1. Kim HK, Lee SD. Pathophysiology of chronic obstructive pulmonary disease. Tuberc Respir Dis (Seoul). 2005; 59(1):5–13.

2. Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, Held LS, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006; 27(2):397–412. PMID:
16452599.

3. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006; 3(11):e442. PMID:
17132052.

4. Kim C, Kim Y, Yang DW, Rhee CK, Kim SK, Hwang YI, et al. Direct and indirect costs of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis (Seoul). 2019; 82(1):27–34. PMID:
30302958.

5. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380(9859):2163–2196. PMID:
23245607.
6. Abubakar I, Tillmann T, Banerjee A. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015; 385(9963):117–171. PMID:
25530442.
7. Cazzola M, MacNee W, Martinez FJ, Rabe KF, Franciosi LG, Barnes PJ, et al. Outcomes for COPD pharmacological trials: from lung function to biomarkers. Eur Respir J. 2008; 31(2):416–469. PMID:
18238951.

8. Morrow DA, de Lemos JA. Benchmarks for the assessment of novel cardiovascular biomarkers. Circulation. 2007; 115(8):949–952. PMID:
17325253.

9. Singh D. Blood eosinophil counts in chronic obstructive pulmonary disease: a biomarker of inhaled corticosteroid effects. Tuberc Respir Dis (Seoul). 2020; 83(3):185–194. PMID:
32578413.

10. Sin DD. Chronic obstructive pulmonary disease: reactive past, preventive future. Proc Am Thorac Soc. 2009; 6(6):523–523.

11. Mikolov T, Chen K, Corrado G, Dean J. Efficient estimation of word representations in vector space. arXiv. 2013.
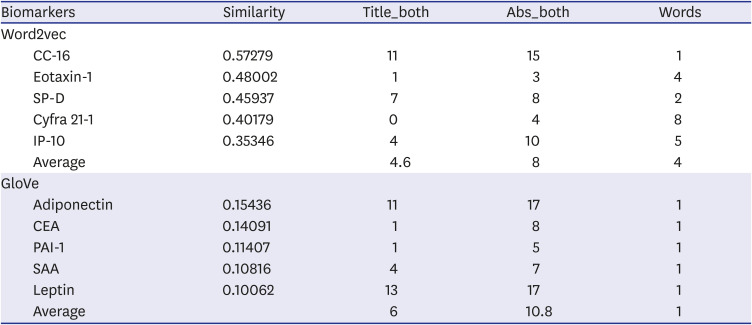
12. Yoon BH, Kim YS. Correlation analysis of chronic obstructive pulmonary disease (COPD) and its biomarkers using the word embeddings. In : Proceedings of the Eighth International Joint Conference on Natural Language Processing (Volume 2: Short Papers); Taipei, Taiwan; IJCNLP. 2017. p. 337–342.
13. Hahm CR, Lim MN, Kim HY, Hong SH, Han SS, Lee SJ, et al. Implications of the pulmonary artery to ascending aortic ratio in patients with relatively mild chronic obstructive pulmonary disease. J Thorac Dis. 2016; 8(7):1524–1531. PMID:
27499939.

14. Koo HK, Hong Y, Lim MN, Yim JJ, Kim WJ. Relationship between plasma matrix metalloproteinase levels, pulmonary function, bronchodilator response, and emphysema severity. Int J Chron Obstruct Pulmon Dis. 2016; 11:1129–1137. PMID:
27313452.

15. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017; 195(5):557–582. PMID:
28128970.

16. Ahn J, Cho J. Current serum lung cancer biomarkers. J Mol Biomark Diagn. 2013; 4:2.

17. Srikanthan K, Feyh A, Visweshwar H, Shapiro JI, Sodhi K. Systematic review of metabolic syndrome biomarkers: a panel for early detection, management, and risk stratification in the West Virginian population. Int J Med Sci. 2016; 13(1):25–38. PMID:
26816492.

18. Fabbri LM, Hurd S. Global strategy for the diagnosis, management and prevention of COPD: 2003 update. Eur Respir J. 2003; 22(1):1–2. PMID:
12882441.

19. Nakayama M, Satoh H, Ishikawa H, Fujiwara M, Kamma H, Ohtsuka M, et al. Cytokeratin 19 fragment in patients with nonmalignant respiratory diseases. Chest. 2003; 123(6):2001–2006. PMID:
12796181.
20. Arai T, Inoue Y, Sugimoto C, Inoue Y, Nakao K, Takeuchi N, et al. CYFRA 21-1 as a disease severity marker for autoimmune pulmonary alveolar proteinosis. Respirology. 2014; 19(2):246–252. PMID:
24251830.

21. Han Y, Heo Y, Hong Y, Kwon SO, Kim WJ. Correlation between physical activity and lung function in dusty areas: results from the chronic obstructive pulmonary disease in dusty areas (CODA) cohort. Tuberc Respir Dis (Seoul). 2019; 82(4):311–318. PMID:
31172706.

22. Stieber P, Bodenmüller H, Banauch D, Hasholzner U, Dessauer A, Ofenloch-Hähnle B, et al. Cytokeratin 19 fragments: a new marker for non-small-cell lung cancer. Clin Biochem. 1993; 26(4):301–304. PMID:
7694815.

23. Zemans RL, Jacobson S, Keene J, Kechris K, Miller BE, Tal-Singer R, et al. Multiple biomarkers predict disease severity, progression and mortality in COPD. Respir Res. 2017; 18(1):117. PMID:
28610627.

24. Kim DK, Cho MH, Hersh CP, Lomas DA, Miller BE, Kong X, et al. Genome-wide association analysis of blood biomarkers in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012; 186(12):1238–1247. PMID:
23144326.

25. Brusselle G, Pavord ID, Landis S, Pascoe S, Lettis S, Morjaria N, et al. Blood eosinophil levels as a biomarker in COPD. Respir Med. 2018; 138:21–31. PMID:
29724389.

26. Park SY, Lee JG, Kim J, Park Y, Lee SK, Bae MK, et al. Preoperative serum CYFRA 21-1 level as a prognostic factor in surgically treated adenocarcinoma of lung. Lung Cancer. 2013; 79(2):156–160. PMID:
23206831.

27. Kim J, Jung H, Kim D, Lee S, Kim M, Park K. Lack of clinical utility for CYFRA 21-1 in medical screening. Korean J Fam Pract. 2018; 8(1):73–79.

28. Wieskopf B, Demangeat C, Purohit A, Stenger R, Gries P, Kreisman H, et al. Cyfra 21-1 as a biologic marker of non-small cell lung cancer. Evaluation of sensitivity, specificity, and prognostic role. Chest. 1995; 108(1):163–169. PMID:
7541742.
29. Simpson JK, Maher TM, Bentley J, Braybrooke R, Carter P, Costa MJ, et al. CYFRA-21-1 as a biomarker with prognostic potential in idiopathic pulmonary fibrosis: an analysis of the PROFILE cohort. Am J Respir Crit Care Med. 2017; 195:A6791.
30. Joo H, Park J, Lee SD, Oh YM. Comorbidities of chronic obstructive pulmonary disease in Koreans: a population-based study. J Korean Med Sci. 2012; 27(8):901–906. PMID:
22876057.

31. Park TS, Lee JS, Seo JB, Hong Y, Yoo JW, Kang BJ, KOLD Study Group, et al. Study design and outcomes of Korean obstructive lung disease (KOLD) cohort study. Tuberc Respir Dis (Seoul). 2014; 76(4):169–174. PMID:
24851130.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download