Precision medicine seeks to achieve disease prevention and treatment that is optimized to individual characteristics for improved treatment outcomes and quality of life.
123 Rapid development of biomedical technology and significant reductions in the cost of genome sequencing have helped in realizing precision medicine in medical practice.
4 With the announcement of the Precision Medicine Initiative by President Obama in 2015,
15 the US and other countries, including the UK,
6 France,
7 Japan,
8 China,
9 and Korea,
1011 have been working on developing precision medicine as a new medical paradigm to improve the accuracy and efficacy of medicine globally.
As views on and understanding of precision medicine among health professionals might play an important role in the realization of precision medicine, we aimed to investigate awareness, attitudes, and perspectives on precision medicine in Korea via mixed methods study. Initially, we conducted a qualitative study to explore awareness, attitudes, expectations, and concerns regarding precision medicine among health professionals. We then conducted a quantitative study to expand and generalize the qualitative findings.
In the current study, we conducted mixed methods research, which involves collecting, analyzing, and integrating quantitative and qualitative research.
12 We adopted a sequential exploratory design comprising an initial phase of qualitative data collection and analysis, followed by a phase of quantitative data collection and analysis, to explore opinions on precision medicine. In the initial phase, a semi-structured focus group interview (FGI) was conducted. To begin, we sent an invitation letter to the members of the Big Data Research Advisory Committee via e-mail. Those who accepted our invitation helped us identify experts on precision medicine that might want to participate in the study. Through such snowball sampling, we were able to recruit six experts who are working in the areas of preventive medicine, bioinformatics or health data sciences, oncology, and big data research. The FGI was conducted on October 12, 2016. All participants were asked to provide written informed consent prior to participation in the interviews. An FGI guide, which included questions designed to ascertain their perspectives on precision medicine, potential challenges that may impede or delay the realization of precision medicine, and recommendations for the adoption of precision medicine, was used. The interviews were audio recorded and transcribed verbatim. Using a qualitative content analysis approach, the transcripts were analyzed manually by two experts. Thematic analysis was conducted, then the substantial content of the dialogue was extracted, coded, and classified according to the over-reaching themes. During these processes, two experts cross-checked and a third senior researcher finally reviewed coded data confirming similarities in themes.
In the second phase, utilizing our results from the qualitative research, we developed a survey questionnaire and administered a self-reported survey (
Supplementary Materials, only online). Health professionals, including clinicians, nurses, professors, and researchers, were then recruited during the 21st Annual Fall Symposium of the Korean Cancer Association held on November 18, 2016. All participants were asked to provide written informed consent prior to participation in the surveys. A total of 542 health professionals participated in the survey, and 526 completed the entire questionnaire. The questionnaire was developed to assess awareness and attitudes about precision medicine. We conducted descriptive analysis and chi-square tests to compare the distributions of awareness and attitudes about precision medicine according to job type. We further conducted post-hoc analysis for pairwise comparisons with Bonferroni correction of the
p values. We categorized health professions into three different groups: 1) clinicians, 2) researchers, and 3) other health care professionals. All statistical analyses were conducted using SAS software, version 9.3 (SAS Institute, Cary, NC, USA). The study procedure was approved by the Institutional Review Board of the National Cancer Center, Korea (NCC-20160256).
When asked about the main application areas for precision medicine, most participants reported that it can be widely used in patient treatment: “The major use of precision medicine would be in facilitating the use of personalized drugs for each patient.” Some participants showed high expectations for precision medicine. They believed precision medicine could improve the quality of life of cancer patients by avoiding side effects: “In cancer treatment, adverse drug reactions are quite large. However, if we find out a medicine that directly targets an individual disease, we will be able to avoid all unsuccessful attempts to find the right treatment without having to deal with unwanted side effects.” Further, they expected that precision medicine would be reduce medical costs in the long term: “If ineffective treatments are avoided, we can reduce side effects and save on medical costs.” However, some participants also confessed that the concept of precision medicine and its possible practical implications are still unclear, except in the field of cancer.
