This article has been
cited by other articles in ScienceCentral.
Abstract
Coronavirus disease was first reported in December 2019, and the World Health Organization declared it as a pandemic on March 11, 2020. The virus is known to attack various vital organs, including the respiratory system. Patients sometimes require positive pressure ventilation and tracheostomy. Because tracheostomy is a droplet-spreading procedure, medical staff should protect themselves against the risk of transmission of this contagious viral disease. In our case, we performed tracheostomy for a 70-year-old man with coronavirus disease 2019 (COVID-19) who had required more oxygen with gradual weakness of respiratory muscle to maintain his arterial oxygen saturation. We focused on the risks of the medical staffs and patients, and minimized them at the same time using temporary balloon over-inflation, pre-operative adjustment of endotracheal tube position, and attachment of a transparent film dressing to the surgical field without stopping the ventilator while following routine safety measures. Fourteen days after the tracheostomy, all participating medical staff members were healthy and asymptomatic. The patient was discharged 105 days after the COVID-19 diagnosis.
Keywords: COVID-19, Sputum, Tracheostomy, Transmission
INTRODUCTION
Since the first case report in Wuhan, China, in December 2019, coronavirus disease 2019 (COVID-19) has rapidly spread worldwide with declaration of ‘pandemic’ by the World Health Organization (WHO) on March 11, 2020.
1 This contagious virus is transmitted by droplets from the nose or mouth to other people who might come in contact with the virus by touch or inhalation (R0 value, 1.4–2.5).
2 As of May 5, 2020, 3,517,345 cases with 243,401 deaths (6.92% mortality rate) have been confirmed worldwide; in Korea, the same are 10,804 and 254 (2.35%), respectively.
3 The WHO–China Joint Mission reported that, among 55,924 laboratory-confirmed cases in China, severe cases (dyspnea, respiratory rate ≥ 30/min, oxygen saturation ≤ 93%, partial pressure of arterial oxygen to fraction of inspired oxygen [PaO
2/FiO
2] ratio < 300 mmHg, increase in lung infiltrates > 50% within 24–48 hours) comprised 13.8% and critical cases (respiratory failure, shock, and multiple organ dysfunction or failure) comprised 6.1%.
4
In the respiratory system, it begins with a pattern similar to that of viral pneumonia and progresses to respiratory failure in some cases; thus, clinicians must decide appropriate timing to perform tracheostomy.
56 During tracheostomy, there is a high risk of viral spread through the opening of the trachea to medical staff. It is important to prevent the spread of droplets to lower the risk of medical staff contracting COVID-19 at the forefront. Here we report a case of tracheostomy that was performed in a way that minimized the risk to the patient by maintaining ventilation and simultaneously minimized the risk of transmission to the treating medical staffs.
CASE DESCRIPTION
History and clinical features of the case
Four days after symptoms first occurred, a 70-year-old man received a laboratory-confirmed diagnosis of COVID-19 through real-time reverse transcription polymerase chain reaction. His respiratory symptoms such as dyspnea and tachypnea became exacerbated on the 7th day and his arterial partial pressure of oxygen (PaO2) was 68.2 mmHg on 0.4 of fraction of inspired oxygen (FiO2) with 4 L/min via nasal cannula. He was transferred from a local hospital to our hospital's intensive care unit (ICU) on March 18, 2020. His dyspnea gradually worsened with 60.5 mmHg of PaO2 on FiO2 0.9 and 40 L/min of high flow nasal cannula, so intubation was performed on the 20th day after transfer. The patient remained on a ventilator for 8 days and was then extubated. However, he was unable to breathe properly and was re-intubated 2 days later because he could not enough expectorate respiratory secretion with his weak respiratory muscle. We planned to perform a tracheostomy 2 days after the re-intubation for a prolonged course of ventilator care was expected.
