1. Antonicelli L, Bucca C, Neri M, De Benedetto F, Sabbatani P, Bonifazi F, et al. Asthma severity and medical resource utilisation. Eur Respir J. 2004; 23(5):723–729.


2. Zeiger RS, Schatz M, Dalal AA, Qian L, Chen W, Ngor EW, et al. Utilization and costs of severe uncontrolled asthma in a managed-care setting. J Allergy Clin Immunol Pract. 2016; 4(1):120–129.e3.


3. Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014; 371(13):1198–1207.


4. Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, Bardin P, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015; 3(5):355–366.


5. Busse W, Corren J, Lanier BQ, McAlary M, Fowler-Taylor A, Cioppa GD, et al. Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol. 2001; 108(2):184–190.


6. Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Fontana, WI: Global Initiative for Asthma;2018.
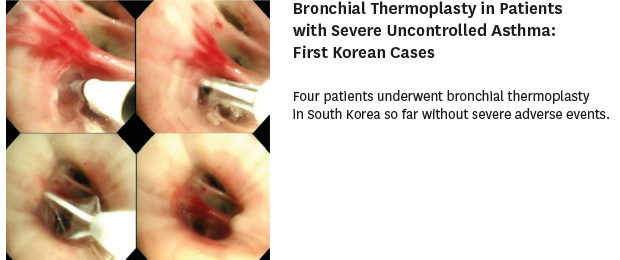
7. Cox G, Miller JD, McWilliams A, Fitzgerald JM, Lam S. Bronchial thermoplasty for asthma. Am J Respir Crit Care Med. 2006; 173(9):965–969.


8. Cox G, Thomson NC, Rubin AS, Niven RM, Corris PA, Siersted HC, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med. 2007; 356(13):1327–1337.


9. Pavord ID, Cox G, Thomson NC, Rubin AS, Corris PA, Niven RM, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med. 2007; 176(12):1185–1191.


10. Castro M, Rubin AS, Laviolette M, Fiterman J, De Andrade Lima M, Shah PL, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med. 2010; 181(2):116–124.
12. Dombret MC, Alagha K, Boulet LP, Brillet PY, Joos G, Laviolette M, et al. Bronchial thermoplasty: a new therapeutic option for the treatment of severe, uncontrolled asthma in adults. Eur Respir Rev. 2014; 23(134):510–518.


13. Han X, Zhang S, Zhao W, Wei D, Wang Y, Hogarth DK, et al. A successful bronchial thermoplasty procedure in a “very severe” asthma patient with rare complications: a case report. J Asthma. 2018; 1–4.

14. Benedetti PA, López JJ, Bezant IF, Flores ML, Ramos AO, Casado MS, et al. Bronchial thermoplasty in patients with very severe asthma: safety and clinical outcomes. Eur Respir J. 2016; 48:PA3839.

15. Langton D, Ing A, Fielding D, Wang W, Plummer V, Thien F. Bronchodilator responsiveness as a predictor of success for bronchial thermoplasty. Respirology. 2019; 24(1):63–67.


16. Wechsler ME, Laviolette M, Rubin AS, Fiterman J, Lapa e Silva JR, Shah PL, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Allergy Clin Immunol. 2013; 132(6):1295–1302.


18. Torrego A, Solà I, Munoz AM, Roqué I Figuls M, Yepes-Nuñez JJ, Alonso-Coello P, et al. Bronchial thermoplasty for moderate or severe persistent asthma in adults. Cochrane Database Syst Rev. 2014; (3):CD009910.






 Citation
Citation Print
Print



 XML Download
XML Download