1. Harrison LH, Pass MA, Mendelsohn AB, Egri M, Rosenstein NE, Bustamante A, et al. Invasive meningococcal disease in adolescents and young adults. JAMA. 2001; 286(6):694–699.

2. Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. N Engl J Med. 2001; 344(18):1378–1388.

3. Thompson MJ, Ninis N, Perera R, Mayon-White R, Phillips C, Bailey L, et al. Clinical recognition of meningococcal disease in children and adolescents. Lancet. 2006; 367(9508):397–403.

4. Agrawal S, Nadel S. Acute bacterial meningitis in infants and children: epidemiology and management. Paediatr Drugs. 2011; 13(6):385–400.
5. Harrison LH, Trotter CL, Ramsay ME. Global epidemiology of meningococcal disease. Vaccine. 2009; 27:Suppl 2. B51–B63.

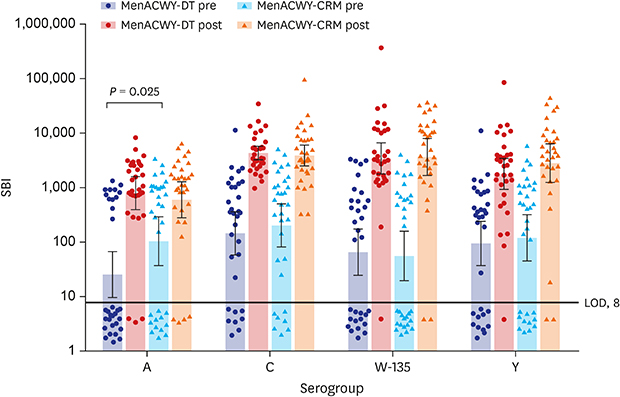
6. Halperin SA, Gupta A, Jeanfreau R, Klein NP, Reisinger K, Walter E, et al. Comparison of the safety and immunogenicity of an investigational and a licensed quadrivalent meningococcal conjugate vaccine in children 2–10 years of age. Vaccine. 2010; 28(50):7865–7872.

7. Jackson LA, Baxter R, Reisinger K, Karsten A, Shah J, Bedell L, et al. Phase III comparison of an investigational quadrivalent meningococcal conjugate vaccine with the licensed meningococcal ACWY conjugate vaccine in adolescents. Clin Infect Dis. 2009; 49(1):e1–10.

8. Halperin SA, Baine Y, Domachowske JB, Aggarwal N, Simon M, Langley JM, et al. Comparison of the safety and immunogenicity of a novel quadrivalent meningococcal ACWY-tetanus toxoid conjugate vaccine and a marketed quadrivalent meningococcal ACWY-diphtheria toxoid conjugate vaccine in healthy individuals 10–25 years of age. J Pediatric Infect Dis Soc. 2014; 3(1):33–42.

9. Heo JY, Choe KW, Yoon CG, Jeong HW, Kim WJ, Cheong HJ. Vaccination policy in Korean armed forces: current status and future challenge. J Korean Med Sci. 2015; 30(4):353–359.

10. World Health Organization. Requirements for meningococcal polysaccharide vaccine (requirements for biological substances No. 23). WHO Expert Committee on Biological Standardization. Twenty-seventh Report. Geneva: Geneva World Health Organization;1976. p. 50–74.
11. Maslanka SE, Gheesling LL, Libutti DE, Donaldson KB, Harakeh HS, Dykes JK, et al. Standardization and a multilaboratory comparison of Neisseria meningitidis serogroup A and C serum bactericidal assays. Clin Diagn Lab Immunol. 1997; 4(2):156–167.
12. Andrews N, Borrow R, Miller E. Validation of serological correlate of protection for meningococcal C conjugate vaccine by using efficacy estimates from postlicensure surveillance in England. Clin Diagn Lab Immunol. 2003; 10(5):780–786.

13. Goldschneider I, Gotschlich EC, Artenstein MS. Human immunity to the meningococcus. I. The role of humoral antibodies. J Exp Med. 1969; 129(6):1307–1326.
14. Lee HJ, Chung MH, Kim WJ, Hong YJ, Choi KM, Lee J, et al. Immunogenicity and safety of a novel quadrivalent meningococcal conjugate vaccine (MenACWY-CRM) in healthy Korean adolescents and adults. Int J Infect Dis. 2014; 28:204–210.

15. Kim DS, Kim MJ, Cha SH, Kim HM, Kim JH, Kim KN, et al. Safety and immunogenicity of a single dose of a quadrivalent meningococcal conjugate vaccine (MenACYW-D): a multicenter, blind-observer, randomized, phase III clinical trial in the Republic of Korea. Int J Infect Dis. 2016; 45:59–64.