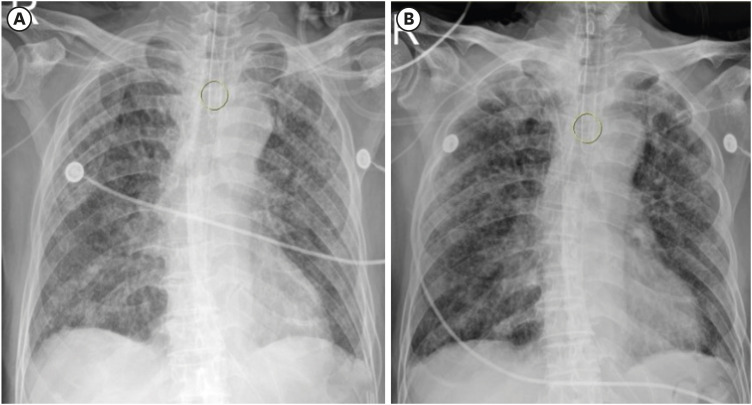
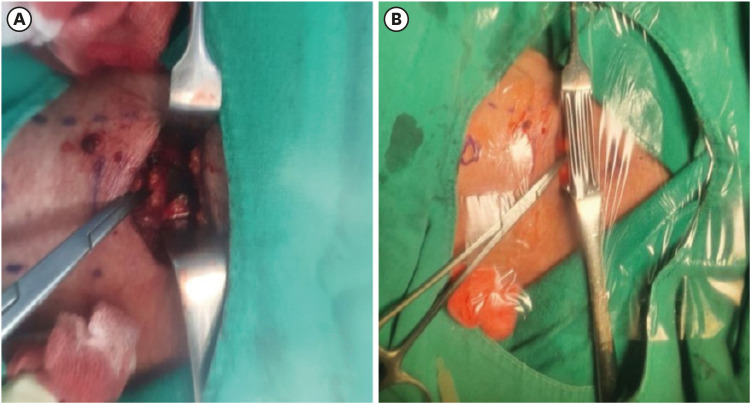
A preoperative chest X-ray was taken to check the position of the endotracheal (ET) tube tip, and the tube was then advanced to reposition the balloon to below the second tracheal ring. Another X-ray was taken to confirm that the balloon was located just above the carina, at which time surgical preparation was performed (
Fig. 1). The patient had thrombocytopenia caused by septic shock, and surgery was performed immediately after the transfusion of platelets to prevent intraoperative bleeding.
Fig. 1
Before surgery, chest radiography was used to adjust the position of the place where the balloon was supposed to be between the level of the second tracheal ring and the carina. (A) Before adjustment tube (B) after adjustment tube.
Surgery of tracheostomy
The surgical team consisted of an operator, an assistant, and a surgical intensivist; to minimize the number of participants, the nursing staff did not participate. The surgery was performed at bedside in a negatively pressured ICU room to minimize the risks of transmission during transfer and worsening of the patient's condition. The tracheostomy was performed in a surgical rather than percutaneous manner due to the risk of droplet transmission, the patient’s desaturation during bronchoscopy, and a distance of only 2.5 cm between the cricoid cartilage and the jugular notch.
6 All participating staff members applied personal protective equipment (PPE) consisting of a Level C powered air-purifying respirator (PAPR) with an aseptic waterproof surgical gown and gloves, while the patient was fitted with a full sterile drape just like in the operating room in the supine position with the neck extended. Because wearing headlamp would be difficult due to the protective hood, a portable astral lamp was moved to the ICU to provide additional light. A bipolar electrocoagulator was not used to prevent droplet aerosolization. Due to the continuous injection of sedatives and neuromuscular blockers for acute respiratory distress syndrome and the dyssynchrony to mechanical ventilation, only a 50-μg bolus of fentanyl was injected with pre-oxygenation at the intensivist's decision at the start of the operation. A transverse incision with the local injection of lidocaine was made 1.5 cm above the jugular notch considering the low level of cricoid cartilage, and the surgery proceeded in a routine manner.
