INTRODUCTION
Pinhole glasses with a series of multiple, equally-sized, regularly-placed pinholes are currently marketed in many countries for improving vision by reducing the circle of confusion and blocking peripheral aberration, increasing depth of focus (DOF), encouraging eye muscles to exercise and relax, and decreasing eye strain and discomfort. These claims are partly correct and partly incorrect. However, the United States Federal Trade Commission charged their unscientific and exaggerated advertisements in 1993 (
1).
For this reason, pinhole glasses have not been of interest to ophthalmic departments, and research on them has not been performed, even though multiple-pinhole (MPH) glasses may have some positive effects. In our previous study, we showed that MPH glasses improved uncorrected near and far visual acuity (VA), DOF, and accommodative amplitude; however, they reduced visual field (VF) sensitivity, contrast sensitivity (CS), and stereopsis (
2).
In contrast with single-pinhole (SPH) glasses, more than 100 pinholes are arranged in each lens of MPH glasses (
3). Therefore, MPH glasses are supposed to allow enough incident light rays through the MPHs to improve luminance behind the glasses, and wearers of pinhole glasses can easily identify the aperture that is perpendicular to their visual axis. To investigate the objective and subjective effects of MPH glasses, a comparison of functional changes induced by MPH and SPH glasses would be useful because the only difference between MPH and SPH glasses is the number of pinholes. However, differences in the functional changes between MPH and SPH glasses have not yet been studied. Also, no studies have verified claims by advertisements that pinhole glasses alleviate eye strain and fatigue and improve visual quality.
The purpose of this study was to compare ocular functional changes of pupil size, VA, DOF, accommodative amplitude, VF, CS, and stereopsis induced by MPH and SPH glasses. In addition, we measured reading speed and conducted surveys about ocular discomfort after reading among people using both types of pinhole glasses.
MATERIALS AND METHODS
We recruited people who visited our clinic for ocular examination and obtained informed consent from all participants from October 12th, 2015 to November 26th, 2015. Inclusion criteria were: 1) age between 20 and 45 years; 2) spherical equivalents (SE) within ± 6.0 diopters (D); 3) correctable distant and near VA by glasses up to 20/20; 4) normal intraocular pressure with normal optic disc appearance; and 5) normal ocular alignment. Exclusion criteria were: 1) disturbance of accommodation for any reason including Adie's pupil, Parkinson's disease, a history of previous ocular surgery or trauma, or systemic or topical medication that might affect accommodation; 2) corneal pathological features; 3) glaucoma; 4) cataracts of grade II or greater by the Lens Opacities Classification System III (LOCS III) (
4); or 5) vitreous and retinal abnormalities that might limit testing accuracy.
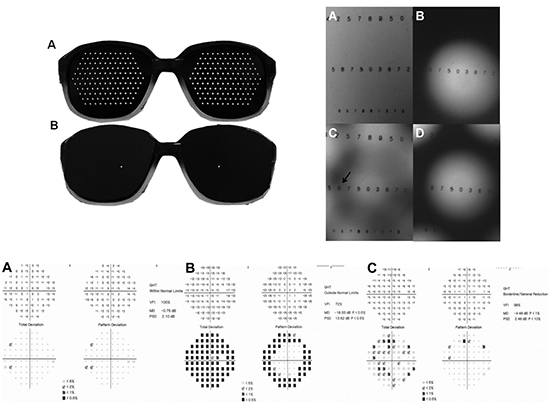
All participants had ocular examinations at baseline including manifest refraction, uncorrected distance and near VA, uncorrected near VA, corrected distance and near VA, pupil size, DOF, accommodative amplitude, standard automated perimetry, CS, and stereopsis. Detailed methodologies for these examinations were described in our previous report (
2). Briefly, distant VA was measured using a Snellen chart (Precision Vision, La Salle, IL, USA) at 4 m, and near VA was measured using the Logarithmic Visual Acuity Chart 2000 (Precision Vision) at 40 cm. Baseline pupil size under photopic conditions (85 cd/m
2) was measured using a WASCA Analyzer (Carl Zeiss Meditec, Oberkochen, Germany), and pupil size with MPH or SPH was measured using a ruler attached to the lateral rim of the glasses. Monocular DOF was assessed with a 4-m Snellen chart under distance correction without cycloplegics. Spherical defocus was induced by adding spherical lenses from −3.0 to +3.0 D in 0.25-D increments in a randomized order. We measured the range of defocus maintaining VA of 20/25 or better. Monocular accommodative amplitude (near point accommodation, NPA) was measured using Donder's push-up method (
5). VF tests were performed with a Humphrey Visual Field Analyzer (Carl Zeiss Meditec, Inc., Dublin, CA, USA) using the 30-2 Swedish interactive threshold algorithm. VF test time, visual field index (VFI), mean deviation (MD), and pattern standard deviation (PSD) were analyzed. Monocular CS tests were performed using a CSV-1000E contrast testing instrument (VectorVision, Dayton, OH, USA) at 2.5-m distance under standard brightness (85 cd/m
2), and stereopsis was measured with the Randot Stereotest (Stereo Optical Co., Chicago, IL, USA).
Reading speed was evaluated using a well-known traditional Korean fairy tale book printed in black-and-white at 10-point font size. The time to read a designated 10 pages with 3,985 letters was recorded, and reading speed was calculated as letters per second (LPS). Questionnaires about ocular symptoms were completed immediately after reading the book. We developed our questionnaire from a modified questionnaire for assessing virtual reality viewing with a head-mounted display (
6). Questionnaire items were sorted into 8 categories rated with a unipolar scale: tired eyes, eye strain, hot/burning sensation, ocular discomfort, difficulty focusing, difficulty concentrating, blurred vision, and double vision. A 7-grade scale (0–6) was used, and higher scores represented more severe symptoms.
