1. Dubois EL, Cozen L. Avascular (aseptic) bone necrosis associated with systemic lupus erythematosus. JAMA. 1960; 174(8):966–971. PMID:
13724595.

2. Freund E. Bilateral aseptic necrosis of the femoral head: problems arising in a compensation case. Ann Surg. 1936; 104(1):100–106. PMID:
17856796.
3. Phemister DB. Changes in bones and joints resulting from interruption of circulation. I. General consideration and changes resulting from injury. Arch Surg. 1940; 41(2):436.
4. Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR. Nontraumatic osteonecrosis of the femoral head: Where do we stand today? A ten-year update. J Bone Joint Surg Am. 2015; 97(19):1604–1627. PMID:
26446969.
5. Kang JS, Park S, Song JH, Jung YY, Cho MR, Rhyu KH. Prevalence of osteonecrosis of the femoral head: a nationwide epidemiologic analysis in Korea. J Arthroplasty. 2009; 24(8):1178–1183. PMID:
19640674.
6. Ikeuchi K, Hasegawa Y, Seki T, Takegami Y, Amano T, Ishiguro N. Epidemiology of nontraumatic osteonecrosis of the femoral head in Japan. Mod Rheumatol. 2015; 25(2):278–281. PMID:
25036228.

7. Zhao DW, Yu M, Hu K, Wang W, Yang L, Wang BJ, et al. Prevalence of nontraumatic osteonecrosis of the femoral head and its associated risk factors in the Chinese population: results from a nationally representative survey. Chin Med J (Engl). 2015; 128(21):2843–2850. PMID:
26521779.
8. Bassoe P. The late manifestations of compressed air disease. Am J Med Sci. 1913; 145(4):526–542.
9. Chung SM, Ralston EL. Necrosis of the femoral head associated with sickle-cell anemia and its genetic variants. A review of the literature and study of thirteen cases. J Bone Joint Surg Am. 1969; 51(1):33–58. PMID:
4884827.
10. Chandler FA. Coronary disease of the hip. J Int Coll Surg. 1948; 11(1):34–36. PMID:
18910401.
11. Pietrogrande V, Mastromarino R. Osteopatia da prolunga trattamento cortisonico. ORTOP Traumatol. 1957; 25:791.
12. Hungerford DS, Zizic TM. Alcoholism associated ischemic necrosis of the femoral head. Early diagnosis and treatment. Clin Orthop Relat Res. 1978; (130):144–153.
13. Duparc J, Frot B, Gastambide D. Radiation-induced lesions of the hip. Chirurgie. 1974; 100(12):837–853. PMID:
4470062.
14. Gun'ko RI, Krasnov AS. Radiation injuries of the bones during treatment of uterine cancer. Vopr Onkol. 1988; 34(10):1188–1195. PMID:
3188420.
15. Arlet J, Franck JL, Nghiem L, Solera ML, de Graeve J. Multiple bone necroses and familial type I hyperlipemia. Apropos of a case report. Rev Rhum Mal Osteoartic. 1983; 50(2):149–153. PMID:
6857128.
16. Pierre-Jacques H, Glueck CJ, Mont MA, Hungerford DS. Familial heterozygous protein-S deficiency in a patient who had multifocal osteonecrosis. A case report. J Bone Joint Surg Am. 1997; 79(7):1079–1084. PMID:
9234887.

17. Arlet JD, Fauchier C, Hungerford DS. Histopathology of nontraumatic necrosis of the femoral head: topographic and evolutive aspects. Bone Circulation. Baltimore, MD, USA: Williams & Wilkins;1984.
18. Hauzeur JP, Perlmutter N, Appelboom T, Pasteels JL. Medullary impairment at early stage of non-traumatic osteonecrosis of the femoral head. Rheumatol Int. 1991; 11(4-5):215–217. PMID:
1784891.

