Abstract
Influenza is an epidemical acute respiratory disease caused by viral infection. Several complications in the respiratory tract, such as pneumonia can occur. However, rare but serious neurological complications are also observed. Here, we described the prevalence, characteristics and suggestive pathomechanism of syncope after influenza infection season. Of 2.2% of patients diagnosed as influenza experienced syncope. None of the patients had severe cough, low blood pressure (BP) or dehydration. Patients suffered with frequent dizziness before syncope. Patient with long duration of loss of consciousness was more observed in those with high fever or positive orthostatic BP drop.
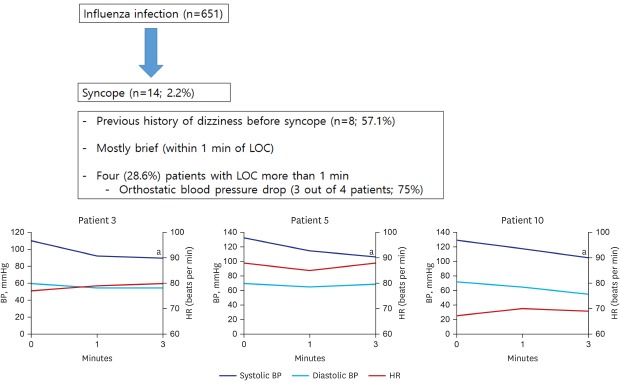
Graphical Abstract
Influenza is an acute respiratory infectious disease that is caused by influenza virus. Local symptoms such as rhinorrhea, cough are usually combined by general symptoms such as high fever and myalgia are common. Symptoms typically start two or three days after exposure to the influenza virus and last less than a week, in other words, self-limited. The most common complication of influenza is pneumonia. Several reports of neurological complications are also reported; meningitis, encephalitis, Guillain-Barré syndrome, acute disseminated encephalomyelitis and myositis.123
Syncope is a loss of consciousness characterized by a sudden onset, short duration and spontaneous recovery, which is caused by decreased blood flow in various situations. Syncope can be observed after viral infection, due to prolonged bed rest, lack of sleep, dehydration with high fever or by direct involvement of cardiac or nervous system. However, the exact mechanism is not clarified. Here, we report patients who experienced syncope after influenza infection confirmed by laboratory tests at a single center during the 2016–2017 influenza season in Korea
This study was performed by a retrospective analysis of patient who visited St. Vincent Hospital, Suwon, Korea from October 2016 to March 2017 and who was diagnosed to have influenza. Influenza was diagnosed based on the confirmatory test using rapid influenza diagnosis test (RIDT; BD Veritor™ System Flu A + B CLIA-waived Device; BD Company, Sparks, MD, USA). This is the most commonly used rapid antigen test for the diagnosis of influenza. Among them, patients who had loss of consciousness were referred to the department of neurology and were consequently registered to our database. Patient's demographics and additional clinical information were obtained from the medical record, retrospectively. Patients' age, gender, previous history of syncope, duration of loss of consciousness, associated symptom, vital signs and concomitant medications information was obtained. All patients received positional blood pressure (BP) test at the outpatient clinic of department of neurology. The electroencephalogram, transthoracic echocardiography and Holter monitoring was selectively performed and the data was analyzed in those who received such tests. The study was approved by the local ethic committee of our center, and informed consent was waived due to the retrospective nature of the study.
The test was based on the protocol of our center for syncope patients; first the patient was lied down for 5 minutes in a comfortable room. After then, the baseline BP and heart rate was measured. The BP and heart rate was repetitively measured by a trained nurse at 1 and 3 minute after standing. Normal response to standing shows slightly increased heart rate and diastolic BP. Abnormal responses are as following: The patient showing more than 20 or 10 mmHg drop in systolic or diastolic BP, respectively, was regarded to have a significant BP drop on standing suggesting orthostatic hypotension due to dysautonomia. Late decrease of BP with bradycardia suggests neuro-cardiogenic syncope. Increase of heart rate more than 30 per minute after standing suggest postural orthostatic tachycardia syndrome.
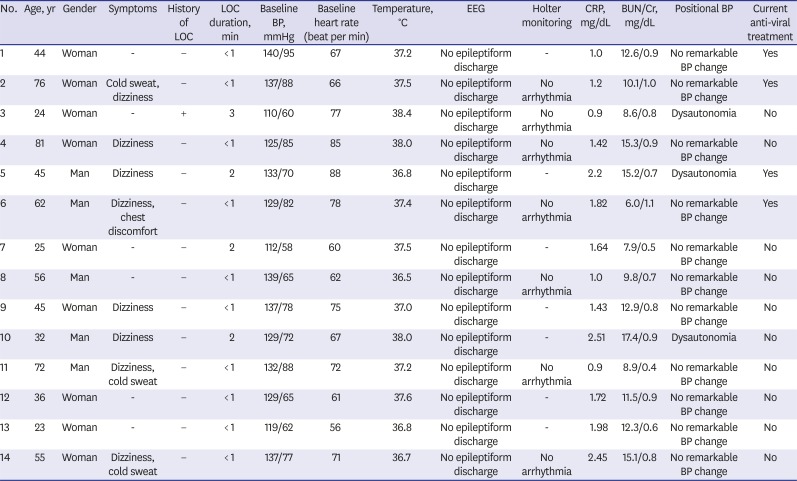
During the study period, 651 patients visited our center due to influenza. Of them, 14 (2.2%) patients experienced syncope (Table 1). The mean age of those patients with syncope after influenza was 48 ± 20 years old, and 9 (64.3%) patients were women. One patient had history of syncope before influenza, who had the longest duration of loss of consciousness (patient number 3). The most common symptoms before loss of consciousness was dizziness (n = 8, 57.1%).
