1. Lee SW, Yang JM, Moon SY, Yoo IK, Ha EK, Kim SY, et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020; 7(12):1025–1031. PMID:
32950066.

2. Kim MS, Jung SY, Lee SW, Li H, Koyanagi A, Kronbichler A, et al. Hepatobiliary adverse drug reactions associated with remdesivir: the WHO international pharmacovigilance study. Clin Gastroenterol Hepatol. 2021; 19(9):1970–1972.e3. PMID:
33940227.

3. Saviano A, Wrensch F, Ghany MG, Baumert TF. Liver disease and coronavirus disease 2019: from pathogenesis to clinical care. Hepatology. 2021; 74(2):1088–1100. PMID:
33332624.

4. Iavarone M, D'Ambrosio R, Soria A, Triolo M, Pugliese N, Del Poggio P, et al. High rates of 30-day mortality in patients with cirrhosis and COVID-19. J Hepatol. 2020; 73(5):1063–1071. PMID:
32526252.

5. Meijnikman AS, Bruin S, Groen AK, Nieuwdorp M, Herrema H. Increased expression of key SARS-CoV-2 entry points in multiple tissues in individuals with NAFLD. J Hepatol. 2021; 74(3):748–749. PMID:
33338513.

6. Singh S, Khan A. Clinical characteristics and outcomes of coronavirus disease 2019 among patients with preexisting liver disease in the United States: a multicenter research network study. Gastroenterology. 2020; 159(2):768–771.e3. PMID:
32376408.

7. Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol. 2019; 71(4):793–801. PMID:
31279902.

8. Shin YH, Shin JI, Moon SY, Jin HY, Kim SY, Yang JM, et al. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol. 2021; 3(10):e698–e706. PMID:
34179832.

9. Lagana SM, Kudose S, Iuga AC, Lee MJ, Fazlollahi L, Remotti HE, et al. Hepatic pathology in patients dying of COVID-19: a series of 40 cases including clinical, histologic, and virologic data. Mod Pathol. 2020; 33(11):2147–2155. PMID:
32792598.

10. Lazarus JV, Colombo M, Cortez-Pinto H, Huang TT, Miller V, Ninburg M, et al. NAFLD - sounding the alarm on a silent epidemic. Nat Rev Gastroenterol Hepatol. 2020; 17(7):377–379. PMID:
32514153.

11. Woo A, Lee SW, Koh HY, Kim MA, Han MY, Yon DK. Incidence of cancer after asthma development: 2 independent population-based cohort studies. J Allergy Clin Immunol. 2021; 147(1):135–143. PMID:
32417133.

12. Lee SW, Lee J, Moon SY, Jin HY, Yang JM, Ogino S, et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. Forthcoming. 2021; DOI:
10.1136/bjsports-2021-104203.

13. Lee SW, Yang JM, Moon SY, Kim N, Ahn YM, Kim JM, et al. Association between mental illness and COVID-19 in South Korea: a post-hoc analysis. Lancet Psychiatry. 2021; 8(4):271–272. PMID:
33617761.

