Abstract
Purpose
Authors attempt to analyze the characteristics of combined ulnar styloid fracture (USF) and its influence on more than a year clinical outcome in patients who underwent conservative treatment for stable distal radius fracture (DRF).
Methods
The retrospective study is a case-control study between January 2011 and December 2016. Through the exclusion process, 175 patients were included (non-USF: 106 patients with 45.4 months mean follow-up, USF: 69 patients with 48.1 months mean follow-up). All patients were treated conservatively under acceptable distal radius alignment. The USF was divided into fracture locations. The visual analogue scale (VAS), Mayo wrist score, and Quick Disabilities of the Arm, Shoulder and Hand (DASH) outcome were assessed at the final follow-up at least more than 1 year.
Results
Between two groups depending on USF, there was none of radiologic outcome difference including union time, rdial height, radial tilting, and volar tilting. The mean VAS score at the final follow-up was 1.1 in both groups. The Mayo wrist score and DASH score for functional performance were 92.3 and 7.5, respectively, in patients with DRF alone, and 90.0 and 9.2, respectively, in those with combined USF, without statistical difference. The functional outcomes also did not present significant differences, depending on USF location and whether or not union.
Distal radius fracture (DRF) is one of the most common fractures that orthopedic surgeons encounter clinically, particularly in patients with osteoporosis12. Due to its pathologic mechanism, the incidence of ulnar styloid fracture (USF) accounts for approximately ≥50%1345.
There has been a controversy regarding the separate management for USF simultaneously while surgically treating DRFs, and past comparative studies focused considerably more on surgically treated patients67. Studies are rare concerning the long-term outcome of patients with minimally displaced DRFs with USF treated conservatively8. When surgeons decide conservative management in DRF, USF does not influence on treatment mainstream9. Besides, a majority of hand surgeons does not think that it is important, they guess it only has a small impact afterward. Therefore, it is still unclear whether USF combined with USF accompanied with DRF affects the clinical outcome and whether surgical treatment is necessary for USF.
Authors attempt to statistically analyze the characteristics of combined USF and its influence on more than a year clinical outcome in patients who underwent conservative treatment for stable DRF.
The hypothesis of this study was whether DRF accompanies USFs would not be imperative in the consideration for deciding surgical intervention if clinicians decided to take conservative treatment on DRF.
The present study is a retrospective case-control study conducted under the official approval of the Institutional Review Board (IRB No. CHAMC 2018-08-030). Between January 2011 and December 2016, we found 1,789 patients diagnosed with DRF who were treated in CHA Bundang Medical Center. We excluded patients with surgical management (n=608), age <20 years (n=319), age >65 years (n=401), conservative management despite unacceptable alignment (n=21), other combined multiple fractures (n=9), refracture (n=5) or occult fracture (n=12), and lost to follow-up (n=239). Finally, 175 patients treated conservatively were included.
The palmar tilt in any degree more than neutral was perceived as the acceptable range. Radial shortening of no more than 2 mm was treated conservatively. Cases in which radial inclination, measured from lunate facet to radial styloid, was more than 10° were also classified as conservatively treatable. Intraarticular step off was only allowed to be <2 mm for conservative treatment10. Fracture types depending on AO/OTA (Orthopaedic Trauma Association) classification were also identified from initial radiograms, X-ray, and computed tomography (CT) by two orthopedic surgeons.
In all patients, the follow-up period should be more than a year. The mean follow-up periods were 48.1±20.4 and 45.4±19.2 months in the patient group with and without USF, respectively.
Closed reduction was selectively performed to obtain an acceptable range of each inclusion criterion. Under acceptable alignment, short arm cast between 4 and 6 weeks, regardless of USF, was followed by range of motion exercise. Serial X-ray was performed during conservative management. In 63 patients (63/175, 36.0%), CT was initially performed to further identify USF. The USF was divided into three types, type I of distal to base fracture, type II of base fracture, and type III of proximally located fracture from styloid base (Table 1). More than 1 mm displacement of USF fragment was regarded as displacement group.
We assessed union time during follow-up period through plain radiographs. At the last follow-up, authors measured radial height, volar tilt, radial inclination, and arthritic changes. The visual analogue scale (VAS), Mayo wrist score, and Quick Disabilities of the Arm, Shoulder and Hand (DASH) outcome were assessed at the final follow-up of at least >1 year.
The Pearson chi-squared test or Fisher exact test for categorical variables, and the Student t-test or Kruskal-Wallis test for continuous variables were used. A p-value less than 0.05 was considered statistically significant. Statistical evaluation was conducted using software R (ver. 3.1.0, Comprehensive R Archive Network, GNU General Public License).
In patients with USF combined with DRF (44/69, 63.8%), closed reduction to achieve acceptable alignment was performed more than in patients with DRF alone (32/106, 30.2%). With regard to DRF, all patients achieved radiologic union with acceptable alignment between 4 and 15 weeks with conservative management.
DRF fracture union during follow-up period was detected in mean 7.34 weeks of only DRF and 7.66 weeks of DRF with USF groups. At the last follow-up, radial height, volar tilt, and radial inclination did not presented statistical differences between two groups (Table 2). There was no evidence of post-traumatic arthritis on last follow-up radiographs in all patients.
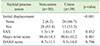