19. Mont MA, Salem HS, Piuzzi NS, Goodman SB, Jones LC. Nontraumatic osteonecrosis of the femoral head: Where do we stand today?: A 5-year update. J Bone Joint Surg Am. 2020; 102(12):1084–1099. PMID:
32282421.
20. Björkman A, Svensson PJ, Hillarp A, Burtscher IM, Rünow A, Benoni G. Factor V leiden and prothrombin gene mutation: risk factors for osteonecrosis of the femoral head in adults. Clin Orthop Relat Res. 2004; (425):168–172.
21. Glueck CJ, Freiberg R, Tracy T, Stroop D, Wang P. Thrombophilia and hypofibrinolysis: pathophysiologies of osteonecrosis. Clin Orthop Relat Res. 1997; (334):43–56. PMID:
9005895.

22. Jones LC, Mont MA, Le TB, Petri M, Hungerford DS, Wang P, et al. Procoagulants and osteonecrosis. J Rheumatol. 2003; 30(4):783–791. PMID:
12672200.
23. Zalavras CG, Vartholomatos G, Dokou E, Malizos KN. Genetic background of osteonecrosis: associated with thrombophilic mutations? Clin Orthop Relat Res. 2004; (422):251–255.
24. Glueck CJ, Fontaine RN, Gruppo R, Stroop D, Sieve-Smith L, Tracy T, et al. The plasminogen activator inhibitor-1 gene, hypofibrinolysis, and osteonecrosis. Clin Orthop Relat Res. 1999; (366):133–146. PMID:
10627727.

25. Glueck CJ, Freiberg RA, Fontaine RN, Tracy T, Wang P. Hypofibrinolysis, thrombophilia, osteonecrosis. Clin Orthop Relat Res. 2001; (386):19–33. PMID:
11347834.

26. Korompilias AV, Gilkeson GS, Ortel TL, Seaber AV, Urbaniak JR. Anticardiolipin antibodies and osteonecrosis of the femoral head. Clin Orthop Relat Res. 1997; (345):174–180.

27. Seleznick MJ, Silveira LH, Espinoza LR. Avascular necrosis associated with anticardiolipin antibodies. J Rheumatol. 1991; 18(9):1416–1417. PMID:
1757948.
28. Glueck CJ, Freiberg RA, Boppana S, Wang P. Thrombophilia, hypofibrinolysis, the eNOS T-786C polymorphism, and multifocal osteonecrosis. J Bone Joint Surg Am. 2008; 90(10):2220–2229. PMID:
18829920.

29. Koo KH, Lee JS, Lee YJ, Kim KJ, Yoo JJ, Kim HJ. Endothelial nitric oxide synthase gene polymorphisms in patients with nontraumatic femoral head osteonecrosis. J Orthop Res. 2006; 24(8):1722–1728. PMID:
16779830.

30. Kim T, Hong JM, Lee J, Oh B, Park EK, Lee C, et al. Promoter polymorphisms of the vascular endothelial growth factor gene is associated with an osteonecrosis of the femoral head in the Korean population. Osteoarthritis Cartilage. 2008; 16(3):287–291. PMID:
17698375.

31. Lee YJ, Lee JS, Kang EH, Lee YK, Kim SY, Song YW, et al. Vascular endothelial growth factor polymorphisms in patients with steroid-induced femoral head osteonecrosis. J Orthop Res. 2012; 30(1):21–27. PMID:
21710604.

32. Rueda JC, Duque MA, Mantilla RD, Iglesias-Gamarra A. Osteonecrosis and antiphospholipid syndrome. J Clin Rheumatol. 2009; 15(3):130–132. PMID:
19300287.

33. Tektonidou MG, Moutsopoulos HM. Immunologic factors in the pathogenesis of osteonecrosis. Orthop Clin North Am. 2004; 35(3):259–263. viiPMID:
15271533.

34. Abu-Shakra M, Buskila D, Shoenfeld Y. Osteonecrosis in patients with SLE. Clin Rev Allergy Immunol. 2003; 25(1):13–24. PMID:
12794257.

35. Hedri H, Cherif M, Zouaghi K, Abderrahim E, Goucha R, Ben Hamida F, et al. Avascular osteonecrosis after renal transplantation. Transplant Proc. 2007; 39(4):1036–1038. PMID:
17524885.

36. Horiuchi H, Hashikura Y, Hisa K, Saito N, Ikegami T, Nakazawa Y, et al. Osteonecrosis of the femoral head in Japanese adults after liver transplantation: a preliminary report. J Orthop Sci. 2004; 9(2):119–121. PMID:
15045538.