14. Yang JM, Koh HY, Moon SY, Yoo IK, Ha EK, You S, et al. Allergic disorders and susceptibility to and severity of COVID-19: a nationwide cohort study. J Allergy Clin Immunol. 2020; 146(4):790–798. PMID:
32810517.
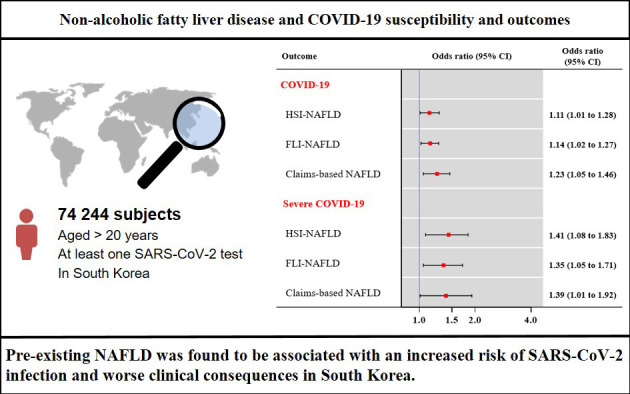
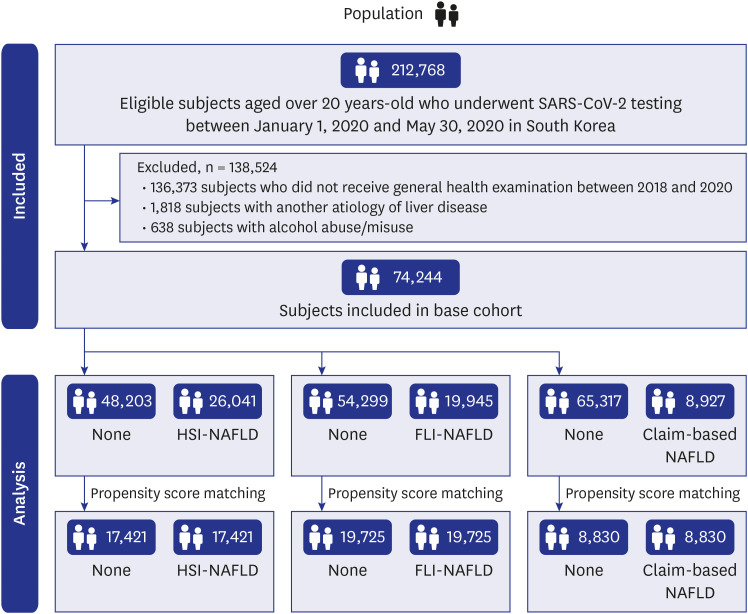
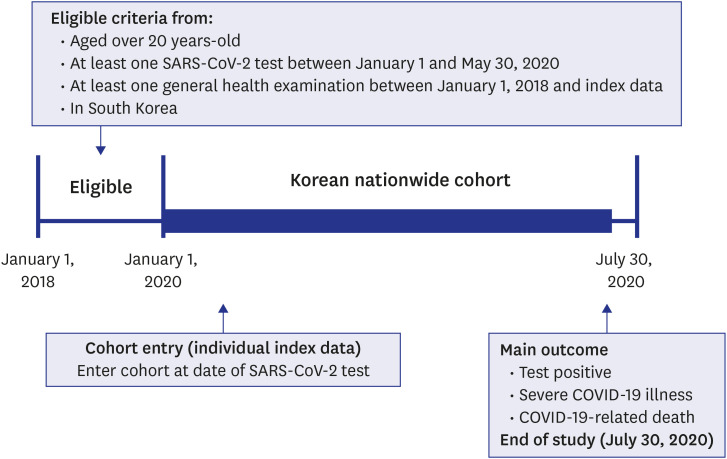
15. Yoo HW, Shin JI, Yon DK, Lee SW. COVID-19 morbidity and severity in patients with nonalcoholic fatty liver disease in South Korea: a nationwide cohort study. Clin Gastroenterol Hepatol. Forthcoming. 2021; DOI:
10.1016/j.cgh.2021.07.031.

16. Lee SW, Ha EK, Yeniova AÖ, Moon SY, Kim SY, Koh HY, et al. Severe clinical outcomes of COVID-19 associated with proton pump inhibitors: a nationwide cohort study with propensity score matching. Gut. 2021; 70(1):76–84. PMID:
32732368.

17. Ha J, Lee SW, Yon DK. Ten-year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017. Clin Exp Pediatr. 2020; 63(7):278–283. PMID:
32023407.

18. Lee SW, Kim SY, Moon SY, Yang JM, Ha EK, Jee HM, et al. Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: a Korean nationwide cohort study. J Allergy Clin Immunol Pract. 2021; 9(6):2262–2271.e2. PMID:
33931377.

19. Boursier J, Shreay S, Fabron C, Torreton E, Fraysse J. Hospitalization costs and risk of mortality in adults with nonalcoholic steatohepatitis: analysis of a French national hospital database. EClinicalMedicine. 2020; 25:100445. PMID:
32775971.

