Abstract
Background and Purpose
Methods
Results
Acknowledgements
Notes
Conflicts of Interest: Linda A. Harris is employed by Alexion Pharmaceuticals, Inc.; Gary Cutter, Haichang Xin, and Inmaculada B. Aban are employed by the University of Alabama at Birmingham, which received financial support from Alexion for this study. Gary Cutter is also President of Pythagoras, Inc., a private consulting company located in Birmingham, AL, USA, and is Professor of Biostatistics at the School of Public Health at the University of Alabama at Birmingham. Gary Cutter has served as a member of consulting or advisory boards (Argenx, Atara Biotherapeutics, Axon, Biogen, BrainStorm Cell Therapeutics, Charleston Laboratories, Click Therapeutics, Genentech, Genzyme, GW Pharmaceuticals, Klein Buendel, MedDay Pharmaceuticals, MedImmune, Novartis, Roche, SciFluor Life Sciences, Somahlution, Teva, TG Therapeutics, and UT Houston), and data and safety monitoring boards [AMO Pharma, BioLineRx, Hisun USA, and Horizon Pharma, Merck, Merck/Pfizer, National Heart, Lung, and Blood Institute (NHLBI; Protocol Review Committee), Neurim Pharmaceuticals, National Institute of Child Health and Human Development (NICHD; OPRU Oversight Committee), Novartis, OPKO Biologics, Orphazyme, Reata Pharmaceuticals, Receptos/Celgene, Sanofi-Aventis, and Teva].
References
Fig. 1
Criteria used for classifying refractory MG. MG-ADL: myasthenia gravis activities of daily living scale.
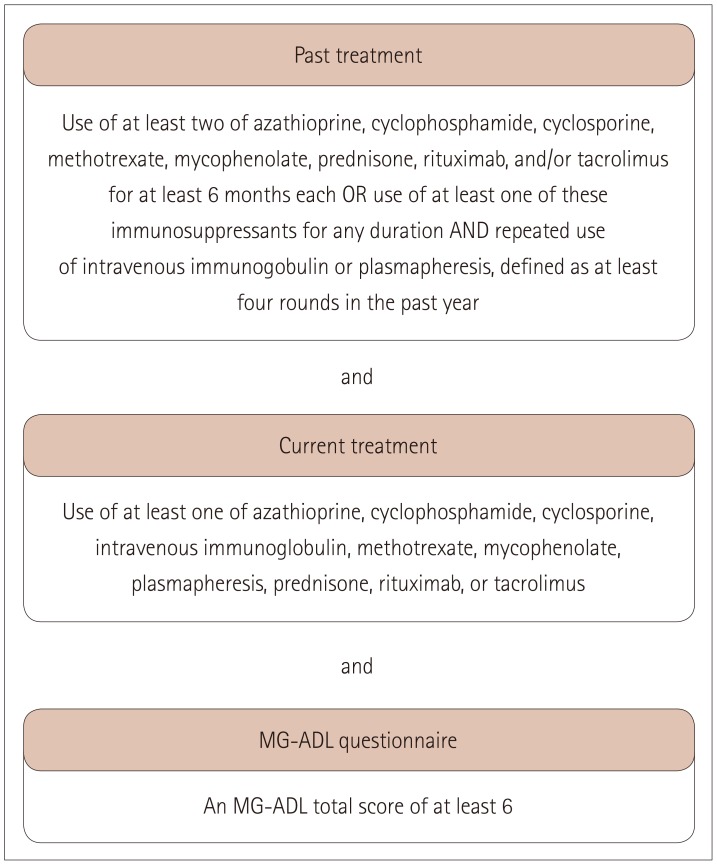
Fig. 2
Flow chart showing selection process for the study sample. MG-ADL: myasthenia gravis activities of daily living scale.