37. Hutter CD. Dysbaric osteonecrosis: a reassessment and hypothesis. Med Hypotheses. 2000; 54(4):585–590. PMID:
10859644.

38. Jones JP. Epidemiological risk factors for non-traumatic osteonecrosis. Orthopade. 2000; 29(5):370–379. PMID:
10875131.

39. Katz K, Horev G, Grunebaum M, Yosipovitch Z. The natural history of osteonecrosis of the femoral head in children and adolescents who have Gaucher disease. J Bone Joint Surg Am. 1996; 78(1):14–19. PMID:
8550670.

40. Li H, Zhang J, He JW, Wang K, Wang GS, Jiang N, et al. Symptomatic osteonecrosis of the femoral head after adult orthotopic liver transplantation. Chin Med J (Engl). 2012; 125(14):2422–2426. PMID:
22882914.
41. Lieberman JR, Roth KM, Elsissy P, Dorey FJ, Kobashigawa JA. Symptomatic osteonecrosis of the hip and knee after cardiac transplantation. J Arthroplasty. 2008; 23(1):90–96. PMID:
18165036.

42. Rodrigue SW, Rosenthal DI, Barton NW, Zurakowski D, Mankin HJ. Risk factors for osteonecrosis in patients with type 1 Gaucher's disease. Clin Orthop Relat Res. 1999; (362):201–207.

43. Sayarlioglu M, Yuzbasioglu N, Inanc M, Kamali S, Cefle A, Karaman O, et al. Risk factors for avascular bone necrosis in patients with systemic lupus erythematosus. Rheumatol Int. 2012; 32(1):177–182. PMID:
20711782.

44. Shibatani M, Fujioka M, Arai Y, Takahashi K, Ueshima K, Okamoto M, et al. Degree of corticosteroid treatment within the first 2 months of renal transplantation has a strong influence on the incidence of osteonecrosis of the femoral head. Acta Orthop. 2008; 79(5):631–636. PMID:
18839369.

45. Tauchmanovà L, De Rosa G, Serio B, Fazioli F, Mainolfi C, Lombardi G, et al. Avascular necrosis in long-term survivors after allogeneic or autologous stem cell transplantation: a single center experience and a review. Cancer. 2003; 97(10):2453–2461. PMID:
12733144.
46. Toklu AS, Cimşit M. Dysbaric osteonecrosis in Turkish sponge divers. Undersea Hyperb Med. 2001; 28(2):83–88. PMID:
11908699.
47. Torii Y, Hasegawa Y, Kubo T, Kodera Y, Minami S, Morishita Y, et al. Osteonecrosis of the femoral head after allogeneic bone marrow transplantation. Clin Orthop Relat Res. 2001; (382):124–132.

48. Winquist EW, Bauman GS, Balogh J. Nontraumatic osteonecrosis after chemotherapy for testicular cancer: a systematic review. Am J Clin Oncol. 2001; 24(6):603–606. PMID:
11801763.
49. Dzik-Jurasz AS, Brooker S, Husband JE, Tait D. What is the prevalence of symptomatic or asymptomatic femoral head osteonecrosis in patients previously treated with chemoradiation? A magnetic resonance study of anal cancer patients. Clin Oncol (R Coll Radiol). 2001; 13(2):130–134. PMID:
11373876.

50. Yoon BH, Jones LC, Chen CH, Cheng EY, Cui Q, Drescher W, et al. Etiologic classification criteria of ARCO on femoral head osteonecrosis part 1: glucocorticoid-associated osteonecrosis. J Arthroplasty. 2019; 34(1):163–168.e1. PMID:
30348552.

51. Yoon BH, Jones LC, Chen CH, Cheng EY, Cui Q, Drescher W, et al. Etiologic classification criteria of ARCO on femoral head osteonecrosis part 2: alcohol-associated osteonecrosis. J Arthroplasty. 2019; 34(1):169–174.e1. PMID:
30348559.

