Dear Editor,
Prostate-specific antigen (PSA) is secreted by the prostate gland, and elevated serum PSA levels are observed in patients with prostate cancer, benign prostatic hyperplasia, and prostatitis [1]. PSA is currently used for diagnosis or case identification, prognosis with other factors, detecting recurrence, and monitoring therapy, but not for screening or early detection, as recommended by the National Academy of Clinical Biochemistry (NACB) [2].
PSA levels have been used for risk stratification. The clinically relevant PSA cut-off level, 4 ng/mL, is most commonly used [1]. After initiation of hormonal therapy, achieving a PSA level of <4 ng/mL is associated with significantly longer remission, and maintaining a PSA level <4 ng/mL after three months of therapy is predictive of survival [3].
Different PSA assays produce different results with the same patient sample [4]. This retrospective multicenter study compared serum PSA levels using four automated chemiluminescent immunoassay analyzers that used different calibration materials: Immulite 2000 XPi (Siemens Healthcare Diagnostics Inc., Tarrytown, NY, USA), UniCel DxI 800 (Beckman Coulter, Brea, CA, USA), ADVIA Centaur XPT (Siemens Healthcare Diagnostics Inc.), and ARCHITECT i2000SR (Abbott Diagnostics, Abbott Park, IL, USA). It was performed in three different affiliated hospitals of The Catholic University of Korea: St. Paul's Hospital, Seoul; St. Mary's Hospital, Uijeongbu; and St. Vincent's Hospital, Suwon. This study was approved by the Institutional Review Board of The Catholic University of Korea.
We used 120 serum samples with PSA levels of 0.04–100 ng/mL, as evaluated by Immulite 2000Xpi. Samples were stored at −70℃ and subsequently thawed for analysis with the other analyzers. We summarized results as mean±SD and performed Pearson correlation analysis and Passing-Bablok regression between analyzers. In addition, Bland-Altman analysis was performed. MedCalc 15.0 (MedCalc Software, Ostend, Belgium) was used for all analyses.
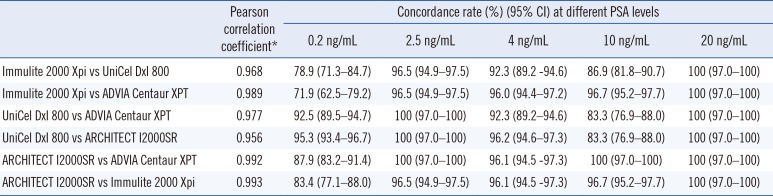
Immulite 2000 XPi showed the lowest mean PSA levels (6.00± 13.68 ng/mL), while UniCel DxI 800 had the highest (6.81± 15.79 ng/mL). The concordance rates using cut-off levels of 0.2, 2.5, 4.0, 10.0, and 20.0 ng/mL are summarized in Table 1. Concordance rates at 0.2 ng/mL were generally low, but those for 2.5 ng/mL were favorable (96.5–100%). Concordance rates for 4.0 ng/mL were also favorable (92.3–96.1%), but those for 10 ng/mL ranged from 83.3% to 100%. At 20 ng/mL, all four analyzers showed 100% concordance rates. Pearson correlation coefficient ranged from 0.956 to 0.993 (Table 1). Comparative analysis of PSA levels revealed strong correlations between each analyzer. However, the PSA levels obtained from Immulite 2000 Xpi were generally lower than those from UniCel DxI (slope=0.842, intercept=−0.0187; Fig. 1). Bland-Altman analysis showed that this bias was mainly due to underestimation of PSA levels >10 ng/mL with Immulite 2000 XPi compared with the other three analyzers.
