1. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007; 146:857–867. PMID:
17577005.

2. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962. PMID:
24315724.

3. Chao TF, Chiang CE, Liao JN, Chen TJ, Lip GYH, Chen SA. Comparing the effectiveness and safety of nonvitamin K antagonist oral anticoagulants and warfarin in elderly Asian patients with atrial fibrillation: a nationwide cohort study. Chest. 2020; 157:1266–1277. PMID:
31809694.
4. Chao TF, Chiang CE, Lin YJ, et al. Evolving changes of the use of oral anticoagulants and outcomes in patients with newly diagnosed atrial fibrillation in Taiwan. Circulation. 2018; 138:1485–1487. PMID:
30354355.

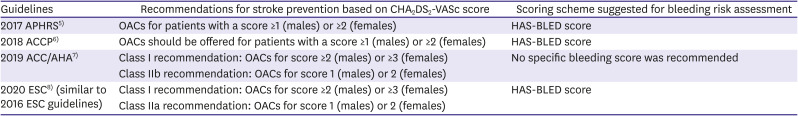
5. Chiang CE, Okumura K, Zhang S, et al. 2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation. J Arrhythm. 2017; 33:345–367. PMID:
28765771.

6. Lip GYH, Banerjee A, Boriani G, et al. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018; 154:1121–1201. PMID:
30144419.
7. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society in collaboration with the society of thoracic surgeons. Circulation. 2019; 140:e125–e151. PMID:
30686041.

8. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021; 42:373–498. PMID:
32860505.
9. Chao TF, Nedeljkovic MA, Lip GYH, Potpara TS. Stroke prevention in atrial fibrillation: comparison of recent international guidelines. Eur Heart J Suppl. 2020; 22:O53–60. PMID:
33380944.

10. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272. PMID:
19762550.
11. Banerjee A, Taillandier S, Olesen JB, et al. Ejection fraction and outcomes in patients with atrial fibrillation and heart failure: the Loire Valley Atrial Fibrillation Project. Eur J Heart Fail. 2012; 14:295–301. PMID:
22294759.

12. Uhm JS, Kim J, Yu HT, et al. Stroke and systemic embolism in patients with atrial fibrillation and heart failure according to heart failure type. ESC Heart Fail. 2021; 8:1582–1589. PMID:
33634593.

13. JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J. 2014; 78:1997–2021. PMID:
24965079.
14. Jung H, Sung JH, Yang PS, et al. Stroke risk stratification for atrial fibrillation patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2018; 72:2409–2411. PMID:
30384898.
15. Jung H, Yang PS, Jang E, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation with hypertrophic cardiomyopathy: a nationwide cohort study. Chest. 2019; 155:354–363. PMID:
30472021.
16. Steensig K, Olesen KKW, Thim T, et al. Should the presence or extent of coronary artery disease be quantified in the CHA2DS2-VASc score in atrial fibrillation? A report from the Western Denmark Heart registry. Thromb Haemost. 2018; 118:2162–2170. PMID:
30419601.

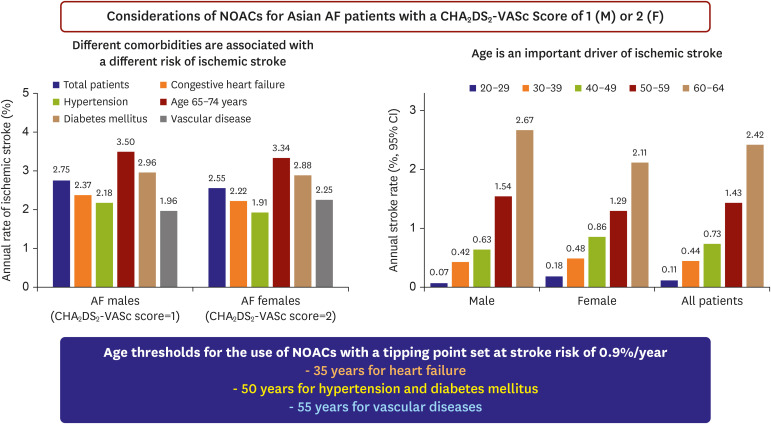
17. Chao TF, Wang KL, Liu CJ, et al. Age threshold for increased stroke risk among patients with atrial fibrillation: a nationwide cohort study from Taiwan. J Am Coll Cardiol. 2015; 66:1339–1347. PMID:
26383720.
18. Kim TH, Yang PS, Yu HT, et al. Age threshold for ischemic stroke risk in atrial fibrillation. Stroke. 2018; 49:1872–1879. PMID:
30012820.