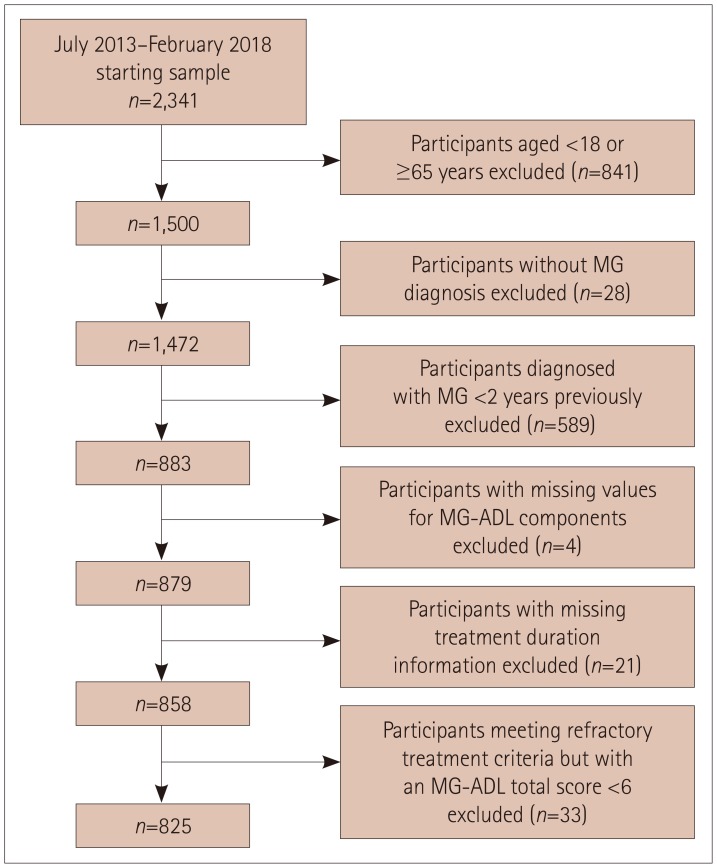
Fig. 3
Exacerbations in and healthcare resource utilization by participants with refractory MG and nonrefractory MG (A) and numbers of exacerbations and ER visits during the 6 months before enrollment in participants with refractory and nonrefractory MG (B). Frequencies of study variables were compared between participants with refractory and nonrefractory MG using χ2 tests for categorical variables and the number of exacerbations, and Fisher's exact test for the number of ER visits. p values are for comparisons between the refractory- and nonrefractory-MG groups, and were calculated after excluding data from participants with unknown/missing data. *During the 6 months before enrollment. ER: emergency room, ICU: intensive care unit, MG: myasthenia gravis.
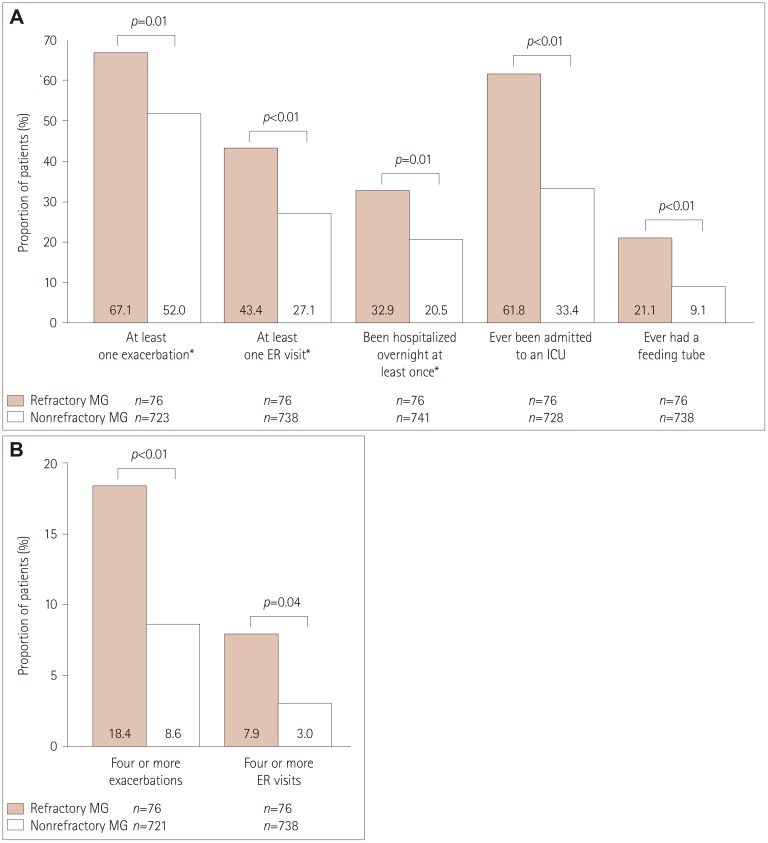
Fig. 4
Unadjusted ordinal logistic model examining the impact of refractory MG on exacerbations and healthcare resource utilization. *During the 6 months before enrollment. Analyses were based on fitting logistic models for binary outcomes except for when analyzing the numbers of exacerbations and ER visits, for which proportional-odds models for ordinal outcomes were fitted. CI: confidence interval, ER: emergency room, ICU: intensive care unit, MG: myasthenia gravis, OR: odds ratio.
