With interest we read the article by Youn et al.1 about a 22 years old male who developed fever and headache three days after having been vaccinated with the first jab of an mRNA-based severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) vaccine (Pfizer). Clinical neurologic exam only revealed mild nuchal rigidity but multimodal magnetic resonance imaging (MRI) showed a cytotoxic lesion in the splenium of the corpus callosum.1 The patient was discharged after two days without therapy and the clinical presentation had not changed at a follow-up one week after discharge.1 The study is appealing but raises the following comments and concerns.
A limitation is that no follow up MRIs were provided. Assuming that the corpus callosum lesion was ischemic in nature, the hypointensity on apparent diffusion coefficient (ADC) maps, as shown in Fig. 1, will turn into a hyperintensity after about 8 hours from the event. The hyperintensity on diffusion weighted imaging (DWI) will turn into an isointensity after a few days. T2-weighted or fluid attenuation inversion recovery (FLAIR) images will show the lesion as hyperintensity after a few hours.
Missing is the exclusion of a venous sinus thrombosis (VST), which is increasingly recognised as a complication of SARS-CoV-2 vaccinations.2 VST can manifest with headache, nuchal rigidity, and with ischemic stroke, all being present in the index case. We should know if the patient was a smoker and if the D-dimer was elevated on admission. Additionally, we should know the results of magnetic resonance venography (MRV).
Missing is the presentation of cerebral arteries on magnetic resonance angiography (MRA). Despite the young age the patient can theoretically have macro- or micro-angiopathy, which could be responsible for the ischemic callosal lesion. We should know if the family history was positive for stroke and if the index patient carried any classical cardiovascular risk factors (smoking, hyperlipidemia, diabetes, arterial hypertension, atrial fibrillation, coagulation disorder).
Since SARS-CoV-2 vaccinations can be also complicated by myocarditis3 and since myocarditis can be complicated by cardio-embolism, we should know the results of echocardiography or cardiac MRI with contrast medium. Did the patient ever complain about anginal chest pain and was the troponin level ever elevated?
To exclude acute, disseminated encephalomyelitis (ADEM) as a differential of the callosal lesion, application of contrast medium is missing. Usually, ADEM lesions show up with gadolinium enhancement.4 Additionally, MRI of the spinal cord should have been carried out to confirm or exclude a spinal lesion. Furthermore, follow-up MRI after treatment with steroids, is required to document the resolution of the abnormality.
Missing are the serum and cerebro-spinal fluid (CSF) levels of cytokines, such as IL-8, IL-6, IL-1A, and TNF-alpha.
Overall, the elegant study has some limitations which challenge the results and their interpretation. These limitations should be addressed to further strengthen the conclusions.
References
1. Youn T, Yang H. Cytotoxic lesion of the corpus callosum (CLOCCs) after SARS-CoV-2 mRNA vaccination. J Korean Med Sci. 2021; 36(31):e228. PMID: 34402238.

2. Shazley O, Alshazley M. A COVID-Positive 52-year-old man presented with venous thromboembolism and disseminated intravascular coagulation following Johnson & Johnson vaccination: a case-study. Cureus. 2021; 13(7):e16383. PMID: 34408937.
3. Khogali F, Abdelrahman R. Unusual presentation of acute perimyocarditis following SARS-COV-2 mRNA-1237 Moderna vaccination. Cureus. 2021; 13(7):e16590. PMID: 34447639.

