INTRODUCTION
Mature cystic teratoma (MCT) is the most common germ cell tumor of the ovary accounting for about 10%–25% of all ovarian neoplasms and 60% of all benign ovarian neoplasms. MCT is most common in adolescents and women of reproductive age. Although most MCTs are asymptomatic, it can be associated with various local complications, including torsion (16%), rupture (1%–4%), malignant transformation (1%–2%), and infection (1%). Rarely, MCT can be associated with paraneoplastic syndrome, such as autoimmune hemolytic anemia and anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis.
1
Anti-NMDAR encephalitis is a recently identified autoimmune encephalitis in which autoantibodies target the NR1 subunit of the NMDAR in the brain, leading to a wide range of neuropsychiatric symptoms.
23 NMDARs are known to play a crucial role in synaptic plasticity, which is involved in memory, learning, and cognition. About 80% of the patients are women and nearly half of them are reported to have an ovarian teratoma.
45 The association between ovarian teratoma and anti-NMDAR encephalitis still remains unrecognized among gynecologists. We report here a case of anti-NMDAR encephalitis that was related to ovarian MCT.
CASE DESCRIPTION
A previously healthy 24-year-old woman had been admitted to a local hospital 10 days before on suspicion of meningitis due to fever, headache, nausea, and malaise. She subsequently became drowsy, incontinent, and unresponsive to external stimuli for the last 4 days. She was referred to our emergency center on January 25, 2017 with complaints of abnormal movement and decreased mental status.
The patient's initial vital signs were stable. Her mental status was stupor and she was not able to obey to command. Involuntary movements of both arms and legs were present. However, brainstem reflexes were normal and there was no evidence of motor weakness or sensory deficit. Pathologic reflexes were absent. Routine laboratory examinations were normal except mild leukocytosis (white blood cell [WBC], 12,790/µL). Cerebrospinal fluid (CSF) examination disclosed mild pleocytosis (WBC, 260/µL; lymphocyte, 91%) and CSF protein (25.7 mg/dL) and glucose (72 mg/dL) were within normal range. All viral and bacterial markers were negative. Brain magnetic resonance imaging (MRI) revealed no significant abnormalities. Electroencephalography (EEG) showed frequent runs of rhythmic theta activities with slow background activity. Under the diagnosis of infectious meningoencephalitis, she was empirically treated with antibiotics, antivirals, and anticonvulsants. However, her neurologic deficits such as mental change and motor weakness continued to worsen and she underwent mechanical ventilation and tracheostomy. She started to show involuntary movements on her face, mouth, and tongue (oro-linguo-facial dyskinesia) in 2 weeks after the admission. We started immunotherapy on suspicion of autoimmune encephalitis based on characteristic features such as persistent altered mental status and oro-linguo-facial dyskinesia. Intravenous steroid pulse therapy (methylprednisolone 1 g daily for 5 days) was not effective. However, her mental status started to improve after 5 cycles of plasma exchanges. She showed dramatic improvement in mental status and quadriplegia accordingly with plasmapheresis that she could breathe without a mechanical ventilator, obey to command, and move her limbs voluntarily. Positive results of anti-NMDAR antibodies in her CSF and serum prompted us to explore for underlying tumor.