52. Cui Q, Jo WL, Koo KH, Cheng EY, Drescher W, Goodman SB, et al. ARCO consensus on the pathogenesis of non-traumatic osteonecrosis of the femoral head. J Korean Med Sci. 2021; 36(10):e65. PMID:
33724736.

53. Cui Q, Wang GJ, Balian G. Steroid-induced adipogenesis in a pluripotential cell line from bone marrow. J Bone Joint Surg Am. 1997; 79(7):1054–1063. PMID:
9234882.

54. Cui Q, Wang Y, Saleh KJ, Wang GJ, Balian G. Alcohol-induced adipogenesis in a cloned bone-marrow stem cell. J Bone Joint Surg Am. 2006; 88(Suppl 3):148–154.

55. Miyanishi K, Yamamoto T, Irisa T, Yamashita A, Jingushi S, Noguchi Y, et al. Bone marrow fat cell enlargement and a rise in intraosseous pressure in steroid-treated rabbits with osteonecrosis. Bone. 2002; 30(1):185–190. PMID:
11792583.

56. Motomura G, Yamamoto T, Miyanishi K, Yamashita A, Sueishi K, Iwamoto Y. Bone marrow fat-cell enlargement in early steroid-induced osteonecrosis--a histomorphometric study of autopsy cases. Pathol Res Pract. 2005; 200(11-12):807–811. PMID:
15792124.

57. Peckett AJ, Wright DC, Riddell MC. The effects of glucocorticoids on adipose tissue lipid metabolism. Metabolism. 2011; 60(11):1500–1510. PMID:
21864867.

58. Wang GJ, Sweet DE, Reger SI, Thompson RC. Fat-cell changes as a mechanism of avascular necrosis of the femoral head in cortisone-treated rabbits. J Bone Joint Surg Am. 1977; 59(6):729–735. PMID:
908695.

59. Hungerford DS, Lennox DW. The importance of increased intraosseous pressure in the development of osteonecrosis of the femoral head: implications for treatment. Orthop Clin North Am. 1985; 16(4):635–654. PMID:
3903603.

60. Koo KH, Dussault R, Kaplan P, Kim R, Ahn IO, Christopher J, et al. Age-related marrow conversion in the proximal metaphysis of the femur: evaluation with T1-weighted MR imaging. Radiology. 1998; 206(3):745–748. PMID:
9494495.

61. Kricun ME. Red-yellow marrow conversion: its effect on the location of some solitary bone lesions. Skeletal Radiol. 1985; 14(1):10–19. PMID:
3895447.

62. Lausten GS, Arnoldi CC. Blood perfusion uneven in femoral head osteonecrosis. Doppler flowmetry and intraosseous pressure in 12 cases. Acta Orthop Scand. 1993; 64(5):533–536. PMID:
8237319.

63. Koo KH, Jeong ST, Jones JP Jr. Borderline necrosis of the femoral head. Clin Orthop Relat Res. 1999; (358):158–165.

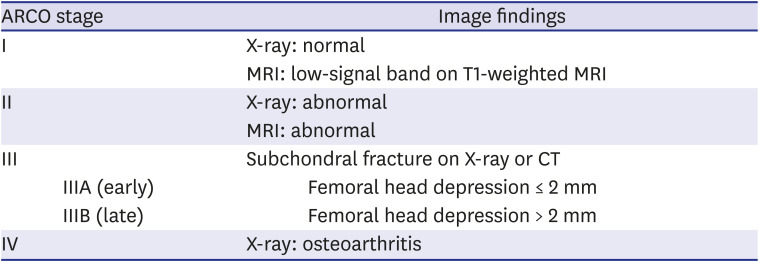
64. Yoon BH, Mont MA, Koo KH, Chen CH, Cheng EY, Cui Q, et al. The 2019 revised version of association research circulation osseous staging system of osteonecrosis of the femoral head. J Arthroplasty. 2020; 35(4):933–940. PMID:
31866252.

65. Goetz JE, Robinson DA, Pedersen DR, Conzemius MG, Brown TD. Cryoinsult parameter effects on the histologically apparent volume of experimentally induced osteonecrotic lesions. J Orthop Res. 2011; 29(6):931–937. PMID:
21259339.