19. Chao TF, Lip GY, Liu CJ, et al. Validation of a modified CHA2DS2-VASc score for stroke risk stratification in Asian patients with atrial fibrillation: a nationwide cohort study. Stroke. 2016; 47:2462–2469. PMID:
27625386.
20. NHFA CSANZ Atrial Fibrillation Guideline Working Group. Brieger D, Amerena J, et al. National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the diagnosis and management of atrial fibrillation 2018. Heart Lung Circ. 2018; 27:1209–1266. PMID:
30077228.

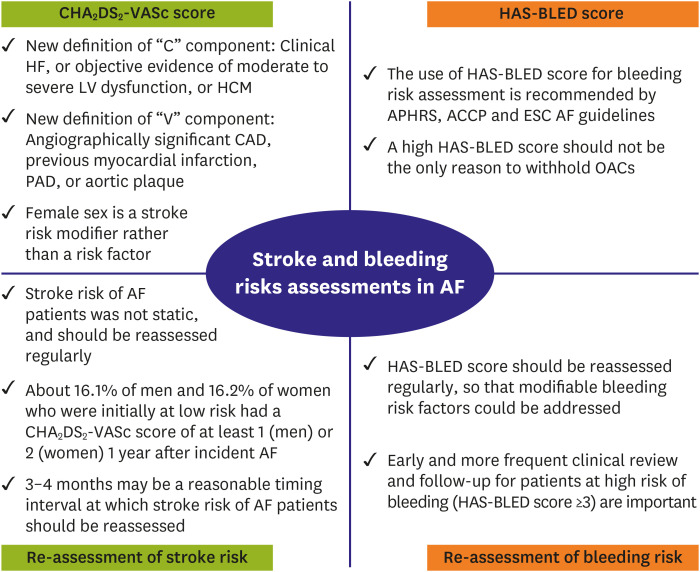
21. Nielsen PB, Skjøth F, Overvad TF, Larsen TB, Lip GYH. Female sex is a risk modifier rather than a risk factor for stroke in atrial fibrillation: should we use a CHA
2DS
2-VA score rather than CHA
2DS
2-VASc? Circulation. 2018; 137:832–840. PMID:
29459469.
22. Chao TF, Lip GYH, Lin YJ, et al. Major bleeding and intracranial hemorrhage risk prediction in patients with atrial fibrillation: attention to modifiable bleeding risk factors or use of a bleeding risk stratification score? A nationwide cohort study. Int J Cardiol. 2018; 254:157–161. PMID:
29407081.

23. Guo Y, Lane DA, Chen Y, Lip GYH. mAF-App II Trial investigators. Regular bleeding risk assessment associated with reduction in bleeding outcomes: the mAFA-II randomized trial. Am J Med. 2020; 133:1195–1202.e2. PMID:
32289310.

24. Chao TF, Chan YH, Chiang CE, et al. Continuation or discontinuation of oral anticoagulants after HAS-BLED scores increase in patients with atrial fibrillation. Clin Res Cardiol. 2021.

25. Chang TY, Lip GYH, Chen SA, Chao TF. Importance of risk reassessment in patients with atrial fibrillation in guidelines: assessing risk as a dynamic process. Can J Cardiol. 2019; 35:611–618. PMID:
31030863.

26. Chao TF, Lip GYH, Liu CJ, et al. Relationship of aging and incident comorbidities to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol. 2018; 71:122–132. PMID:
29325634.
27. Yoon M, Yang PS, Jang E, et al. Dynamic changes of CHA2DS2-VASc score and the risk of ischaemic stroke in Asian patients with atrial fibrillation: a nationwide cohort study. Thromb Haemost. 2018; 118:1296–1304. PMID:
29723875.

28. Chao TF, Liao JN, Tuan TC, et al. Incident co-morbidities in patients with atrial fibrillation initially with a CHA2DS2-VASc score of 0 (males) or 1 (females): implications for reassessment of stroke risk in initially ‘low-risk’ patients. Thromb Haemost. 2019; 119:1162–1170. PMID:
30900222.

29. Chao TF, Chiang CE, Chen TJ, Lip GYH, Chen SA. Reassessment of risk for stroke during follow-up of patients with atrial fibrillation. Ann Intern Med. 2019; 170:663–664. PMID:
30597483.

30. Chao TF, Chen SA, Lip GYH. Recommendations on stroke prevention for patients having a CHA
2DS
2-VASc score of 1 (males) or 2 (females) in 2019 atrial fibrillation guidelines. Trends Cardiovasc Med. 2019; 29:427–428. PMID:
30833072.
31. Olesen JB, Lip GY, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011; 342:d124. PMID:
21282258.

32. Chao TF, Liu CJ, Wang KL, et al. Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation? J Am Coll Cardiol. 2015; 65:635–642. PMID:
25677422.
33. Chao TF, Lip GYH, Lin YJ, et al. Age threshold for the use of non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with atrial fibrillation: insights into the optimal assessment of age and incident comorbidities. Eur Heart J. 2019; 40:1504–1514. PMID:
30605505.