16. Reisinger KS, Baxter R, Block SL, Shah J, Bedell L, Dull PM. Quadrivalent meningococcal vaccination of adults: phase III comparison of an investigational conjugate vaccine, MenACWY-CRM, with the licensed vaccine, Menactra. Clin Vaccine Immunol. 2009; 16(12):1810–1815.

17. Gill CJ, Baxter R, Anemona A, Ciavarro G, Dull P. Persistence of immune responses after a single dose of Novartis meningococcal serogroup A, C, W-135 and Y CRM-197 conjugate vaccine (Menveo®) or Menactra® among healthy adolescents. Hum Vaccin. 2010; 6(11):881–887.

18. Sánchez S, Troncoso G, Criado MT, Ferreirós C. In vitro induction of memory-driven responses against Neisseria meningitidis by priming with Neisseria lactamica
. Vaccine. 2002; 20(23-24):2957–2963.
19. Robbins JB, Myerowitz L, Whisnant JK, Argaman M, Schneerson R, Handzel ZT, et al. Enteric bacteria cross-reactive with Neisseria meningitidis groups A and C and Diplococcus pneumoniae types I and III. Infect Immun. 1972; 6(5):651–656.

20. Maslanka SE, Tappero JW, Plikaytis BD, Brumberg RS, Dykes JK, Gheesling LL, et al. Age-dependent Neisseria meningitidis serogroup C class-specific antibody concentrations and bactericidal titers in sera from young children from Montana immunized with a licensed polysaccharide vaccine. Infect Immun. 1998; 66(6):2453–2459.
21. Lieberman JM, Wong VK, Partridge S, Chang SJ, Gheesling LL, Carlone GM, et al. Bivalent A/C meningococcal conjugate vaccine in toddlers: persistence of antibodies and response to a polysaccharide vaccine booster (poster 75). In : Zollinger WD, Frasch CE, Deal CD, editors. Abstracts of the Tenth International Pathogenic Neisseria Conference. Baltimore, MD: Neisseria Research Community;1996. p. 231–232.
22. MacLennan J, Obaro S, Deeks J, Williams D, Pais L, Carlone G, et al. Immune response to revaccination with meningococcal A and C polysaccharides in Gambian children following repeated immunisation during early childhood. Vaccine. 1999; 17(23-24):3086–3093.

23. Borrow R, Lee JS, Vázquez JA, Enwere G, Taha MK, Kamiya H, et al. Meningococcal disease in the Asia-Pacific region: findings and recommendations from the Global Meningococcal Initiative. Vaccine. 2016; 34(48):5855–5862.

24. Bröker M, Dull PM, Rappuoli R, Costantino P. Chemistry of a new investigational quadrivalent meningococcal conjugate vaccine that is immunogenic at all ages. Vaccine. 2009; 27(41):5574–5580.

25. Kim HW, Lee S, Kwon D, Cha J, Ahn JG, Kim KH. Characterization of oropharyngeal carriage isolates of Neisseria meningitidis in healthy Korean adolescents in 2015. J Korean Med Sci. 2017; 32(7):1111–1117.
26. Durey A, Bae SM, Lee HJ, Nah SY, Kim M, Baek JH, et al. Carriage rates and serogroups of Neisseria meningitidis among freshmen in a University dormitory in Korea. Yonsei Med J. 2012; 53(4):742–747.
27. Pobre K, Tashani M, Ridda I, Rashid H, Wong M, Booy R. Carrier priming or suppression: understanding carrier priming enhancement of anti-polysaccharide antibody response to conjugate vaccines. Vaccine. 2014; 32(13):1423–1430.

28. Burrage M, Robinson A, Borrow R, Andrews N, Southern J, Findlow J, et al. Effect of vaccination with carrier protein on response to meningococcal C conjugate vaccines and value of different immunoassays as predictors of protection. Infect Immun. 2002; 70(9):4946–4954.

29. Arguedas A, Soley C, Loaiza C, Rincon G, Guevara S, Perez A, et al. Safety and immunogenicity of one dose of MenACWY-CRM, an investigational quadrivalent meningococcal glycoconjugate vaccine, when administered to adolescents concomitantly or sequentially with Tdap and HPV vaccines. Vaccine. 2010; 28(18):3171–3179.

30. Gasparini R, Conversano M, Bona G, Gabutti G, Anemona A, Dull PM, et al. Randomized trial on the safety, tolerability, and immunogenicity of MenACWY-CRM, an investigational quadrivalent meningococcal glycoconjugate vaccine, administered concomitantly with a combined tetanus, reduced diphtheria, and acellular pertussis vaccine in adolescents and young adults. Clin Vaccine Immunol. 2010; 17(4):537–544.

31. Kim HW, Park IH, You S, Yu HT, Oh IS, Sung PS, et al. Immunogenicity of MenACWY-CRM in Korean military recruits: influence of tetanus-diphtheria toxoid vaccination on the vaccine response to MenACWY-CRM. Yonsei Med J. 2016; 57(6):1511–1516.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download