At the time of syncope, only 4 patients had fever and none of the patients showed low BP or dehydration based on laboratory findings including blood urea nitrogen and creatinine level, serum osmolality(> 295 mOsm/kg) and physical examination including presence of thirst or decreased urine volume.4 C-reactive protein (CRP) was mildly elevated in all patients. Four (28.6%) patients were under anti-viral agent. None of the patients show abnormal finding in the electroencephalogram. Seven patients underwent Holter monitoring, but none of the patients showed arrhythmia. Of the enrolled patients, 3 (21.4%) showed abnormal positional BP test results showing significant BP lowering without a significant increase of heart rate and another 3 (21.4%) patients showed high fever over 38°C (Fig. 1).
The duration of loss of consciousness was mostly less than 1 minute (n = 10; 71.4%), but four (28.6%) patients experienced loss of consciousness for more than 1 minute. Those with duration of loss of consciousness more than 1 minute showed abnormal positional BP test results (3 out of 4 patients; 75%) and high fever (3 out of 4 patients; 75%), whereas none of the patients with short duration of loss of consciousness showed positive orthostatic BP lowering or high fever.
Various pathomechanism is involved in syncope occurring after respiratory infarction such as pneumonia or bronchitis in elderly patients. This kind of syncope was explained by loss of appetite, dehydration and cough related syncope. However, none of our patients had severe cough, sign of dehydration or electrolyte imbalance due to poor oral intake. CRP only increased mildly. The baseline BP was not abnormally low. The characteristics were similar with those with general influenza patients. It may be difficult to predict the occurrence of syncope by clinical characteristics.
Neurological complication in viral infectious disease is not uncommon. However, the exact neuropathogenesis is not clarified yet. Hypothetical mechanisms include direct invasion of the virus to the nervous system, toxin mediated or immune mediated response of the nervous system. Some studies reported that peripheral nerve is directly destructed due to immune response in Guillain-Barré syndrome.56 The method how viruses are spread throughout the nervous system differs according to the type of viruses, and some viruses involves specific location in peripheral or central nervous system.78
There are previous reports of influenza virus directly involving the cardiac muscles (myocarditis) and causing cardiogenic syncope.9 Some syncope after influenza infection was caused by arrhythmia (acute arterioventricular conduction blocks or sinus pauses). However, our patients also did not show any cardiac problem or showed arrythmia from the cardiac evaluations. Still influenza virus may also directly involve the nervous system as other viruses. It may cause adrenergic denervation with decreased vascular sympathetic tone and cause post infectious dysautonomia. In our patients with syncope after influenza, more than half of the patients suffered from dizziness before syncope. Furthermore, more than 20% of patients showed a significant orthostatic BP drop, especially in those with longer duration of loss of consciousness.
Our study has several limitations. First, this was a small study performed from a single center, respectively. Second, detailed autonomic function test including peripheral vascular resistance and adrenal function test or head tilt test was not performed, which may have strengthened our hypothesis. Finally, if such autonomic dysfunction occurs, whether it is transient or permanent may be important for long-term prognosis. A prospective study focusing at long-term follow-up data may be needed to verify this issue.
However, we could find that syncope after influenza is not uncommon, and autonomic function may be involved. Patients suffering with dizziness after influenza diagnosis may be vulnerable for syncope, and positional BP measurement may be a convenient method to screen those patients at risk of long duration syncope after influenza infection.
Notes
References
1. Morishima T, Togashi T, Yokota S, Okuno Y, Miyazaki C, Tashiro M, et al. Encephalitis and encephalopathy associated with an influenza epidemic in Japan. Clin Infect Dis. 2002; 35(5):512–517. PMID: 12173123.