34. Chao TF, Chiang CE, Chen SA. Stroke in atrial fibrillation - long-term follow-up of cardiovascular events. Arrhythm Electrophysiol Rev. 2013; 2:105–108. PMID:
26835049.
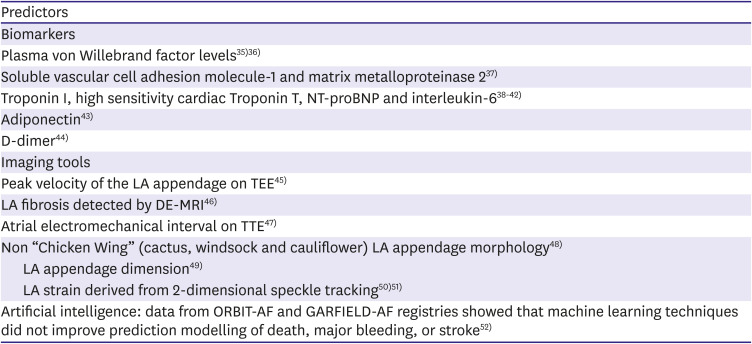
35. Conway DS, Pearce LA, Chin BS, Hart RG, Lip GY. Prognostic value of plasma von Willebrand factor and soluble P-selectin as indices of endothelial damage and platelet activation in 994 patients with nonvalvular atrial fibrillation. Circulation. 2003; 107:3141–3145. PMID:
12796127.

36. Roldán V, Marín F, Muiña B, et al. Plasma von Willebrand factor levels are an independent risk factor for adverse events including mortality and major bleeding in anticoagulated atrial fibrillation patients. J Am Coll Cardiol. 2011; 57:2496–2504. PMID:
21497043.

37. Ehrlich JR, Kaluzny M, Baumann S, Lehmann R, Hohnloser SH. Biomarkers of structural remodelling and endothelial dysfunction for prediction of cardiovascular events or death in patients with atrial fibrillation. Clin Res Cardiol. 2011; 100:1029–1036. PMID:
21725858.

38. Roldán V, Marín F, Díaz J, et al. High sensitivity cardiac troponin T and interleukin-6 predict adverse cardiovascular events and mortality in anticoagulated patients with atrial fibrillation. J Thromb Haemost. 2012; 10:1500–1507. PMID:
22681487.
39. Hijazi Z, Oldgren J, Andersson U, et al. Cardiac biomarkers are associated with an increased risk of stroke and death in patients with atrial fibrillation: a Randomized Evaluation of Long-term Anticoagulation Therapy (RE-LY) substudy. Circulation. 2012; 125:1605–1616. PMID:
22374183.
40. Hijazi Z, Lindbäck J, Alexander JH, et al. The ABC (age, biomarkers, clinical history) stroke risk score: a biomarker-based risk score for predicting stroke in atrial fibrillation. Eur Heart J. 2016; 37:1582–1590. PMID:
26920728.

41. Oldgren J, Hijazi Z, Lindbäck J, et al. Performance and validation of a novel biomarker-based stroke risk score for atrial fibrillation. Circulation. 2016; 134:1697–1707. PMID:
27569438.

42. Berg DD, Ruff CT, Jarolim P, et al. Performance of the ABC scores for assessing the risk of stroke or systemic embolism and bleeding in patients with atrial fibrillation in ENGAGE AF-TIMI 48. Circulation. 2019; 139:760–771. PMID:
30586727.

43. Hernández-Romero D, Jover E, Marín F, et al. The prognostic role of the adiponectin levels in atrial fibrillation. Eur J Clin Invest. 2013; 43:168–173. PMID:
23278336.

44. Mahé I, Bergmann JF, Chassany O, et al. A multicentric prospective study in usual care: D-dimer and cardiovascular events in patients with atrial fibrillation. Thromb Res. 2012; 129:693–699. PMID:
21917302.

45. Cianfrocca C, Loricchio ML, Pelliccia F, et al. C-reactive protein and left atrial appendage velocity are independent determinants of the risk of thrombogenesis in patients with atrial fibrillation. Int J Cardiol. 2010; 142:22–28. PMID:
19178964.

46. Daccarett M, Badger TJ, Akoum N, et al. Association of left atrial fibrosis detected by delayed-enhancement magnetic resonance imaging and the risk of stroke in patients with atrial fibrillation. J Am Coll Cardiol. 2011; 57:831–838. PMID:
21310320.

47. Chao TF, Lin YJ, Tsao HM, et al. Prolonged atrium electromechanical interval is associated with stroke in patients with atrial fibrillation after catheter ablation. J Cardiovasc Electrophysiol. 2013; 24:375–380. PMID:
23252831.