A PSA level of <0.2 ng/mL is significantly associated with disease-free survival after radiotherapy for prostate cancer [5]. A PSA level <4 ng/mL is associated with significantly longer remission following first-line hormonal therapy [3]. A PSA cut-off of 2.5 ng/mL has a prognostic association with disease-free survival after radiotherapy [6]. A PSA level <4.0 ng/mL following first-line hormonal therapy is a favorable prognosis marker, in conjunction with tumor stage (<T2b) and Gleason score (<6) for salvage therapy [67]. Boccon-Gibod et al. [3] have proposed that the application of a PSA cut-off of 4–10 ng/mL over a minimum period of eight weeks would be useful following first/second-line hormonal therapy. Moreover, a PSA level of 20 ng/mL could be used to define recurrences following treatment [8].
Our results showed that all four analyzers equally detected one sample with a PSA level >100 ng/mL. Patients with a PSA level >100 ng/mL have significantly lower five- and 10-year overall survival than patients with a diagnostic PSA level of 20–100 ng/mL or <20 ng/mL [9]. Gontero et al. [10] have reported that prostate cancer patients with PSA levels >100 ng/mL have a very high risk of bone metastatic disease.
In summary, the comparison results of these four analyzers are quite satisfactory. Nonetheless, a few biases suggest that sequential patient monitoring needs to be performed using the same analyzer. One limitation of this study was that we used different calibration materials. The development and use of common calibration materials might help reduce differences between these methods.
Acknowledgements
This work was supported by The Seoul St. Mary's Hospital IVD Medical Devices Development Center, Seoul, Korea. The funding organization played no role in study design, collection, analysis, or interpretation of data.
References
1. Bozeman CB, Carver BS, Eastham JA, Venable DD. Treatment of chronic prostatitis lowers serum prostate specific antigen. J Urol. 2002; 167:1723–1726. PMID: 11912396.
2. Sturgeon C. Tumor markers. In : Rifai N, Horvath AR, editors. Tietz textbook of clinical chemistry and molecular diagnostics. 6th ed. St. Louis: Elsevier;2018. p. 437–478. .
3. Boccon-Gibod L, Djavan WB, Hammerer P, Hoeltl W, Kattan MW, Prayer-Galetti T, et al. Management of prostate-specific antigen relapse in prostate cancer: a European Consensus. Int J Clin Pract. 2004; 58:382–390. PMID: 15161124.
4. Kort SA, Martens F, Vanpoucke H, van Duijnhoven HL, Blankenstein MA. Comparison of 6 automated assays for total and free prostate-specific antigen with special reference to their reactivity toward the WHO 96/670 reference preparation. Clin Chem. 2006; 52:1568–1574. PMID: 16762996.
5. Critz FA, Williams WH, Holladay CT, Levinson AK, Benton JB, Holladay DA, et al. Post-treatment PSA < or=0.2 ng/mL defines disease freedom after radiotherapy for prostate cancer using modern techniques. Urology. 1999; 54:968–971. PMID: 10604691.
6. Moul JW. Prostate specific antigen only progression of prostate cancer. J Urol. 2000; 163:1632–1642. PMID: 10799151.
7. Gheiler EL, Tefilli MV, Tiguert R, Grignon D, Cher ML, Sakr W, et al. Predictors for maximal outcome in patients undergoing salvage surgery for radio-recurrent prostate cancer. Urology. 1998; 51:789–795. PMID: 9610593.
8. Roach M 3rd, Hanks G, Thames H Jr, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006; 65:965–974. PMID: 16798415.
9. Ang M, Rajcic B, Foreman D, Moretti K, O'Callaghan ME. Men presenting with prostate-specific antigen (PSA) values of over 100 ng/mL. BJU Int. 2016; 117(S4):68–75. PMID: 26890320.
10. Gontero P, Joniau S, Van Poppel H. Radical prostatectomy for PSA> or =100 ng/mL prostate cancer. Eur Urol. 2008; 54:957–958. PMID: 18433984.