4. Liu JG, Qiao WY, Dong QW, Zhang HL, Zheng KH, Qian HR, et al. [Clinical features and neuroimaging findings of 12 patients with acute disseminated encephalomyelitis involved in corpus callosum]. Zhonghua Yi Xue Za Zhi. 2012; 92(43):3036–3041. PMID: 23328373.
To the editor:
To begin with, we would like to appreciate the authors of the letter to the editor regarding our previous article, cytotoxic lesion of the corpus callosum (CLOCCs) after mRNA vaccination, for constructive criticism. In line with current JKMS guidelines of “Image in This Issue”, we focused on reporting typical MRI images of CLOCCs in our previous report. However, it seems that some were unconvinced of our conclusion, resulting from a lack of some patient information and follow-up data. Therefore, we would like to report follow-up MRI images and additional laboratory information of the patient.
First, the diagnosis of CLOCCs can be made based on imaging and clinical findings, and not necessarily on a diagnosis of exclusion. With the widespread use of MRI, many cases of various conditions of CLOCCs have been reported. According to Jay Starkey et al.,1 CLOCCs shows typical imaging findings such as a small round or oval shape lesion located in the center of the splenium. As mentioned in prior studies, ischemic infarction and acute disseminated encephalomyelitis (ADEM) of the corpus callosum tend to be asymmetric and more aggressive. Increasing evidence suggests that CLOCC has distinctive MRI findings compared to both ischemic stroke and ADEM. The patient's diagnosis was made based on common and typical findings of CLOCCs.
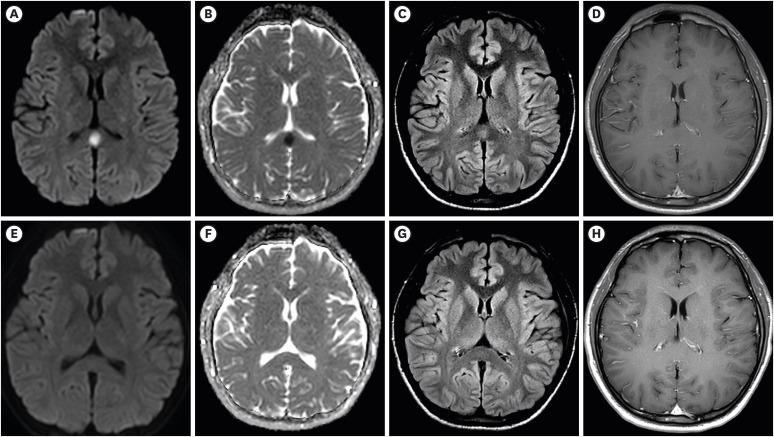
Due to the nature of cytotoxic edema, the MRI findings could be interpreted as an ischemic lesion of the corpus callosum. However, cytotoxic edema is not only seen in cerebral ischemia but also inflammatory conditions associated with a brain infection, encephalitis, metabolic abnormality, brain tumor, seizure, trauma, hemorrhage, vaccination, and COVID-19.234 In addition, CLOCCs is not always reversible, which implies that follow-up MRI might be unnecessary to confirm the diagnosis.5 As mentioned previously, the patient's initial MRI showed a lack of enhancement on the lesion (Fig. 1A-D).
In our prior report, the patient was a healthy young man without any underlying diseases, thus no notable risk factors for ischemia and there were no abnormal findings on neurological examination. This was another clinical clue that suggested against ischemic stroke. Ischemic stroke of the corpus callosum has more distinguishing clinical symptoms including cognitive impairment, complete or incomplete motor aphasia, language disorder, facial and limb paralysis, and alien hand syndrome.67 The patient's initial magnetic resonance angiography scan also showed no notable abnormality.
Second, in all likelihood, it is credible that CLOCCs could be secondary to cerebral venous thrombosis (CVT), which also has distinguishable findings such as clot signs and vasogenic and cytotoxic edema around the lesion, all not found in our index case.89 On the contrary, in our case, it is important to point out that the patient's initial D-dimer level was < 0.1 mg/L, which is known to carefully screen CVT with Vaccine-induced immune thrombocytopenia and thrombosis (VITT).10 Furthermore, we are rather reluctant to fully agree on the notion that the mRNA vaccination is a risk factor for CVT.11 VITT tends to appear after recombinant adenovirus vaccination rather than mRNA vaccine.12 The patient's initial cardiac enzyme levels (CK-MB, Tn-I, pro-BNP) were not elevated and there were no chest pains or other symptoms suggestive of myocarditis.
Third, we appreciate your generous suggestions to perform advanced diagnostic modalities including echocardiography, cardiac MRI, whole spine MRI, and cerebrospinal fluid cytokine test. Since the patient's headache completely resolved within a day of being admitted to a tertiary hospital, further imaging and laboratory examinations were not performed during admission. The purpose of this study was to suggest the possible need for further evaluation including an MRI scan of a healthy individual presenting with fever and headache after COVID-19 mRNA vaccination to identify adverse reactions. The World Health Organization's definition of adverse reaction is a response to a drug that is noxious, unintended, and which occurs at doses normally used in man for the prophylaxis, diagnosis, or therapy of disease, or the modifications of physiological function.13
We are grateful for the opportunity to report follow-up images that show resolution of previous lesions and no significant abnormalities after 3 months from the index event (Fig. 1E-H). Unfortunately, pressed for time, our previous paper was published without relevant follow-up MRI images but we hope that the images included in this report would be sufficient in supporting our last conclusion.
References
1. Starkey J, Kobayashi N, Numaguchi Y, Moritani T. Cytotoxic lesions of the corpus callosum that show restricted diffusion: mechanisms, causes, and manifestations. Radiographics. 2017; 37(2):562–576. PMID: 28165876.