48. Di Biase L, Santangeli P, Anselmino M, et al. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study. J Am Coll Cardiol. 2012; 60:531–538. PMID:
22858289.
49. Beinart R, Heist EK, Newell JB, Holmvang G, Ruskin JN, Mansour M. Left atrial appendage dimensions predict the risk of stroke/TIA in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2011; 22:10–15. PMID:
20662984.

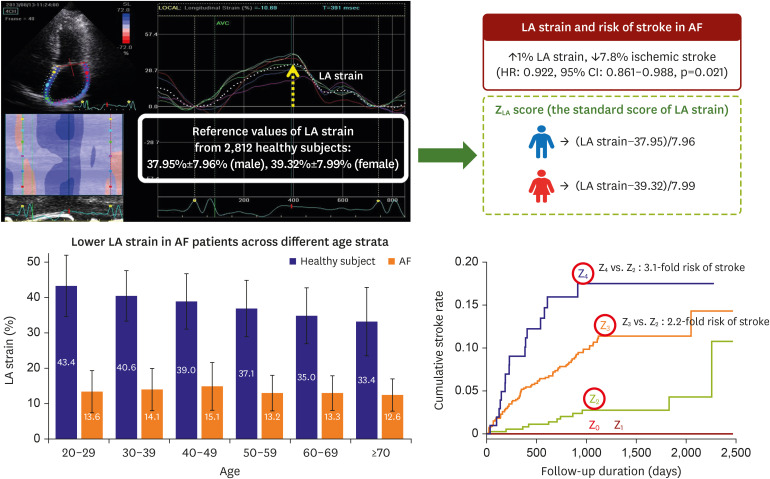
50. Liao JN, Chao TF, Kuo JY, et al. Global left atrial longitudinal strain using 3-beat method improves risk prediction of stroke over conventional echocardiography in atrial fibrillation. Circ Cardiovasc Imaging. 2020; 13:e010287. PMID:
32787500.

51. Liao JN, Chao TF, Hung CL, Chen SA. The decrease in peak atrial longitudinal strain in patients with atrial fibrillation as a practical parameter for stroke risk stratification. Heart Rhythm. 2021; 18:538–544. PMID:
33385571.

52. Loring Z, Mehrotra S, Piccini JP, et al. Machine learning does not improve upon traditional regression in predicting outcomes in atrial fibrillation: an analysis of the ORBIT-AF and GARFIELD-AF registries. Europace. 2020; 22:1635–1644. PMID:
32879969.

53. Rivera-Caravaca JM, Roldán V, Esteve-Pastor MA, et al. Long-term stroke risk prediction in patients with atrial fibrillation: comparison of the ABC-stroke and CHA
2DS
2-VASc scores. J Am Heart Assoc. 2017; 6:e006490. PMID:
28729407.
54. Oyama K, Giugliano RP, Berg DD, et al. Serial assessment of biomarkers and the risk of stroke or systemic embolism and bleeding in patients with atrial fibrillation in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2021; 42:1698–1706. PMID:
33760027.

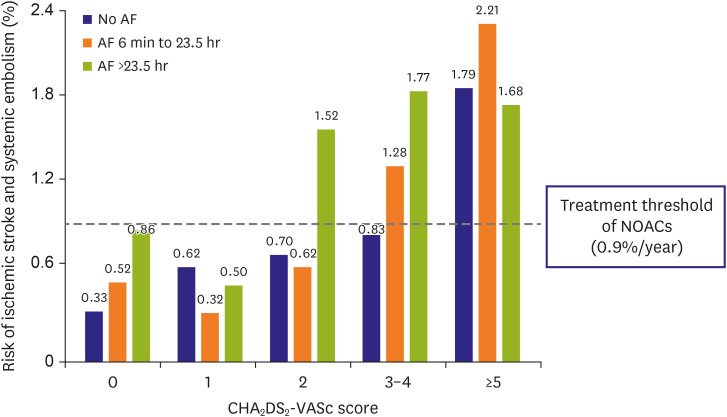
55. Kaplan RM, Koehler J, Ziegler PD, Sarkar S, Zweibel S, Passman RS. Stroke risk as a function of atrial fibrillation duration and CHA
2DS
2-VASc score. Circulation. 2019; 140:1639–1646. PMID:
31564126.
56. Goette A, Kalman JM, Aguinaga L, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Heart Rhythm. 2017; 14:e3–40. PMID:
27320515.

57. Hammwöhner M, Bukowska A, Mahardika W, Goette A. Clinical importance of atrial cardiomyopathy. Int J Cardiol. 2019; 287:174–180. PMID:
30527991.

58. Liao JN, Chao TF, Kuo JY, et al. Age, sex, and blood pressure-related influences on reference values of left atrial deformation and mechanics from a large-scale Asian population. Circ Cardiovasc Imaging. 2017; 10:e006077. PMID:
29021258.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download