66. Arlet J. Nontraumatic avascular necrosis of the femoral head. Past, present, and future. Clin Orthop Relat Res. 1992; (277):12–21.
67. Seamon J, Keller T, Saleh J, Cui Q. The pathogenesis of nontraumatic osteonecrosis. Arthritis. 2012; 2012:601763. PMID:
23243507.

68. Jones JP Jr. Concepts of etiology and early pathogenesis of osteonecrosis. Instr Course Lect. 1994; 43:499–512. PMID:
9097180.
69. Jones JP Jr, Peltier LF. Alcoholism, hypercortisonism, fat embolism and osseous avascular necrosis. 1971. Clin Orthop Relat Res. 2001; (393):4–12.
70. Steinberg ME, Brighton CT, Steinberg DR, Tooze SE, Hayken GD. Treatment of avascular necrosis of the femoral head by a combination of bone grafting, decompression, and electrical stimulation. Clin Orthop Relat Res. 1984; (186):137–153.

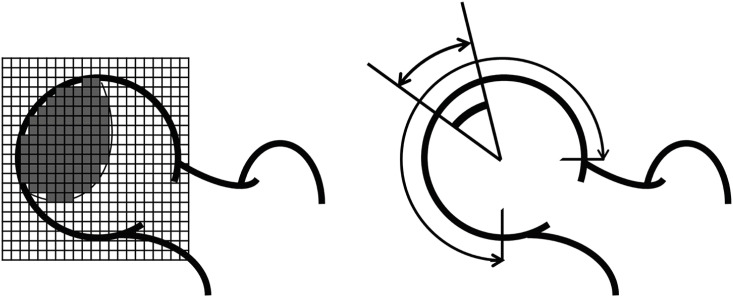
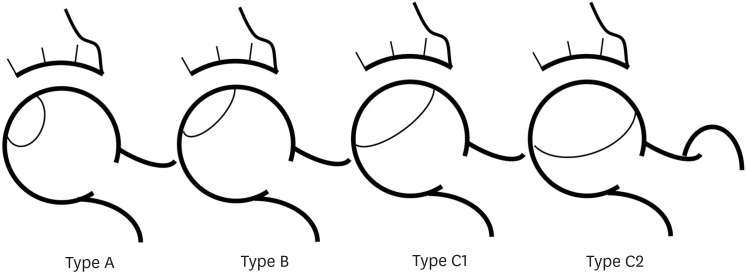
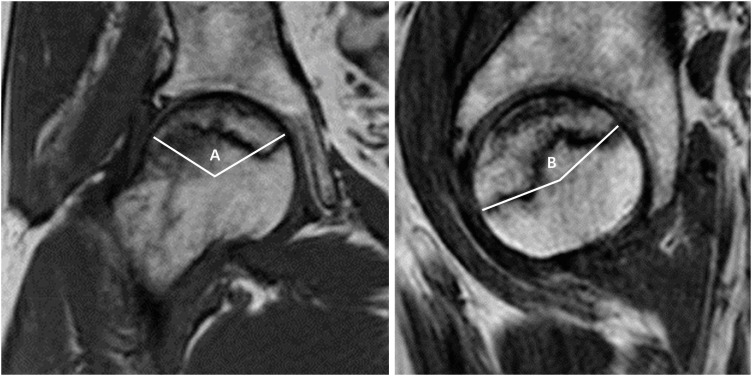
71. Nishii T, Sugano N, Ohzono K, Sakai T, Sato Y, Yoshikawa H. Significance of lesion size and location in the prediction of collapse of osteonecrosis of the femoral head: a new three-dimensional quantification using magnetic resonance imaging. J Orthop Res. 2002; 20(1):130–136. PMID:
11853079.

72. Nakasone S, Takao M, Sakai T, Nishii T, Sugano N. Does the extent of osteonecrosis affect the survival of hip resurfacing? Clin Orthop Relat Res. 2013; 471(6):1926–1934. PMID:
23397316.

73. Kerboul M, Thomine J, Postel M, Merle d'Aubigné R. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974; 56-B(2):291–296.