Prior to opening of the second tracheal ring, the FiO
2 was lowered to 0.4 and the balloon was temporarily overinflated. The balloon was below the level of the tracheal opening when we observed it through the opening as it was positioned preoperatively (
Fig. 2A). No droplets escaped the opening due to the repositioned and overinflated balloon. The ET tube was withdrawn until the tip of the tube reached above the tracheal opening. During withdrawal, to prevent the spread of droplets, pausing the ventilator was considered before balloon deflation, but because of the patient's poor condition, a transparent film dressing was attached to the neck and the ventilation was continued (
Fig. 2B). In this process, droplet spread caused by ventilator flow was protected by the film. Immediately after ET tube tip repositioning, a hole was made on a transparent film dressing with scissors and a tracheostomy tube was immediately inserted. After a quick check of tracheostomy tube patency with a rubber catheter, the ventilator was connected, the tidal volume was checked, and the existing ET tube was removed. During the surgery, the patient's oxygen saturation with a peripheral pulse oximeter was maintained at above 98%. Fourteen days after the tracheostomy, all participating medical staff members were healthy and asymptomatic. The patient was discharged 105 days after the diagnosis of COVID-19 with a cuffless tracheostomy tube.
Fig. 2
Around tracheal manipulation. (A) Balloon is below the tracheal incision without air leakage through its side. (B) Through transparent membrane, tube withdrawal can be seen without pause of ventilator and spreading droplets.
Ethics statement
This case was approved by the Institutional Review Board of the National Medical Center (NMC-2006-018), which waived the need for informed consent.
DISCUSSION
According to the WHO report by the WHO–China Joint Mission, COVID-19 is a contagious viral disease that progresses to severe status requiring intensive care in 13.8% of cases; approximately half of these progress to critical status requiring ventilator care with acute respiratory distress syndrome. Therefore, tracheostomy should be considered in some cases.
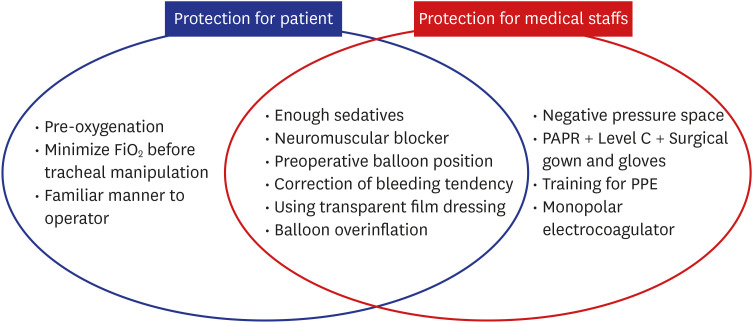
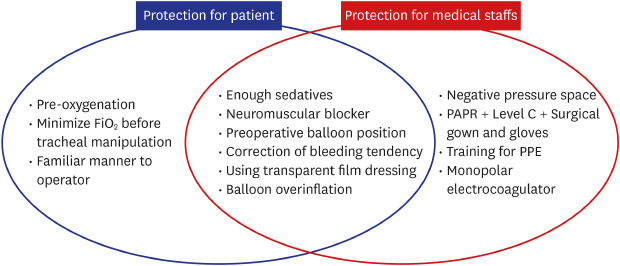
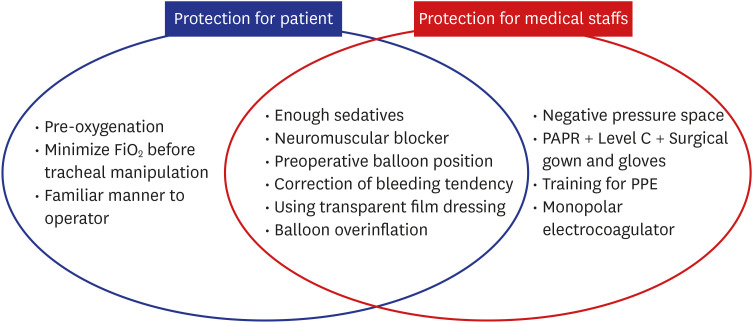
4 However, this surgery produces many droplets, so methods are required to prevent droplet spread to ensure medical staffs and patients safety (
Fig. 3).
7
Fig. 3
Procedures to protect patient (left), medical staff (right), and both (middle).