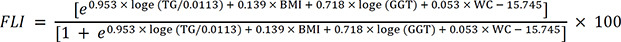
20. Chen LD, Huang JF, Chen QS, Lin GF, Zeng HX, Lin XF, et al. Validation of fatty liver index and hepatic steatosis index for screening of non-alcoholic fatty liver disease in adults with obstructive sleep apnea hypopnea syndrome. Chin Med J (Engl). 2019; 132(22):2670–2676. PMID:
31765354.

21. Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008; 57(10):1441–1447. PMID:
18390575.

22. Lee SW, Yang JM, Yoo IK, Moon SY, Ha EK, Yeniova AÖ, et al. Proton pump inhibitors and the risk of severe COVID-19: a post-hoc analysis from the Korean nationwide cohort. Gut. 2021; 70(10):2013–2015. PMID:
33303566.

23. Mushtaq K, Khan MU, Iqbal F, Alsoub DH, Chaudhry HS, Ata F, et al. NAFLD is a predictor of liver injury in COVID-19 hospitalized patients but not of mortality, disease severity on the presentation or progression - The debate continues. J Hepatol. 2021; 74(2):482–484. PMID:
33223215.

24. Sachdeva S, Khandait H, Kopel J, Aloysius MM, Desai R, Goyal H. NAFLD and COVID-19: a pooled analysis. SN Compr Clin Med. 2020; 1–4.

25. Forlano R, Mullish BH, Mukherjee SK, Nathwani R, Harlow C, Crook P, et al. In-hospital mortality is associated with inflammatory response in NAFLD patients admitted for COVID-19. PLoS One. 2020; 15(10):e0240400. PMID:
33031439.

26. Huang R, Zhu L, Wang J, Xue L, Liu L, Yan X, et al. Clinical features of COVID-19 patients with non-alcoholic fatty liver disease. Hepatol Commun. 2020; 4(12):1758–1768.
27. Campos-Murguía A, Román-Calleja BM, Toledo-Coronado IV, González-Regueiro JA, Solís-Ortega AA, Kúsulas-Delint D, et al. Liver fibrosis in patients with metabolic associated fatty liver disease is a risk factor for adverse outcomes in COVID-19. Dig Liver Dis. 2021; 53(5):525–533. PMID:
33551355.

28. Targher G, Mantovani A, Byrne CD, Wang XB, Yan HD, Sun QF, et al. Detrimental effects of metabolic dysfunction-associated fatty liver disease and increased neutrophil-to-lymphocyte ratio on severity of COVID-19. Diabetes Metab. 2020; 46(6):505–507. PMID:
32505652.

29. Sohrabi Y, Reinecke H, Godfrey R. Altered cholesterol and lipid synthesis mediates hyperinflammation in COVID-19. Trends Endocrinol Metab. 2021; 32(3):132–134. PMID:
33455862.

30. Nardo AD, Schneeweiss-Gleixner M, Bakail M, Dixon ED, Lax SF, Trauner M. Pathophysiological mechanisms of liver injury in COVID-19. Liver Int. 2021; 41(1):20–32. PMID:
33190346.

31. Kukla M, Skonieczna-Żydecka K, Kotfis K, Maciejewska D, Łoniewski I, Lara LF, et al. COVID-19, MERS and SARS with concomitant liver injury-systematic review of the existing literature. J Clin Med. 2020; 9(5):1420.

32. Foschi FG, Conti F, Domenicali M, Giacomoni P, Borghi A, Bevilacqua V, et al. External validation of surrogate indices of fatty liver in the general population: the Bagnacavallo Study. J Clin Med. 2021; 10(3):520. PMID:
33535679.

33. Gianfrancesco MA, Robinson PC. Changing COVID-19 outcomes in patients with rheumatic disease-are we really getting better at this? Lancet Rheumatol. 2021; 3(2):e88–e90. PMID:
33655223.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download