74. Ha YC, Kim HJ, Kim SY, Kim KC, Lee YK, Koo KH. Effects of age and body mass index on the results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. J Bone Joint Surg Am. 2010; 92(2):314–321. PMID:
20124057.

75. Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K. The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci. 2002; 7(5):601–605. PMID:
12355139.

76. Ha YC, Jung WH, Kim JR, Seong NH, Kim SY, Koo KH. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006; 88(Suppl 3):35–40.

77. Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995; 77-B(1):34–41.

78. Koo KH, Ahn IO, Kim R, Song HR, Jeong ST, Na JB, et al. Bone marrow edema and associated pain in early stage osteonecrosis of the femoral head: prospective study with serial MR images. Radiology. 1999; 213(3):715–722. PMID:
10580944.

79. Ajmal M, Matas AJ, Kuskowski M, Cheng EY. Does statin usage reduce the risk of corticosteroid-related osteonecrosis in renal transplant population? Orthop Clin North Am. 2009; 40(2):235–239. PMID:
19358908.

80. Chotanaphuti T, Thongprasert S, Laoruengthana A. Low molecular weight heparin prevents the progression of precollapse osteonecrosis of the hip. J Med Assoc Thai. 2013; 96(10):1326–1330. PMID:
24350415.
81. Glueck CJ, Freiberg RA, Sieve L, Wang P. Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res. 2005; (435):164–170.

82. Glueck CJ, Freiberg RA, Wissman R, Wang P. Long term anticoagulation (4-16 years) stops progression of idiopathic hip osteonecrosis associated with familial thrombophilia. Adv Orthop. 2015; 2015:138382. PMID:
25709842.

83. Pengde K, Fuxing P, Bin S, Jing Y, Jingqiu C. Lovastatin inhibits adipogenesis and prevents osteonecrosis in steroid-treated rabbits. Joint Bone Spine. 2008; 75(6):696–701. PMID:
18620886.

84. Pritchett JW. Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clin Orthop Relat Res. 2001; (386):173–178.

85. Agarwala S, Shetty V, Karumuri LK, Vijayvargiya M. Patellar resurfacing versus nonresurfacing with patellaplasty in total knee arthroplasty. Indian J Orthop. 2018; 52(4):393–398. PMID:
30078898.

86. Chen CH, Chang JK, Lai KA, Hou SM, Chang CH, Wang GJ. Alendronate in the prevention of collapse of the femoral head in nontraumatic osteonecrosis: a two-year multicenter, prospective, randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2012; 64(5):1572–1578. PMID:
22127729.

87. Lai KA, Shen WJ, Yang CY, Shao CJ, Hsu JT, Lin RM. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J Bone Joint Surg Am. 2005; 87(10):2155–2159. PMID:
16203877.
88. Lee YK, Ha YC, Cho YJ, Suh KT, Kim SY, Won YY, et al. Does zoledronate prevent femoral head collapse from osteonecrosis? A prospective, randomized, open-label, multicenter study. J Bone Joint Surg Am. 2015; 97(14):1142–1148. PMID:
26178889.
89. Nishii T, Sugano N, Miki H, Hashimoto J, Yoshikawa H. Does alendronate prevent collapse in osteonecrosis of the femoral head? Clin Orthop Relat Res. 2006; 443(443):273–279. PMID:
16462451.

90. Albers A, Carli A, Routy B, Harvey EJ, Séguin C. Treatment with acetylsalicylic acid prevents short to mid-term radiographic progression of nontraumatic osteonecrosis of the femoral head: a pilot study. Can J Surg. 2015; 58(3):198–205. PMID:
26011853.

91. Claßen T, Becker A, Landgraeber S, Haversath M, Li X, Zilkens C, et al. Long-term clinical results after iloprost treatment for bone marrow edema and avascular necrosis. Orthop Rev (Pavia). 2016; 8(1):6150. PMID:
27114807.

92. Jäger M, Zilkens C, Bittersohl B, Matheney T, Kozina G, Blondin D, et al. Efficiency of iloprost treatment for osseous malperfusion. Int Orthop. 2011; 35(5):761–765. PMID:
20306261.

