Breast cancer treatment with breast-conserving surgery (BCS) requires the establishment of adequate margins to reduce the risk of local recurrence, which can be achieved through several methods. Intraoperative assessment of margin status is commonly performed using frozen section analysis (FSA). However, this technique lacks a standardized sampling method for relatively rounded breast specimens, which is not always practical in a busy unit. Intraoperative specimen mammography has been found useful to identify margin involvement, especially in cases with microcalcification or nonpalpable lesions. Although surgical margin analysis has been acknowledged as a critical component of BCS, the best assessment technique has yet to be determined [
1]. Proponents of specimen mammography report that this radiologic procedure allows surgeons to assess excision adequacy and reduce the number of metachronous re-excisions required to achieve margin-negative resection [
2].
In patients with dense breast, it is especially difficult to define breast lesions using mammography. Nevertheless, intraoperative specimen mammography may be useful in assessing the margin status of visible or nonvisible lesions on preoperative mammography. To date, no studies have evaluated the effectiveness of specimen mammography in dense breasts. The proportion of Korean women with dense breasts is higher than their Western counterpart [
3].
In the present study, we evaluated the influence of preoperative mammography density in specimen mammography analysis. The value of intraoperative specimen mammography in determining the margin status of excised palpable or nonpalpable breast lesions was evaluated. Additionally, the level of agreement between the radiologic and final pathologic interpretations of margin status was analyzed.
Between October 2015 and September 2017, we evaluated 182 patients with breast cancer who underwent intraoperative specimen mammography after BCS at the Ajou University Hospital. Patients with bilateral breast cancer or neoadjuvant chemotherapy or diffuse microcalcifications were excluded. The control group consisted of 84 patients who underwent BCS between January 2014 and December 2014 with the same inclusion criteria and were evaluated for the margin of the frozen section during surgery. We compared the operative time, margin status, and frequency of a second operation for further resection between the 2 groups. The mammogram reports were based on visual analysis by two radiologists. The mammographic findings of breast density were classified according to the following categories, based on the American College of Radiology Breast Imaging Reporting and Data System [
4]. The lesions were pathologically confirmed as ductal carcinoma
in situ (DCIS), invasive ductal carcinoma, lobular carcinoma
in situ, invasive lobular carcinoma, and other malignant neoplasms. Histologic margins were measured as the closest distance between the specimen's edge and cancer cell location. This study was approved by the Ajou University Hospital Institutional Review Board (IRB No. MED-OBS-11-361). For this type of study, informed consent from the patients was not required.
All surgical procedures were performed by 2 specialized breast cancer surgeons. Preoperatively, nonpalpable lesions with microcalcifications were marked by wire-guided localization, which was performed with a hooked wire through an 18-G spinal needle. Following wire insertion, mediolateral oblique view mammography was performed to identify the wire location. One metallic clip was placed on the superior surface, and 2 metallic clips were placed on the lateral margin. Based on the histopathological results obtained from the first surgery, a second operation was performed in patients exhibiting ink on the tumor surface.
Direction-oriented specimens were sent to the mammography unit. Single-image standard compression magnification radiographs were obtained. Specimen mammography was immediately identified, and if mass or calcifications were near the specimen's margins, further resection was performed upon the surgeons' decision.
Statistical analyses were performed using SPSS version 19.0 (IBM Corp., Armonk, USA). Categorical variables were evaluated using the chi-square test. A p-value < 0.05 was considered statistically significant. Linear regression results are presented as the coefficient with confidence intervals and R2 values. Univariate and multivariate analyses were performed using logistic regression.
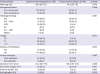
The clinicopathologic characteristics of 182 patients with specimen mammography and 84 patients who underwent FSA after BCS are presented in
Table 1. After confirmation of margin status by two methods, there were no statistical difference in the proportion of further resection (22.0% vs. 25.0%,
p = 0.467).