Most participants professed concerns that precision medicine may be too expensive. They expected that only a few patients would be able to access precision medicine, introducing another source of disparity in health care: “In general, new, targeted drugs that are launched on the market are so highly-priced that patients can hardly afford them, unless their cost is fully covered by health insurance.” “New technology is always costly. Precision medicine will also be provided at a high price, and only a few people who can afford it will benefit from precision medicine.” Also, several participants expressed skepticism regarding the abilities of individual patients to understand precision medicine. They noted that patients often struggle to understand basic medical information: “People do not understand information well enough. They are not ready to learn and understand their genetic profile.” Further, some participants worried about a lack of competence among physicians: “When physicians perform DNA sequencing, they should explain the results to the patients, but some of them do not know about the genome.” Some experts expressed concerns that use of incomplete and unstandardized data may lead confusion for both the physician and patients and thus hinder the implementation of precision medicine. In this context, they pointed out the lack of bioinformaticians and biomedical informatics specialists: “Precision medicine is based on IT infrastructure… There are many IT personnel in Korea, but biotechnicians in the medical field are too scarce in Korea.”
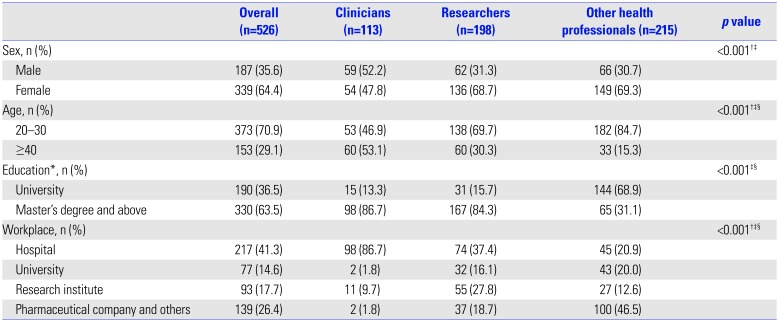
Of the 526 health professions who completed the survey, 187 were male (35.6%) and 339 were female (64.4%), with a mean age of 35.2 years. Health professionals were categorized as clinicians (21.5%), researchers (37.6%), and other health professionals (40.9%) (
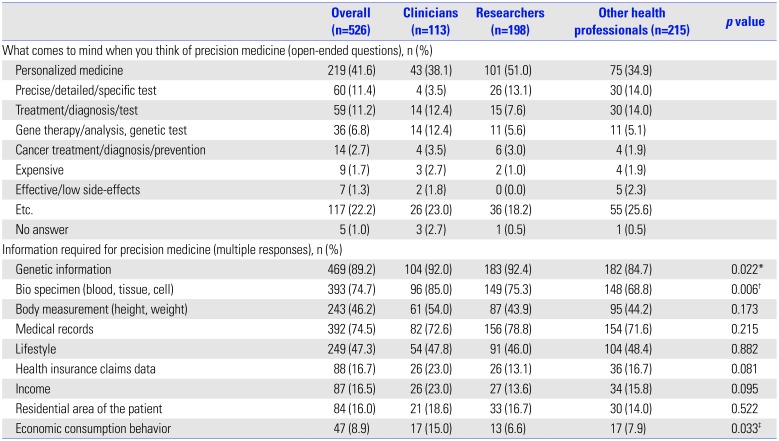
Table 1). Most of the participants described precision medicine as personalized medicine (41.6%); precise/detailed/specific treatment (11.4%); diagnosis testing (11.2%); gene therapy, gene analysis, or genetic testing (6.8%); cancer treatment, cancer diagnosis, or cancer prevention (2.7%); expensive (1.7%); and effective treatment with fewer side-effects (1.3%) (
Table 2). To identify the core information needed to adopt precision medicine into practice, the highest proportion of respondents (89.2%) agreed that genetic information is needed: in particular, researchers were more likely to answer that genetic information is needed than other health professionals (
p=0.041). Also, the respondents indicated that genetic and clinical information is needed more than health behavior information.
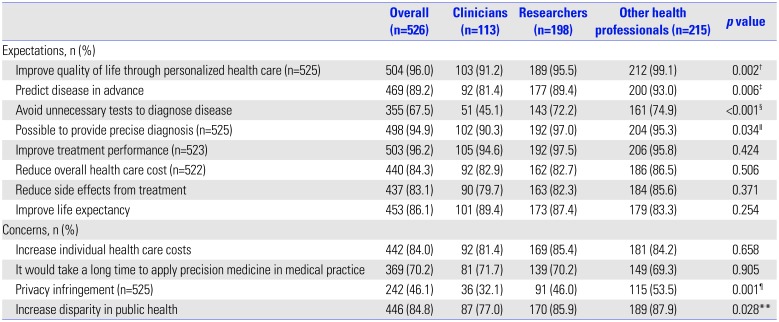
About 96% of the respondents reported that precision medicine will be effective in patient treatment and will provide precise diagnosis (94.9%) (
Table 3). However, overall expectations on precision medicine were the lowest among clinicians, compared with other health care professionals. Specifically, expectations for improving quality of life, predicting disease in-advance, and reducing unnecessary tests with which to diagnose disease, and providing precise diagnosis were significantly lower among clinicians than the other two groups. Regarding concerns related to precision medicine, health professionals were most concerned about increases in disparity and health care costs. However, concerns for infringing upon personal information were relatively low among clinicians and researchers, compared with other health professionals.