93. Pazianas M, Abrahamsen B. Safety of bisphosphonates. Bone. 2011; 49(1):103–110. PMID:
21236370.

94. Pountos I, Giannoudis PV. The role of iloprost on bone edema and osteonecrosis: safety and clinical results. Expert Opin Drug Saf. 2018; 17(3):225–233. PMID:
29315006.

96. Lee YJ, Cui Q, Koo KH. Is there a role of pharmacological treatments in the prevention or treatment of osteonecrosis of the femoral head?: A systematic review. J Bone Metab. 2019; 26(1):13–18. PMID:
30899719.

97. Yoon BH, Lee YK, Kim KC, Ha YC, Koo KH. No differences in the efficacy among various core decompression modalities and non-operative treatment: a network meta-analysis. Int Orthop. 2018; 42(12):2737–2743. PMID:
29855682.

98. Hernigou P, Dubory A, Homma Y, Guissou I, Flouzat Lachaniette CH, Chevallier N, et al. Cell therapy versus simultaneous contralateral decompression in symptomatic corticosteroid osteonecrosis: a thirty year follow-up prospective randomized study of one hundred and twenty five adult patients. Int Orthop. 2018; 42(7):1639–1649. PMID:
29744647.
99. Kang JS, Suh YJ, Moon KH, Park JS, Roh TH, Park MH, et al. Clinical efficiency of bone marrow mesenchymal stem cell implantation for osteonecrosis of the femoral head: a matched pair control study with simple core decompression. Stem Cell Res Ther. 2018; 9(1):274. PMID:
30359323.

100. Li X, Xu X, Wu W. Comparison of bone marrow mesenchymal stem cells and core decompression in treatment of osteonecrosis of the femoral head: a meta-analysis. Int J Clin Exp Pathol. 2014; 7(8):5024–5030. PMID:
25197374.
101. Ma Y, Wang T, Liao J, Gu H, Lin X, Jiang Q, et al. Efficacy of autologous bone marrow buffy coat grafting combined with core decompression in patients with avascular necrosis of femoral head: a prospective, double-blinded, randomized, controlled study. Stem Cell Res Ther. 2014; 5(5):115. PMID:
25315149.

102. Sen RK, Tripathy SK, Aggarwal S, Marwaha N, Sharma RR, Khandelwal N. Early results of core decompression and autologous bone marrow mononuclear cells instillation in femoral head osteonecrosis: a randomized control study. J Arthroplasty. 2012; 27(5):679–686. PMID:
22000577.
103. Zhao D, Cui D, Wang B, Tian F, Guo L, Yang L, et al. Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone. 2012; 50(1):325–330. PMID:
22094904.

104. Lim YW, Kim YS, Lee JW, Kwon SY. Stem cell implantation for osteonecrosis of the femoral head. Exp Mol Med. 2013; 45(11):e61. PMID:
24232260.

105. Nally FJ, Zanotti G, Buttaro MA, Diaz Dilernia F, Mansilla IG, Comba FM, et al. THA conversion rate comparing decompression alone, with autologous bone graft or stem cells in osteonecrosis. Hip Int. 2018; 28(2):189–193. PMID:
29027191.

106. Pepke W, Kasten P, Beckmann NA, Janicki P, Egermann M. Core decompression and autologous bone marrow concentrate for treatment of femoral head osteonecrosis: a randomized prospective study. Orthop Rev (Pavia). 2016; 8(1):6162. PMID:
27114808.

107. Nishio A, Sugioka Y. A new technique of the varus osteotomy at the upper end of the femur. Orthop Traumatol. 1971; 20(3):381–386.

108. Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res. 1978; (130):191–201.
109. Lee YK, Park CH, Ha YC, Kim DY, Lyu SH, Koo KH. Comparison of surgical parameters and results between curved varus osteotomy and rotational osteotomy for osteonecrosis of the femoral head. Clin Orthop Surg. 2017; 9(2):160–168. PMID:
28567217.

110. Judet J, Judet H, Gilbert A. Trial revascularization of the femur head with a pediculed fibular transplant. Rev Chir Orthop Reparatrice Appar Mot. 1980; 66(Suppl 2):65. PMID:
6453381.
111. Urbaniak JR, Coogan PG, Gunneson EB, Nunley JA. Treatment of osteonecrosis of the femoral head with free vascularized fibular grafting. A long-term follow-up study of one hundred and three hips. J Bone Joint Surg Am. 1995; 77(5):681–694. PMID:
7744893.