FiO2 = fraction of inspired oxygen, PAPR = powered air-purifying respirator, PPE = personal protective equipment.
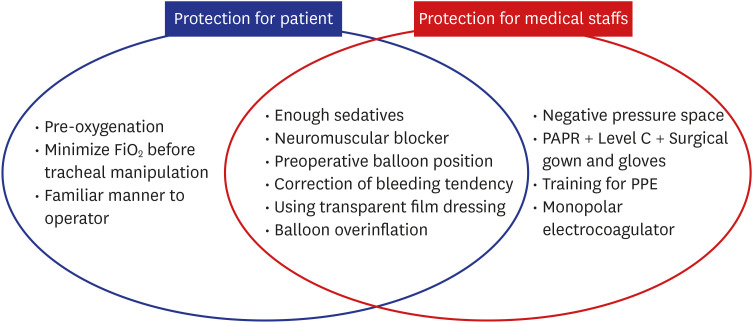
The surgery room should be chosen depending on each hospital's situation. However, considering medical staff safety, a negative pressure room is preferred.
6 In cases of droplet-induced transmission such as COVID-19, the use of appropriate PPE (Level C PAPR) is recommended, and medical staffs should be well trained in advance to safely wear and remove them.
8 Full sedatives and muscle relaxants are needed to prevent coughing during tracheal manipulation.
6 To prevent balloon rupture that can cause droplet spread and cease patient oxygenation, balloon positioning below the tracheal opening can be helpful. In addition, overinflation just below tracheal opening can prevent air leakage through the gap between the balloon and the tracheal wall with spreading droplets. During withdrawal of the ET tube with deflated balloon for insertion of tracheostomy tube, ventilator flow can spread droplets or mucus through the opening. The transparent film dressing attached to the surgical field could block droplet spread; thus, pausing of the ventilator was unnecessary. It is important to correct bleeding tendency to prevent blood aspiration and reduce aerosolization caused by electrocoagulation during tracheal manipulation. For the same reason, a monopolar coagulator is preferred to serve as a bipolar coagulator for coagulation.
9
The patient risk can be reduced by choosing the percutaneous or surgical method, which is more skilled to the surgeon, and considers patient-specific factors (e.g., anatomic variation). Sufficient pre-oxygenation is needed before surgery, and FiO
2 should be reduced to the minimum that the patient can tolerate to prevent airway fire with electrocoagulation during tracheal manipulation.
10 The effect of balloon positioning just above the carina is the same as described above. Because the transparent film dressing could block the spread of droplets during tube withdrawal, the ventilator did not stop. This can help maintain the patient's oxygen saturation and ensure medical staff safety. The reasons to correct the bleeding tendency before surgery are as described above.
The present case of COVID-19 required assisted ventilation by weak respiratory muscle for a long time, and the tracheostomy was indispensable to save his life. Tracheostomy using an ET tube balloon and a transparent film dressing can minimize droplet spread and keep patients and medical staffs safe during the surgical procedure.
ACKNOWLEDGMENTS
All authors thank the doctors, nurses, and assistants dedicated to treating COVID-19 patients at National Medical Center, Korea.
References
1. Du Toit A. Outbreak of a novel coronavirus. Nat Rev Microbiol. 2020; 18(3):123. PMID:
31988490.

2. Phan LT, Nguyen TV, Luong QC, Nguyen TV, Nguyen HT, Le HQ, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020; 382(9):872–874. PMID:
31991079.

5. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061.

6. Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T, et al. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020; 277(8):2173–2184. PMID:
32314050.

7. Wei WI, Tuen HH, Ng RW, Lam LK. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope. 2003; 113(10):1777–1779. PMID:
14520105.

9. Givi B, Schiff BA, Chinn SB, Clayburgh D, Iyer NG, Jalisi S, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020; 146(6):579–584.

10. Sosis MB, Braverman B. Prevention of cautery-induced airway fires with special endotracheal tubes. Anesth Analg. 1993; 77(4):846–847. PMID:
8214674.