The mean VAS score at the final follow-up was 1.1±1.7 and 1.1±1.8 in the DRF only and DRF with USF groups, respectively. The Mayo wrist score and DASH score for functional performance were 92.3±9.8 and 7.5±12.3, respectively, in patients with DRF alone, and 90.0±12.2 and 9.2±12.7, respectively, in patients with combined USF, without statistical difference (Table 2).
We divided the patients with USF depending on fracture location.
Of 69 patients, 41 patients initially presented with USF fragment >1 mm displacement (59.4%).
The functional outcomes, VAS, Mayo wrist score, and DASH score did not also present significant differences depending on USF location (Table 3).
Furthermore, authors compared outcomes depending on styloid process union. Of 69 patients, 39 patients (56.5%) achieved union during the follow-up period. Patients of union presented slightly better outcomes than non-union patients, without significant differences (Table 4).
The main finding of the present study was that the conservative treatment on concomitant USF in patients with DRF, age between 20 and 65 years with minimal and acceptable degree of displacement, has shown favorable clinical results in consecutive clinical data collection via out-patient ward follow-up of more than a year. We excluded immature osseous structure of age younger than 20 years. Although DRF more commonly occurs in elderly patients with or without osteoporosis, we excluded those older than 65 years because elderly patients could be relatively satisfied with their overall condition regardless of radiographic outcomes11.
To the best of our knowledge, only one comparative study was conducted regarding the effect of USF on outcomes after conservative treatment of the distal radius8. Turan et al.8 reported mean Quick-DASH score of intact USF (16.8), ulnar styloid non-union (19.5), and healed USF (19.4) without significant difference, which were slightly higher than our study. Although they only included 56 patients, they concluded that USF should not be the focus during initial treatment of DRF, which coincided with our reports.
In patients with USF, 63.8% required closed reduction to achieve acceptable alignment for DRF with significant difference. Compared with patients without fracture, combined USF can occur with higher energy with more change of displacement. However, once it is reduced until acceptable alignment, the result was similar in patients who did not undergo close reduction.
Furthermore, we did not find functional outcome differences based on USF location.
In previous researches, there were several implications of USF, including triangular fibrocartilage complex (TFCC) tear, chronic instability of distal radioulnar joint (DRUJ), extensor carpi ulnaris (ECU) tendon irritation, and ulnar nerve irritation5121314151617. Any legions can elicit wrist ulnar side pain and affect functional outcomes.
Ulnar styloid avulsion may result in DRUJ instability due to TFCC disruption, the principal stabilizer of the DRUJ1618. Especially, some authors also mentioned potential DRUJ instability when displaced fracture involves the ulnar styloid base or fovea, because TFCC has insertion on it56. Moreover, pain could be chronic, which means subjective satisfaction would be poor. However, whether USF affects the function of wrist and trigger chronic instability of DRUJ is still debatable.
Richards et al.19 evaluated the soft tissue injuries associated with DRFs by using arthroscopy. They found no correlation between USFs and TFCC injuries.
Kazemian et al.20 used external fixation to treat DRF with USF, proving that USF does not influence DRUJ instability. Furthermore, Lindau et al.21 reported that DRUJ problem after DRF has poor prognosis, but its instability was not correlated with the presence of USF. Finally, DRUJ problem might develop in DRF regardless of USF.
In previous studies, 17% to 54% of union rate was reported1. Despite high rate of nonunion, only a few cases were reported to be symptomatic in previous studies2223. In our study, the USFs were united in 56.5% (39 of 69 patients), which was a relatively high union rate compared with previous reports22. Besides, nonunion did not present significant differences although with slight value differences.
Although there were only a few cases, some patients with non-united USF occasionally complain on nonunion site associated with ECU tendinitis due to irritation and impingement, which can be treated with simple excision of the fragment1516.
Nerve irritation or damage also can be imperative consideration after DRFs with or without USF. Clarke and Spencer17 reported clinical and anatomical studies on patients with DRF with ulnar nerve palsy, resulting from dense scar tissue formation around nerve. The reasons of scar formation were fracture with open wound and dislocated radioulnar joint, which means high-energy injury17. However, no statistically relevant report suggested that USF was associated with the functional outcome. Moreover, based on meta-analysis, Wijffels et al.1 claimed that the result of USF union or nonunion does not seem to influence the functional outcome, and the ulnar styloid should not be the focus during initial treatment.
Despite ongoing debates, most of the studies have documented that USF did not affect outcomes and that the presence, displacement, or level of USF did not have any effect on the outcome68122425.
The present study has several limitations. First, our study contained only 175 cases of DRF with or without USF. With larger sample sizes, statistical differences might be generated. However, it is difficult to infer clinical implications because the two groups presented only a slight difference in functional results. Besides, USF can affect the patients with follow-up of less than 1 year and present significant difference in the short-term follow-up.
Nevertheless, the authors attempted to identify the influence of USF in conservatively treatable DRF, acceptable range from previous literature, with more than 1 year follow-up and relatively medium sample sizes.
Figures and Tables
References
1. Wijffels MM, Keizer J, Buijze GA, et al. Ulnar styloid process nonunion and outcome in patients with a distal radius fracture: a meta-analysis of comparative clinical trials. Injury. 2014; 45:1889–1895.