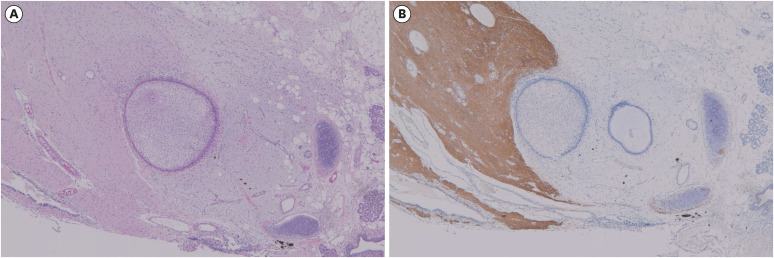
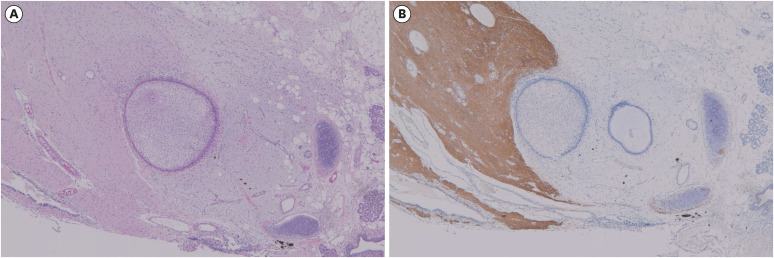
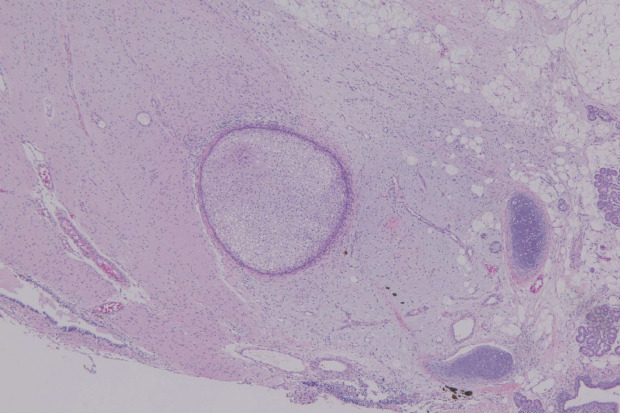
Computed tomography of the thorax, abdomen, and pelvis was performed and revealed a 1 cm sized mass suggestive of MCT arising from the right ovary. Serum tumor markers were within normal limits: CA 125 was 5.0 U/mL and CA 19-9 was 4.6 U/mL. We promptly performed laparoscopic right ovarian cystectomy on March 29, 2017. Intraoperative frozen section analysis and the final pathological diagnosis was MCT (
Fig. 1). Her mental status continued to improve and returned to normal. On postoperative day 8, her tracheostomy tube was removed. She was transferred to the rehabilitation department for mild quadriparesis and ataxia. She was discharged 2 weeks post-operatively with mild memory deficit.
Fig. 1
Pathological examination of the resected ovarian tumor. (A) Histological findings of ovarian mass revealed typical feature of mature cystic teratoma consisting of ectodermal derivatives represented by squamous epithelium with adnexal structures, brain tissue including glia and ependymal tubule, mesodermal derivatives such as cartilage and adipose tissue, and endodermal derivatives such as gastrointestinal epithelium and salivary glands (hematoxylin and eosin stain, ×40). (B) Brain tissue in ovarian teratoma showed strong immunohistochemical reactivity for glial fibrillary acidic protein as evidence of glial tissues (×40).
Ethics statement
The requirement for patient consent was waived by the Institutional Review Board of Dongguk University Ilsan Hospital (DUIH 2020-03-004).
DISCUSSION
Anti-NMDAR encephalitis is the most common form of autoimmune encephalitis, surpassing the frequency of any individual viral cause of encephalitis in patients younger than 30 years old.
6 Anti-NMDAR encephalitis was originally described in 2005 in four women with ovarian teratoma, presenting with acute psychiatric manifestations, cognitive deficits, seizures, and altered level of consciousness.
7 In 2007, Dalmau et al.
2 for the first time identified specific autoantibodies to the NR1 subunit of NMDAR in a cohort of 12 women patients, 11 of whom had ovarian teratoma. This condition was initially considered to be a paraneoplastic syndrome in young women with ovarian teratoma. However, later studies showed many cases in women without an associated tumor, as well as men and children.
58 The largest cohort study of 577 patients with anti-NMDAR encephalitis showed that underlying tumors were found in 38% of patients overall and 46% of female patients; most of them were ovarian teratomas (94%), followed by extraovarian teratomas (2%), and other tumors (4%).
5 Some of the implicated tumors contain nerve tissue or tumor cells expressing the neuronal cell surface or synaptic proteins targeted by the autoantibodies, suggesting that the ectopic expression of these proteins may play a role in triggering the autoimmune response.
9
Epidemiologic studies suggest that anti-NMDAR encephalitis primarily affects children and young adults with median age of 21 years (range, 8 months–85 years), with female predominance (8:2). Up to 58% of young women patients have an ovarian teratoma and its size ranged from 1 to 22 cm with a mean diameter of 6 cm.