2. Lin J, Lawson EC, Verma S, Peterson RB, Sidhu R. Cytotoxic lesion of the corpus callosum in an adolescent with multisystem inflammatory syndrome and SARS-CoV-2 infection. AJNR Am J Neuroradiol. 2020; 41(11):2017–2019. PMID: 32819898.

3. Moritani T, Smoker WR, Sato Y, Numaguchi Y, Westesson PL. Diffusion-weighted imaging of acute excitotoxic brain injury. AJNR Am J Neuroradiol. 2005; 26(2):216–228. PMID: 15709116.
4. Rasmussen C, Niculescu I, Patel S, Krishnan A. COVID-19 and involvement of the corpus callosum: potential effect of the cytokine storm? AJNR Am J Neuroradiol. 2020; 41(9):1625–1628. PMID: 32732269.

5. Tetsuka S. Reversible lesion in the splenium of the corpus callosum. Brain Behav. 2019; 9(11):e01440. PMID: 31588684.

6. Sun TK, Chen YY, Huang SH, Hsu SW, Lee CC, Chang WN, et al. Neurotoxicity of carbon monoxide targets caudate-mediated dopaminergic system. Neurotoxicology. 2018; 65:272–279. PMID: 29173994.

7. Yang LL, Huang YN, Cui ZT. Clinical features of acute corpus callosum infarction patients. Int J Clin Exp Pathol. 2014; 7(8):5160–5164. PMID: 25197390.
8. Liu J, Liu D, Yang B, Yan J, Pu Y, Zhang J, et al. Reversible splenial lesion syndrome (RESLES) coinciding with cerebral venous thrombosis: a report of two cases. Ther Adv Neurol Disord. 2017; 10(12):375–379. PMID: 29204189.

9. Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006; 26(Suppl 1):S19–S41. discussion S42-3. PMID: 17050515.

10. Makris M, Pavord S, Lester W, Scully M, Hunt B. Vaccine-induced immune thrombocytopenia and thrombosis (VITT). Res Pract Thromb Haemost. 2021; 5(5):e12529. PMID: 34136745.

11. Sharifian-Dorche M, Bahmanyar M, Sharifian-Dorche A, Mohammadi P, Nomovi M, Mowla A. Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis post COVID-19 vaccination; a systematic review. J Neurol Sci. 2021; 428:117607. PMID: 34365148.

12. Franchini M, Liumbruno GM, Pezzo M. COVID-19 vaccine-associated immune thrombosis and thrombocytopenia (VITT): diagnostic and therapeutic recommendations for a new syndrome. Eur J Haematol. 2021; 107(2):173–180. PMID: 33987882.

13. International drug monitoring: the role of national centres. Report of a WHO meeting. World Health Organ Tech Rep Ser. 1972; 498:1–25. PMID: 4625548.
Fig. 1
Brain MRI showed a cytotoxic lesion of the corpus callosum (CLOCCs) after the first dose of mRNA vaccination (BNT162b). (A-B) Diffusion and ADC map showed a small oval-shaped restricted lesion of corpus callosal splenium. (C) Fluid-attenuated inversion- recovery (FLARE) image showed high signal intensity on the same lesion. (D) A lack of enhancement on T1 contrast-enhanced image (T1CE). (E-H) After 3 months, follow-up images of the same patient showed the resolution of previous lesions and no significant abnormalities without T1CE enhancement. The patient refused to receive the second dose of the mRNA vaccine.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download