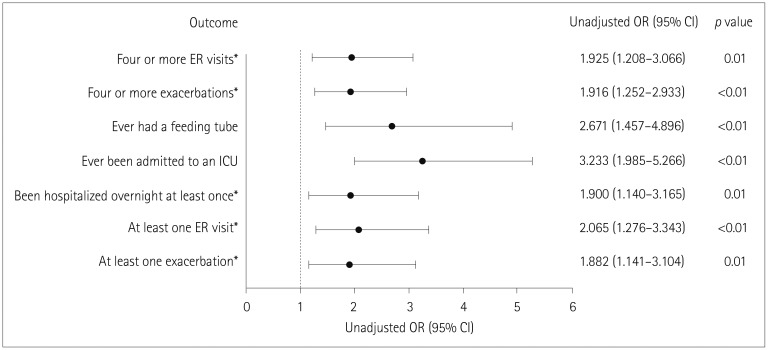
Fig. 5
Exacerbations in and healthcare resource utilization by younger and older female participants with refractory MG (A) and numbers of exacerbations and ER visits during the 6 months before enrollment in younger and older female participants with refractory MG (B). Frequencies of study variables were compared between participants with refractory and nonrefractory MG using χ2 tests for categorical variables and the number of exacerbations, and using Fisher's exact test for the number of ER visits. p values are for comparisons between the refractory- and nonrefractory-MG groups, and were calculated after excluding data from participants with unknown/missing data. *During the 6 months before enrollment. ER: emergency room, ICU: intensive care unit, MG: myasthenia gravis.
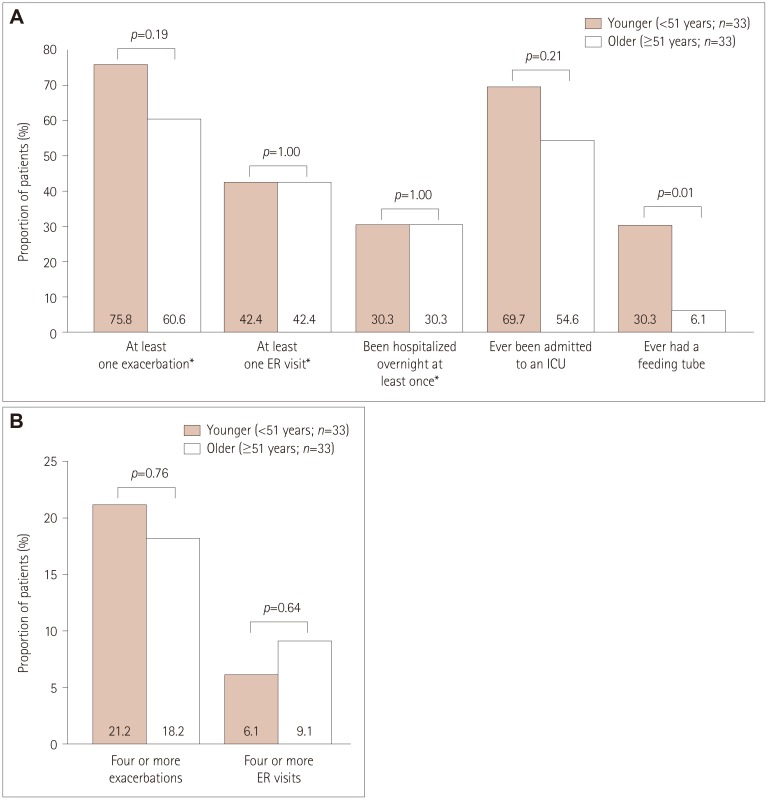
Table 1
Summary of the Myasthenia Gravis Foundation of America patient registry enrollment questions used in the study
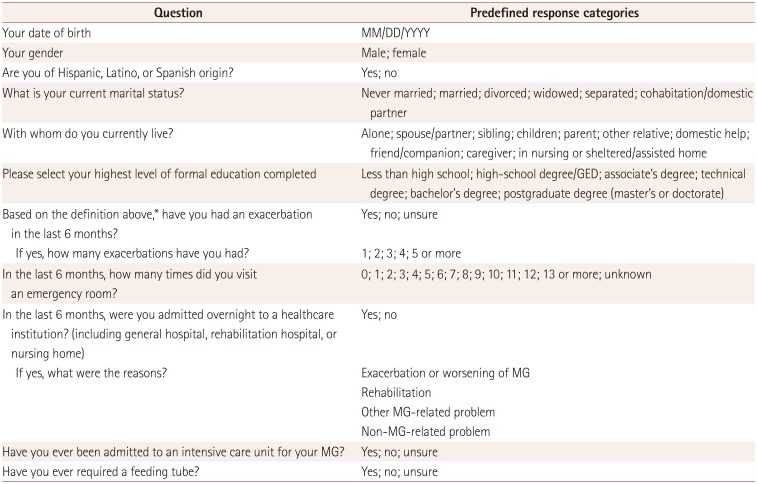
Reproduced with permission from the MGFA.