2. Maricich SM, Neul JL, Lotze TE, Cazacu AC, Uyeki TM, Demmler GJ, et al. Neurologic complications associated with influenza A in children during the 2003–2004 influenza season in Houston, Texas. Pediatrics. 2004; 114(5):e626–33. PMID: 15520093.

3. Lee YJ, Hwang SK, Kwon S. Acute necrotizing encephalopathy in children: a long way to go. J Korean Med Sci. 2019; 34(19):e143. PMID: 31099193.

4. Hooper L, Abdelhamid A, Attreed NJ, Campbell WW, Channell AM, Chassagne P, et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst Rev. 2015; (4):CD009647. PMID: 25924806.

5. Koski CL. Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy: pathogenesis and treatment. Semin Neurol. 1994; 14(2):123–130. PMID: 7984827.

6. Koski CL. Humoral mechanisms in immune neuropathies. Neurol Clin. 1992; 10(3):629–649. PMID: 1501599.

7. Ludlow M, Kortekaas J, Herden C, Hoffmann B, Tappe D, Trebst C, et al. Neurotropic virus infections as the cause of immediate and delayed neuropathology. Acta Neuropathol. 2016; 131(2):159–184. PMID: 26659576.

8. Bradshaw MJ, Venkatesan A. Herpes simplex virus-1 encephalitis in adults: pathophysiology, diagnosis, and management. Neurotherapeutics. 2016; 13(3):493–508. PMID: 27106239.

9. Sen N, Tanwar S. H1N1 positive case represent as cardiogenic syncope in cardiac emergency department. Int J Sci Res. 2016; 5(4):524–525.
Fig. 1
Abnormal results of positional BP test. A decrease in BP without an increase in heart rate was observed in 3 patients (dysautonomia). Results of positional BP test are classified according to the following criteria: 1) Dysautonomia: more than 20 mmHg or 10 mmHg drop in systolic or diastolic BP, respectively; 2) Neuro-cardiogenic syncope: decrease of BP with bradycardia; and 3) Postural orthostatic tachycardia syndrome: increase of heart rate more than 30 per minute after standing.
BP = blood pressure, HR = heart rate.
aSignificant BP lowering without a significant increase of heart rate.
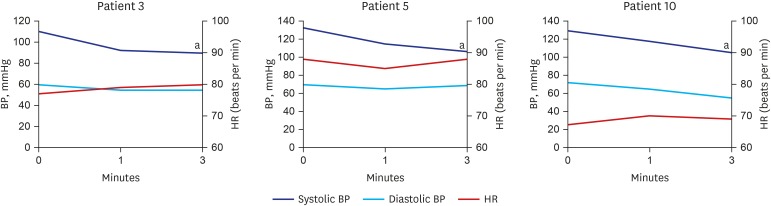
Table 1
Patient characteristics and laboratory findings




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download