The pandemic of coronavirus disease 2019 (COVID-19) is an unprecedented situation that we have never experienced during the last century.1 To cope with this situation in the absence of curative treatment or vaccine, we must turn to universal infection control resources; hand hygiene, environmental control, personal protective equipment (PPE) and quarantine.2 All of these resources are limited and should be used rationally.2 The global supply chains of PPE have collapsed, so that PPE is not available for the person, place and time requiring it the most, while it is overused than needed elsewhere. Public use of PPE should be prudential when long-term reign of COVID-19 pandemic with multiple waves is expected.
Here I purposed to break the myth of a high efficiency particulate air (HEPA) mask for everyone-mask-wearing policy based on previous reports and one simple experiment. How to prevent the spread of common cold and flu are well understood from plentiful resources.3 First, the respiratory viruses are transmitted more commonly via contact than droplet. Secondly, the control measure to reduce spread of respiratory viruses should therefore focus on contact precaution. The single most important protective measure is hand washing, rather than mask wearing. Lastly, the person who wear a face mask to prevent the droplet transmission is the one who have respiratory symptoms.
Because COVID-19 is an infection caused by severe acute respiratory syndrome coronavirus 2, the seventh coronavirus to infect human4 all above mentioned measures are applicable for COVID-19 too. Unlike other respiratory virus infections, COVID-19 has shown many cases with mild or no presenting symptoms, who are highly infectious during asymptomatic period.5
Consequently, new policy has been implemented in the COVID-19 pandemic era, that everyone in public area wears masks not to transfer their germ to others. Long-term implementation of such policy might be difficult without the threat of a looming pandemic. Although proper assessment on the feasibility of this policy has not been made, it appears to settle in as the ‘new normal’ these days. Therefore it is important what type of mask is appropriate for the policy.
The most important factor in choosing mask type will be how well it can contain user-generated droplets. Indeed, HEPA mask filters can collect particles more efficiently than surgical mask filters, only when the mask fits to the face sealing the boundary (Table 1).6 However, the compliance will be affected by how comfortable is mask-wearing,3 especially for a long-term use. HEPA masks such as KF94 or N95 are more uncomfortable, such as demanding tedious cautions (Table 1). Surgical masks are used to protect the operation field from droplets generated from body fluids of users' nasal and oral mucosa by talking or coughing (Table 1).7 Its effectiveness has long been proven in practice, although it is loose-fitting, allowing possible leakage of aerosol droplets through open boundaries.8 Homemade masks made of cotton also have significantly reduced droplet and particle transmission when coughing, but their efficiency is only one third of surgical masks.9 The surgical mask is a pleated rectangular three-layer mask, efficiently preventing wetting to the outer surface by user generated droplets (Fig. 1). HEPA filters are affected by the moisture in the exhaled air10 and it is not recommended to use single mask for longer than 4 hours.2 When the more tightly the HEPA mask fits to the face, droplets will be better contained inside it and will break the mask filter faster.10 If symptomatic patients wear the HEPA mask properly-fitted, they are possibly suffocated by own secretions, otherwise the mask will be unsealed and useless.
In conclusion, a surgical mask is the best type for a person wearing a mask to prevent the droplet transmission, with or without symptoms. A cotton mask rather than a HEPA mask can be the last resort for the person without respiratory symptoms.
References
1. World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Updated 2020. Accessed April 29, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
2. World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19): Interim guidance 27 February 2020. Updated 2020. Accessed April 29, 2020. https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf.
3. Jefferson T, Foxlee R, Del Mar C, Dooley L, Ferroni E, Hewak B, et al. Cochrane review: interventions for the interruption or reduction of the spread of respiratory viruses. Evid Based Child Health. 2008; 3(4):951–1013. PMID: 32313518.

4. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020; 5(4):536–544. PMID: 32123347.
5. Gandhi M, Yokoe DS, Havlir DV. Asymptomatic transmission, the Achilles' heel of current strategies to control COVID-19. N Engl J Med. 2020.

6. Brosseau L, Ann RB. N95 respirators and surgical masks. Updated 2020. Accessed April 29, 2020. https://blogs.cdc.gov/niosh-science-blog/2009/10/14/n95/.
7. Howard RA, Lathrop GW, Powell N. Sterile field contamination from powered air-purifying respirators (PAPRs) versus contamination from surgical masks. Am J Infect Control. 2020; 48(2):153–156. PMID: 31519477.