112. Yoo MC, Chung DW, Hahn CS. Free vascularized fibula grafting for the treatment of osteonecrosis of the femoral head. Clin Orthop Relat Res. 1992; (277):128–138.

113. Zhao D, Xu D, Wang W, Cui X. Iliac graft vascularization for femoral head osteonecrosis. Clin Orthop Relat Res. 2006; 442:171–179. PMID:
16394757.

114. Amstutz HC, Le Duff MJ. Current status of hemi-resurfacing arthroplasty for osteonecrosis of the hip: a 27-year experience. Orthop Clin North Am. 2009; 40(2):275–282. PMID:
19358913.

115. De Smet KA, Van Der Straeten C, Van Orsouw M, Doubi R, Backers K, Grammatopoulos G. Revisions of metal-on-metal hip resurfacing: lessons learned and improved outcome. Orthop Clin North Am. 2011; 42(2):259–269. ixPMID:
21435500.

116. Zustin J, Sauter G, Morlock MM, Rüther W, Amling M. Association of osteonecrosis and failure of hip resurfacing arthroplasty. Clin Orthop Relat Res. 2010; 468(3):756–761. PMID:
19597896.

117. Kamath AF, Prieto H, Lewallen DG. Alternative bearings in total hip arthroplasty in the young patient. Orthop Clin North Am. 2013; 44(4):451–462. PMID:
24095062.

118. Muratoglu OK, Bragdon CR, O'Connor DO, Jasty M, Harris WH. A novel method of cross-linking ultra-high-molecular-weight polyethylene to improve wear, reduce oxidation, and retain mechanical properties. Recipient of the 1999 HAP Paul Award. J Arthroplasty. 2001; 16(2):149–160. PMID:
11222887.
119. Min BW, Lee KJ, Song KS, Bae KC, Cho CH. Highly cross-linked polyethylene in total hip arthroplasty for osteonecrosis of the femoral head: a minimum 5-year follow-up study. J Arthroplasty. 2013; 28(3):526–530. PMID:
23146583.
120. Kim YH, Choi Y, Kim JS. Cementless total hip arthroplasty with alumina-on-highly cross-linked polyethylene bearing in young patients with femoral head osteonecrosis. J Arthroplasty. 2011; 26(2):218–223. PMID:
20452176.

121. Kim YH, Park JW, Patel C, Kim DY. Polyethylene wear and osteolysis after cementless total hip arthroplasty with alumina-on-highly cross-linked polyethylene bearings in patients younger than thirty years of age. J Bone Joint Surg Am. 2013; 95(12):1088–1093. PMID:
23783205.

122. Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008; 90(2):329–336. PMID:
18245593.

123. Lee YK, Ha YC, Yoo JI, Jo WL, Kim KC, Koo KH. Mid-term results of the BIOLOX delta ceramic-on-ceramic total hip arthroplasty. Bone Joint J. 2017; 99-B(6):741–748. PMID:
28566392.

124. Park YS, Park SJ, Lim SJ. Ten-year results after cementless THA with a sandwich-type alumina ceramic bearing. Orthopedics. 2010; 33(11):796. PMID:
21053885.

125. Baek SH, Kim SY. Cementless total hip arthroplasty with alumina bearings in patients younger than fifty with femoral head osteonecrosis. J Bone Joint Surg Am. 2008; 90(6):1314–1320. PMID:
18519326.

126. Kang BJ, Ha YC, Ham DW, Hwang SC, Lee YK, Koo KH. Third-generation alumina-on-alumina total hip arthroplasty: 14 to 16-year follow-up study. J Arthroplasty. 2015; 30(3):411–415. PMID:
25449586.

127. Konan S, Alazzawi S, Yoon BH, Cha YH, Koo KH. A focused update on preventing ceramic fractures in hip arthroplasty: is the ‘cup’ half full? Bone Joint J. 2019; 101-B(8):897–901. PMID:
31362553.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download