Fig. 1
Performance evaluation of four PSA automated analyzers using 120 samples. Passing-Bablok regression and Bland-Altman analysis of Immulite 2000Xpi and UniCel DXI 800 (A), Immulite 2000Xpi and ADVIA Centaur XPT (B), UniCel DXI 800 and ADVIA Centaur XPT (C), UniCel DXI 800 and ARICHITECT I2000SR (D), ARICHITECT I2000SR and ADVIA Centaur XPT (E), ARICHITECT I2000SR and Immulite 2000Xpi (F). Dotted lines in Bland-Altman plots indicate mean difference and mean difference±1.96 SD.
Abbreviation: PSA, prostate specific antigen.
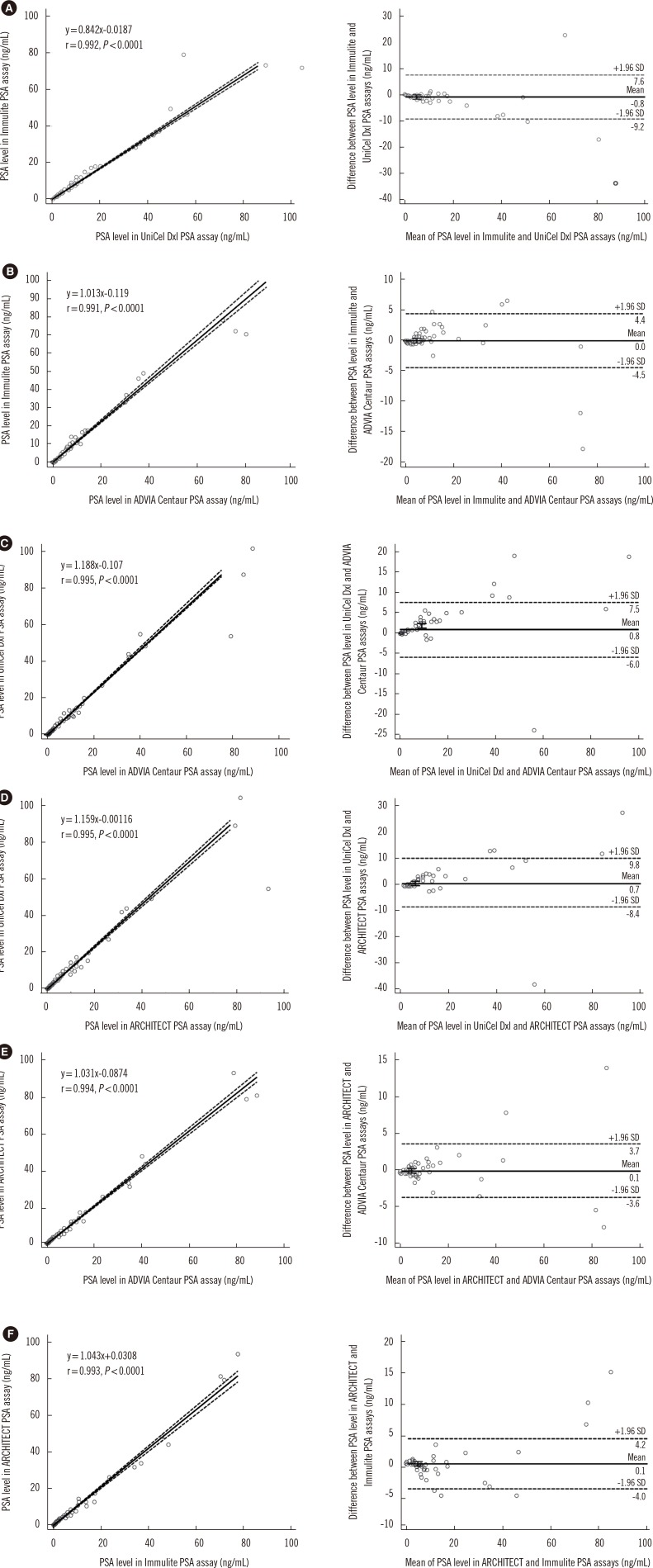
Table 1
Pearson correlation coefficients, mean bias, and concordance rates between four analyzers




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download