8. Bae S, Kim MC, Kim JY, Cha HH, Lim JS, Jung J, et al. Effectiveness of surgical and cotton masks in blocking SARS-CoV-2: a controlled comparison in 4 patients. Ann Intern Med. Forthcoming. 2020.

9. Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013; 7(4):413–418. PMID: 24229526.

10. Roberge RJ, Bayer E, Powell JB, Coca A, Roberge MR, Benson SM. Effect of exhaled moisture on breathing resistance of N95 filtering facepiece respirators. Ann Occup Hyg. 2010; 54(6):671–677. PMID: 20522519.
Fig. 1
The inner and outer surfaces of the KF94 mask and surgical mask after inoculating 3 drops of 5 µL of methylene blue dye on the inner surfaces of both masks. The dye diffused from the inner surfaces (A) of the KF94 mask to the extent that it was visible on the outer surface (B), while the dye diffused only in inner layer (C) of the surgical mask, leaving the outer surface (D) dry.
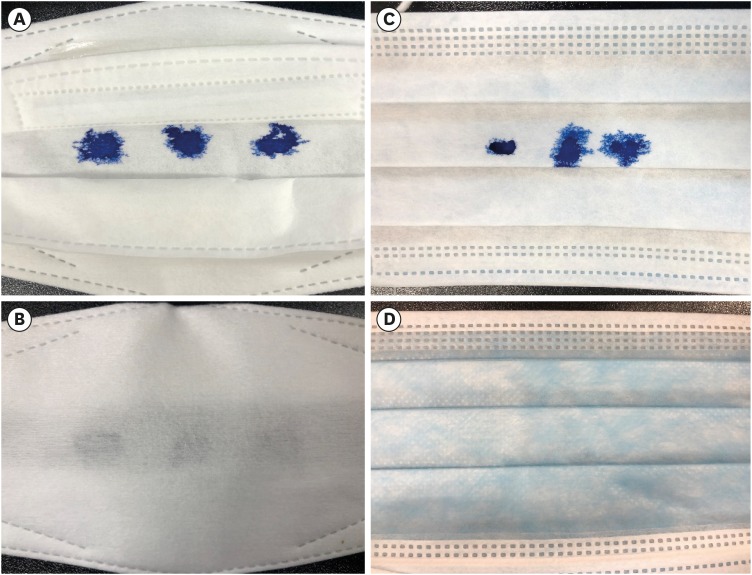
Table 1
Features of surgical mask, HEPA filter mask and cotton mask
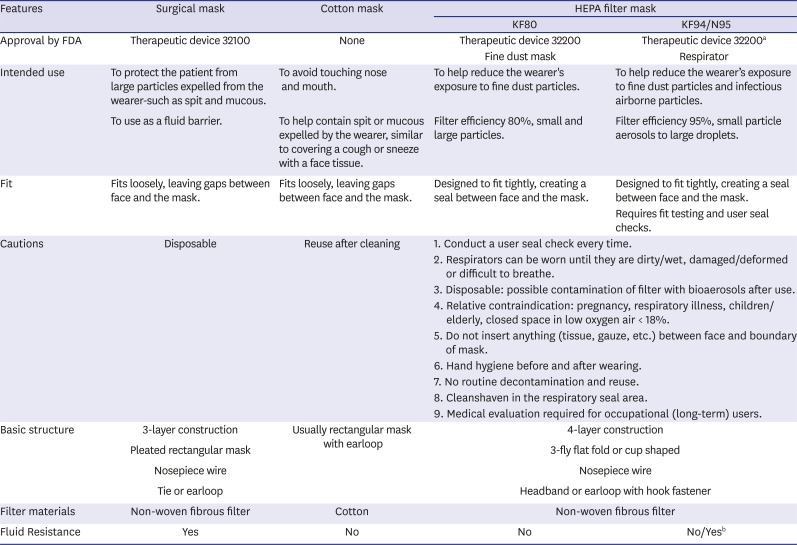
HEPA = high efficiency particulate air, FDA = Ministry of Food and Drugs.
aN95 cleared for use as surgical mask by FDA in US; bThe highest level of fluid resistance is required for surgical N95 respirator.
This table was adapted from Korea Ministry of Food and Drugs information (https://nedrug.mfds.go.kr) and 3M PPE information and guidelines (https://www.3m.com/3M/en_US/medical-us/coronavirus/ppe-information-and-guidance/#protection).




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download