Regarding the respondents' willingness to participate as study subjects in precision medicine, more than half of all health professionals (69.9%) reported that they would participate as study subjects (
Table 4). Also, most of the respondents answered that they would be willing to provide their health information for the purposes of treating themselves (90.9%). However, only 62.4% of respondents agreed that they would be willing to provide their health information for the purposes of treating others. Regarding information that they would provide, more than 90% of health professionals agreed to provide their genetic, physical, and health behavior information for the purposes of treating themselves. In addition, the percentage of respondents who agreed to provide medical records was high (85.7%). More researchers agreed to provide medical records than other professionals (
p=0.010). For treating others, only 45.4% of respondents indicated being willing to provide their medical records. In a question about the maximum amount payable for a genetic test, overall, 27% of the respondents answered less than $100 US. Clinicians were willing to pay higher costs than other groups: Among clinicians, 31% answered that they would pay more than $1,000 US. Only 15.7% and 16.9% of researchers and other health professionals, respectively, responded accordingly, and this difference between clinicians and researchers was statistically significant after Bonferroni correction (
p=0.021).
This study was conducted to investigate awareness of and attitudes on precision medicine among health professionals in Korea using mixed methods. In the FGI findings, health professionals indicated that, while precision medicine is needed, ethical and societal challenges may arise in the process of adopting precision medicine in clinical practice, such as training of health workers, educating the general public, providing equal and affordable access thereto, and standardized data use. The participants also recommended allocating specific funding for developing necessary biobanks and data sharing infrastructure currently lacking in Korea. Privacy protection was seen as particularly important when health data are to be shared, and the respondents suggested that public promotion is needed to make people comfortable with sharing their personal health data.
Through our survey, we discovered that many health professionals associated precision medicine with “personalized medicine.” While the terms precision medicine and personalized medicine are used interchangeably, they mean different things. Personalized medicine is an old term referring to individualized medicine, whereas precision medicine means effective approaches based on genetic, environmental, and lifestyle factors.
13 The concept of precision medicine and its possible practical implications remain unclear among health professionals in Korea and need to be addressed.
In the current study, health professionals reported more expectations than concerns for precision medicine, and around 70% of health professionals responded that they would participate as study subjects for precision medicine research. This result is consistent with previous studies that indicated positive attitudes toward precision medicine.
141516 However, in comparison of three different groups of health professionals, we found that clinicians showed lower expectations for precision medicine than researchers and other health professionals. Actually, in the FGI, the interviewees suggested that, most clinicians are not ready to provide genetic testing, interpretation, and personalized treatment to patients in their practice. To increase the number of professionals with the necessary expertise to correctly interpret the genomics profiles of patients, several strategies that involve medical curriculum reform, specialist training, and ongoing physician training must be prepared.
15171819
In addition, the participants in the FGI also highlighted needs for education of the general population to facilitate communication and collaborations between doctor and patient. In precision medicine, patients are encouraged to consult with their healthcare provider to determine their treatment options. However, most patients in Korea are not used to participating in their treatment process. Thus, increasing patient understanding of precision medicine and reshaping the health care system such that patients can participate in their care process are important challenges to implementing precision medicine effectively in Korea.
Our FGI and survey results also showed that developing precision medicine in an equitable way is a major issue. Most health professionals expressed concerns that precision medicine may exacerbate heath disparities if only individuals who are more socioeconomically advantaged are able to benefit from it. This is where health professionals may play an important role by working with decision makers to find ways to implement precision medicine fairly and reasonably. The Scottish Medicines Consortium convened clinicians, health economists, and patient representatives to identify and prioritize new medicines and interventions with good value for the money for patients.
20 Such collaborative efforts may be a good example of how to fairly implement precision medicine into broader clinical practice.
Although this study was the first time health professionals in Korea discussed precision medicine, the study results are not representative of all health professionals' opinions in Korea due to the small number of participants from a specific area (e.g., oncology). Further, many individuals of younger age who are more favorable to new technology participated in the survey. Thus, further research is needed to ensure the representativeness of the results. Also, more work may be needed to investigate how to introduce precision medicine effectively and equitably.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download