2. Nakamura T, Iwamoto T, Matsumura N, Sato K, Toyama Y. Radiographic and arthroscopic assessment of DRUJ instability due to foveal avulsion of the radioulnar ligament in distal radius fractures. J Wrist Surg. 2014; 3:12–17.


3. Gogna P, Selhi HS, Mohindra M, Singla R, Thora A, Yamin M. Ulnar styloid fracture in distal radius fractures managed with volar locking plates: to fix or not? J Hand Microsurg. 2014; 6:53–58.



4. Kim JK, Yun YH, Kim DJ, Yun GU. Comparison of united and nonunited fractures of the ulnar styloid following volar-plate fixation of distal radius fractures. Injury. 2011; 42:371–375.


5. Sammer DM, Chung KC. Management of the distal radioulnar joint and ulnar styloid fracture. Hand Clin. 2012; 28:199–206.


6. Kim JK, Kim JO, Koh YD. Management of distal ulnar fracture combined with distal radius fracture. J Hand Surg Asian Pac Vol. 2016; 21:155–160.


7. Sawada H, Shinohara T, Natsume T, Hirata H. Clinical effects of internal fixation for ulnar styloid fractures associated with distal radius fractures: a matched case-control study. J Orthop Sci. 2016; 21:745–748.


8. Turan S, Çankaya D, Yılmaz S, Karakuş D, Dündar A, Özdemir G. Effect of ulnar styloid fracture on outcomes after conservative treatment of distal radius fracture. Eklem Hastalik Cerrahisi. 2016; 27:87–93.


9. Wolfe SW. Distal radius fractures. In : Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS, editors. Green's operative hand surgery. 7th ed. Philadelphia, PA: Elsevier;2017. p. 516–587.
10. Ruch DS, McQueen MM. Distal radius and ulna fractures. In : Rockwood CA, Green DP, Bucholz RW, MacQueen M, editors. Rockwood and Green's fractures in adults. 7th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins;2010. p. 829–880.
11. Chen Y, Chen X, Li Z, Yan H, Zhou F, Gao W. Safety and efficacy of operative versus nonsurgical management of distal radius fractures in elderly patients: a systematic review and meta-analysis. J Hand Surg Am. 2016; 41:404–413.


12. af Ekenstam F, Jakobsson OP, Wadin K. Repair of the triangular ligament in Colles' fracture. No effect in a prospective randomized study. Acta Orthop Scand. 1989; 60:393–396.

13. Kim JK, Kim DJ, Yun Y. Natural history and factors associated with ulnar-sided wrist pain in distal radial fractures treated by plate fixation. J Hand Surg Eur Vol. 2016; 41:727–731.


14. Ploegmakers J, The B, Wang A, Brutty M, Ackland T. Supination and pronation strength deficits persist at 2-4 years after treatment of distal radius fractures. Hand Surg. 2015; 20:430–434.


15. Hauck RM, Skahen J 3rd, Palmer AK. Classification and treatment of ulnar styloid nonunion. J Hand Surg Am. 1996; 21:418–422.


16. May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am. 2002; 27:965–971.


17. Clarke AC, Spencer RF. Ulnar nerve palsy following fractures of the distal radius: clinical and anatomical studies. J Hand Surg Br. 1991; 16:438–440.


18. Haugstvedt JR, Berger RA, Nakamura T, Neale P, Berglund L, An KN. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am. 2006; 31:445–451.


19. Richards RS, Bennett JD, Roth JH, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997; 22:772–776.


20. Kazemian GH, Bakhshi H, Lilley M, et al. DRUJ instability after distal radius fracture: a comparison between cases with and without ulnar styloid fracture. Int J Surg. 2011; 9:648–651.


21. Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000; (376):229–235.

22. Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res. 1996; (327):135–146.

23. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg Am. 1991; 16:375–384.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download