Two different intraoperative margin assessment methods were compared in terms of mean operative time, narrowest margin from the lesion, and need of a second operation for further resection. The operative time was significantly shorter in the specimen mammography group than that in the FSA group (85.2 vs. 108.4 minutes,
p = 0.026). There were no significant differences in the incidence of extremely close margins (< 1 mm) (
p = 0.421) and second operation (
p = 0.252) between the 2 groups. A significant difference was found between the preoperative mammographic density and possibility of margin assessment, regardless of lesion status. The comparison is shown in
Table 2. All patients' specimens with < 25% density in preoperative mammography allowed lesion identification, whereas lesions were confirmed in only 68.8% of patients with specimens with > 75% density. The results indicated that the difficulty in determining the margin status increases with breast density (
p = 0.003). The correlation between radiological and histological margins is shown in
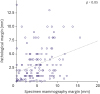
Figure 1. A significant correlation was found between intraoperative specimen mammography and histological nearest distance from lesions (
p < 0.05).
As the use of BCS in oncoplastic surgery expands worldwide, greater efforts are needed to achieve cancer-free margins, which are associated with local recurrence of breast cancer. The reported rates of margin positivity at the initial BCS range from 10% to 27% [
5678]. Furthermore, in the second operation after oncoplastic surgery, it is difficult to find margins with remaining cancer cells, which led several studies to establish the most effective method for intraoperative surgical margin assessment.
Several studies have reported intraoperative methods for pathological evaluation, such as FSA and touch smear and imprint cytology. The re-excision rate of FSA ranges from 3% to 10%, whereas that of imprint cytology ranges from 0% to 33%. Both are significantly lower than that achieved without intraoperative pathological assessment [
910]. However, FSA has several limitations, such as loss of tissue for permanent pathology, technical difficulties caused by a large amount of adipose tissue, significantly longer operative time, and lower accuracy for nonpalpable lesions and/or those containing microcalcifications [
1112]. Several other radio-guided surgery (RGS) techniques have been proposed to improve margin clearance, including radio-guided occult lesion localization (ROLL) and radioactive seed localization (RSL). ROLL involves an intratumoral injection of a radioactive tracer under ultrasound or stereotactic guidance. The surgical excision range can be detected with a handheld gamma probe. RSL uses a small titanium seed containing
125I, which can be detected in mammography. A recent meta-analysis of 7 randomized control trials (RCTs) demonstrated that RGS reduces operative time but increases excised volume. Moreover, no significant differences were found between RGS and wire-guided localization in terms of positive margin and reoperation rate [
13].
Intraoperative specimen radiography can be used in both nonpalpable lesions with calcifications and palpable lesions visible on mammograms. However, few data are available in the literature concerning the accuracy, sensitivity, and specificity of specimen mammography. Several previous RCTs reported a 15.7% positive margin rate and 5.7% reoperation rate [
141516].
The present study found a significant correlation between radiological and histological margins. However, there are several limitations regarding the data about radiological and histological margins. First, the radiological margins was measured as the closest distance between the resection borders on two-dimensional mammography, whereas the histological margin was microscopically measured as the closest distance from the 6-direction surface of the specimen, Therefore, a mismatch might have occurred between the radiological and histological margin status. Second, after specimen compression in the mammography unit, the direction and margin might have been distorted. A previous retrospective study revealed a significant association between specimen radiographs and histological results [
17].
Several factors may affect mammographic breast density, such as age, body mass index, parity, menstrual status, and race [
18]. Asian women more frequently have dense breasts on mammography [
1920]. Therefore, the mammographic sensitivity to breast masses rather than calcification might be lower in Asian women than in Western women due to the high frequency of dense breasts. We evaluated the possibility of identifying the lesion on specimen mammography regardless of the initial mammographic density. Based on our results, margin status was confirmed in 97.1% of lesions with < 50% mammographic density and 85.7% of other lesions. Therefore, mammographic density was found to affect margin status identification on specimen mammography.
Therefore, this study suggests that specimen mammography can be useful in assessing margin status, especially in Asian patients with breast cancer who have denser breasts than Western patients. Moreover, preoperative mammographic density can affect margin assessment on specimen mammography. Further RCTs with larger sample sizes are needed to confirm the significant advantage compared with other methods of intraoperative margin assessment.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download