45 Ovarian teratomas were preferentially found in women aged 12–45 years.
5 The frequency of associated tumors is lower in men or older adults and various carcinomas such as neuroblastoma, Hodgkin lymphoma, teratoma of the mediastinum, tumors of lung, breast, testicle, ovary, thymus, and pancreas were reported.
510
Interestingly, the frequency of immature teratoma among the patients with anti-NMDAR encephalitis has been reported to be much higher than that in general population. Dalmau et al.
4 observed that 12 out of 21 women patients younger than 19 years had ovarian teratoma and 5 (41.6%) of them had immature teratoma. In a systematic review of 174 cases of anti-NMDAR encephalitis with ovarian teratoma, 21.6% were immature teratoma.
11 In a retrospective study of 252 patients with anti-NMDAR encephalitis, ovarian teratomas were found in 51 patients and 6 (11.8%) of them were immature teratoma.
10 Immature teratomas generally comprise less than 1% of ovarian teratomas, occurring most often in the first two decades of life.
12 Therefore, gynecologists should pay special attention to prevent spillage of cyst contents and peritoneal dissemination of malignant cells during surgery in patients with anti-NMDAR encephalitis.
Approximately 70% of patients have prodromal symptoms such as fever, headache, nausea, vomiting, diarrhea, and flu-like symptoms. Within less than two weeks, they develop psychiatric symptoms such as agitation, hallucinations, delusions, and catatonia. Because the psychiatric symptoms predominate, many patients are often misdiagnosed with acute psychosis. The disease progresses to reduction of speech, memory deficit, orofacial and limb dyskinesias, seizures, decreased level of consciousness, and autonomic instability manifested as excess salivation, hyperthermia, fluctuations of blood pressure, tachycardia, or central hypoventilation that require mechanical ventilation and admission to an intensive care unit.
9 On the other hand, young children frequently present with seizures, abnormal movements, insomnia, and irritability.
The rarity and unawareness of anti-NMDA-receptor encephalitis often lead to delay in diagnosis while more common conditions, such as primary psychiatric disorders and infectious encephalitis, are ruled out first. CSF findings may include moderate lymphocytic pleocytosis, normal or mildly increased protein concentration, and oligoclonal bands. Brain MRI is normal in up to 67% of patients, whereas EEG is abnormal in 90% of patients.
5 The definitive diagnosis is made by the detection of anti-NMDAR antibodies in the blood or CSF; serum testing is less reliable, with false negative results in 14.4% of cases.
13 Once the diagnosis is confirmed in female patients, imaging studies should be performed to search for the presence of ovarian teratoma.
The treatment includes removal of the immunologic trigger (if present), such as ovarian teratoma or other tumor, and immunotherapy.
9 Early tumor removal is critically important in accelerating the improvement of clinical symptoms and reducing the risk of relapse.
41415 First-line immunotherapy includes corticosteroids, intravenous immunoglobulins, and plasmapheresis. Half of patients improve within 4 weeks of first-line therapy. If there is no response to first-line immunotherapy, second-line immunotherapy such as rituximab and cyclophosphamide is used. Approximately 80% of patients have substantial recovery (no or minimal disability) within 2 years, whereas the remainder experience severe disability or death. The mortality rate has been reported to be as high as 7%.
45 Early treatment and no admission to an intensive care unit are reportedly predictors of good outcome.
5 The frequency of relapse within 2 years is 12%. Relapses may imply the recurrence of associated tumor or a tumor that was missed in the first episode.
9
In conclusion, anti-NMDAR encephalitis is a rare but potentially life-threatening autoimmune disorder primarily affecting young women with ovarian teratoma. Gynecologists should be aware that prompt removal of ovarian teratoma is particularly important in achieving a good outcome and periodic surveillance for recurrence of ovarian teratoma is necessary after surgery. Given that the proportion of immature teratoma is relatively high in this condition, intraoperative frozen section analysis should be employed. Although the majority of women with ovarian teratoma will not develop anti-NMDAR encephalitis, those who are managed expectantly without surgery should be informed of the risk of anti-NMDAR encephalitis.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download