduction in volume rather than in area, as in recent attempts.13 In addition, visualizing structural connectivity might be more important than measuring only the CSA of the spinal cord. Diffusion tensor imaging (DTI) of the spinal cord is suggested as a useful tool to evaluate fiber connectivity14 and to predict outcome of traumatic spinal cord injury.15 DTI could be helpful in predicting the prognosis of ATM also, especially in patients who had motor improvement despite spinal cord atrophy. Authors tried to take DTI in a few cases recently, however, DTI of the thoracic spinal cord was hard to obtain due to adjacent cardiac activity.
The results of our study revealed that children with transverse myelitis who had developed spinal cord atrophies in late MRIs had a smaller motor recovery than those who had not. These findings suggest that the appearance of the spinal cord atrophy on MRI could be an indicator of poor prognosis in pediatric patients with transverse myelitis.
References
1. Dunne K, Hopkins IJ, Shield LK. Acute transverse myelopathy in childhood. Dev Med Child Neurol. 1986; 28:198–204. PMID: 3709989.

2. Berman M, Feldman S, Alter M, Zilber N, Kahana E. Acute transverse myelitis: incidence and etiologic considerations. Neurology. 1981; 31:966–971. PMID: 7196523.

3. Jeffery DR, Mandler RN, Davis LE. Transverse myelitis. Retrospective analysis of 33 cases, with differentiation of cases associated with multiple sclerosis and parainfectious events. Arch Neurol. 1993; 50:532–553. PMID: 8489410.
4. Defresne P, Hollenberg H, Husson B, Tabarki B, Landrieu P, Huault G, Tardieu M, Sebire G. Acute transverse myelitis in children: clinical course and prognostic factors. J Child Neurol. 2003; 18:401–406. PMID: 12886975.

5. Kalra V, Sharma S, Sahu J, Sankhyan N, Chaudhry R, Dhawan B, Mridula B. Childhood acute transverse myelitis: clinical profile, outcome, and association with antiganglioside antibodies. J Child Neurol. 2009; 24:466–471. PMID: 19196873.

6. Bang MS, Kim SJ. Progression of spinal cord atrophy by traumatic or inflammatory myelopathy in the pediatric patients: case series. Spinal Cord. 2009; 47:822–825. PMID: 19172153.

7. Awerbuch G, Feinberg WM, Ferry P, Komar NN, Clements J. Demonstration of acute post-viral myelitis with magnetic resonance imaging. Pediatr Neurol. 1987; 3:367–369. PMID: 2853946.

8. Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002; 59:499–505. PMID: 12236201.
9. Bruna J, Martinez-Yelamos S, Martinez-Yelamos A, Rubio F, Arbizu T. Idiopathic acute transverse myelitis: a clinical study and prognostic markers in 45 cases. Mult Scler. 2006; 12:169–173. PMID: 16629419.
10. Knebusch M, Strassburg HM, Reiners K. Acute transverse myelitis in childhood: nine cases and review of the literature. Dev Med Child Neurol. 1998; 40:631–639. PMID: 9766742.

11. Irani DN, Kerr DA. 14-3-3 protein in the cerebrospinal fluid of patients with acute transverse myelitis. Lancet. 2000; 355:901. PMID: 10752712.

12. Braddom RL, Chan L, Harrast MA, Kowalske KJ, Matthews DJ, Ragnarsson KT, Stolp KA. Physical medicine and rehabilitation. 2011. 4th ed. Philadelphia: Elsevier Sounders;p. 47.
13. Coulon O, Hickman SJ, Parker GJ, Barker GJ, Miller DH, Arridge SR. Quantification of spinal cord atrophy from magnetic resonance images via a B-spline active surface model. Magn Reson Med. 2002; 47:1176–1185. PMID: 12111964.

14. Wheeler-Kingshott CA, Hickman SJ, Parker GJ, Ciccarelli O, Symms MR, Miller DH, Barker GJ. Investigating cervical spinal cord structure using axial diffusion tensor imaging. Neuroimage. 2002; 16:93–102. PMID: 11969321.

15. Kim JH, Loy DN, Wang Q, Budde MD, Schmidt RE, Trinkaus K, Song SK. Diffusion tensor imaging at 3 hours after traumatic spinal cord injury predicts long-term locomotor recovery. J Neurotrauma. 2010; 27:587–598. PMID: 20001686.

Fig. 2
A, B, and C denotes the level of each cross-sectional view. Cross-sectional areas in atrophied spinal cord segments were measured using Marosis M-view 5.4.
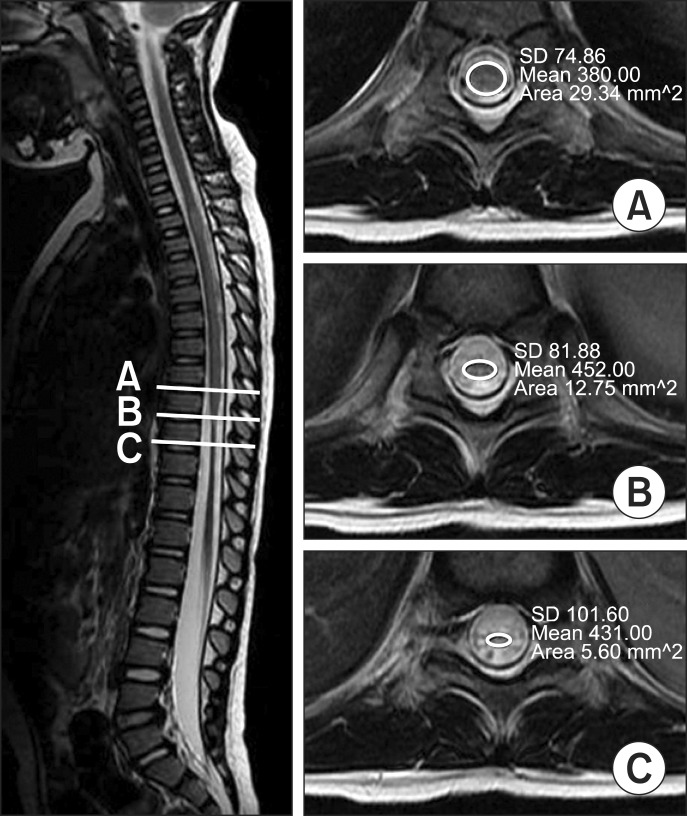
Fig. 3
A T2-weighted sagittal view of the whole spine MRI of the patient (a 4 year-old girl) diagnosed as transverse myelitis (A) There was diffuse cord swelling below T5 level and (B) a spinal cord atrophy was detected with residual swelling in MRI taken 20 days after the initial one.

Table 1
Transverse Myelitis Consortium Working Group Criteria for Idiopathic Acute Transverse Myelitis





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download