*Definition of an exacerbation of MG: development of new symptoms or worsening of existing symptoms that lasted >7 days and occurred ≥30 days after the last exacerbation. In an exacerbation, MG symptoms generally worsen over a period of days to weeks. They then improve over several weeks or months, usually with specific treatment. An exacerbation can be associated with several different symptoms that worsen simultaneously.
GED: general equivalency diploma, MG: myasthenia gravis.
Table 2
Participant demographics
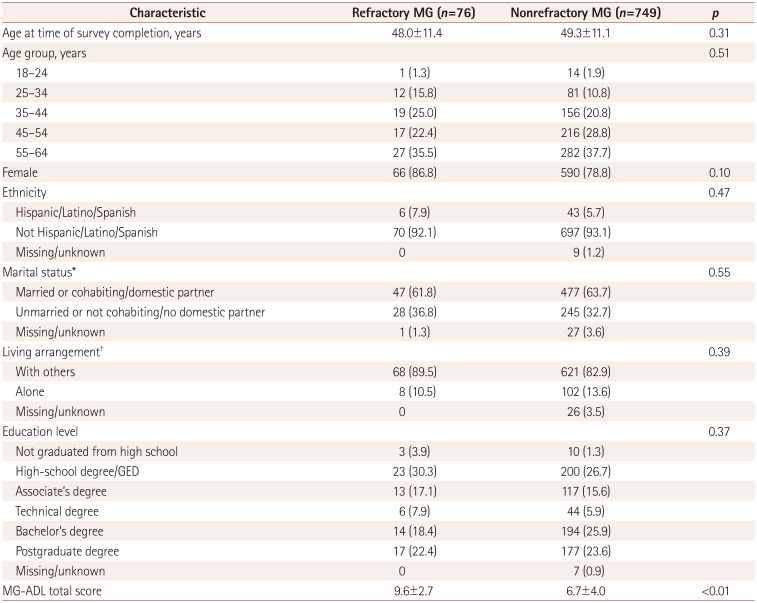
Data are mean±standard deviation or n (%) values. Frequency or mean values of study variables were compared between participants with refractory and nonrefractory MG using χ2 tests for categorical variables and t-tests for continuous variables. p values were calculated after excluding participants with unknown/missing data.
*Six predefined options, which were simplified into married or unmarried, †Ten predefined options, which were simplified into living alone or with others.
GED: general equivalency diploma, MG-ADL: myasthenia gravis activities of daily living scale.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download