After baseline examination, participants underwent the same examinations while wearing MPH and SPH glasses. Tests were administered one week apart, with the order of glasses type determined randomly. Although both eyes were examined, only data for the right eye were included in analysis for all measurements except stereopsis, reading speed, and ocular symptoms.
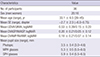
Trayner Pinhole Glasses (Trayner Glasses, Ivybridge Devon, UK) with 125 pinholes in each glass lens were used for the MPH glasses. SPH glasses were made by modifying MPH glasses by blocking all pinholes except a central hole on the visual axis, depending on participant's pupillary distance. This method maintained uniform features for the glasses such as vertex distance, pinhole size, and pinhole location (
Fig. 1).
Fig. 1
MPH glasses (A) and SPH glasses (B). SPH glasses were modified from MPH glasses by blocking all pinholes except a central hole on the visual axis.
MPH = multiple-pinhole, SPH = single-pinhole.

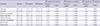
We took photographs to show the effects of SPH and MPH. The photographs were taken with an automated digital camera under 4 different conditions: photo without pinhole, with a SPH of 0.9-mm size, with MPHs of 3-mm size, and with MPHs of 2-mm size.
Statistical analysis
Paired t-tests were used to compare differences among measurements at baseline and when wearing MPH or SPH glasses. Statistical analyses were performed using SPSS software (ver. 19.0 for Windows; SPSS Inc., Chicago, IL, USA). Statistical significance was accepted for P values < 0.05.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Chung-Ang University Hospital Institutional Review Board (No. C2013115) and adhered to the tenets of the Declaration of Helsinki. Informed consent was submitted by all subjects when they were enrolled.
DISCUSSION
In this study, we determined objective and subjective changes in ocular functions and ocular symptoms induced by wearing MPH and SPH glasses. Compared with SPH, MPH induced less pupil dilation and improved VF indicators of MD, PSD, and VFI due to increased luminance and relatively preserved peripheral VF from the multiple apertures. However, no significant difference was observed between MPH and SPH glasses for uncorrected distance and near VA, DOF, accommodative amplitude, CS (except 12 cpd), and stereopsis. Reading speed using both types of pinhole glasses was significantly slower than baseline, and SPH glasses were associated with the slowest reading speed. Wearing either type of pinhole glasses resulted in ocular discomfort after reading. However, symptoms including tired eyes, eye strain, hot/burning sensation, eye discomfort, difficulty concentrating, blurred vision, and double vision were more severe with MPH glasses than with SPH glasses. We believe that this study has important implications as a trial that quantified the influence of both types of pinhole glasses on eye function. Our results supply evidence to verify that advertisements for these glasses are inaccurate.
Pupil size and luminance have a negative relationship (
7); thus, we can estimate the luminance behind the pinhole glasses using pupil size. Mean pupil size with SPH was considerably larger than the size at baseline and while wearing MPH glasses. Pupil size increased 30.9% (from 3.5 to 5.3 mm) while wearing MPH glasses and 68.6% (from 3.5 to 5.9 mm) with SPH glasses. According to the correlation curve of pupil diameter and luminance (
8), a 3.5-mm pupil diameter corresponds to photopic luminance, and pupil sizes of 5.3 and 5.9 mm with pinhole glasses correspond to mesopic luminance, even though measurements were under photopic conditions. The slope of the luminance change in the interval from 5.3 to 5.9 mm is relatively flat. Therefore, although pupil size was significantly different with MPH and SPH glasses, the gap in luminance might be small. This result indicated that both types of pinhole glasses induced low luminance, although luminance was lowest with SPH glasses.
VA while wearing both types of pinhole glasses improved due to the pinhole effect. A smaller aperture than the pupil can reduce the blur circle (
39) and block aberrant incident rays from the peripheral cornea and lens (
101112). Hence, pinhole glasses improved distant and near VA. The two types of pinhole glasses had the same pinhole aperture sizes, and VA was not significantly different with the 2 glasses types (
Fig. 2). However, image quality with pinhole glasses can be diminished when illumination reaching the retina is attenuated (
13). MPH glasses allow more incident rays to pass through the multiple apertures than SPH glasses, so SPH glasses might reduce illumination. This hypothesis is supported by the finding that wearing SPH glasses was associated with greater dilation in pupil diameter than wearing MPH glasses. However, contrary to our hypothesis, visual quality was better with SPH glasses or at least equal to quality with MPH glasses. We suggest that the reason for this result was that the central 15° range of vision was relatively intact with SPH glasses because incident rays were blocked only in the peripheral area outside of the central 15° (
Figs. 4 and
5B). In addition, central vision had increased contrast compared with baseline (
Fig. 5A) and was highlighted by the black occluder and enhanced by the pinhole effect. In contrast, MPHs sometimes resulted in blurred vision (
Fig. 5C) or induced double or triple vision based on the embraced number of pinholes within the participant's pupil (
3). Most participants complained about awareness of the MPHs that appeared as a honeycomb (
Fig. 5C and
5D) and the horizontal lines of the grating visible while blinking. These findings were demonstrated in our questionnaire results showing that MPH glasses resulted in more severe subjective symptoms of visual discomfort, difficulty concentrating, blurred vision, and double vision than SPH glasses (
Table 5). Thus, MPH glasses reduced the positive effects of luminance on visual quality.
Fig. 5
Photographs showing the effects of pinhole glasses on reading. It must be considered that photographs differ from actual vision while wearing pinhole glasses because they were taken with a digital camera. This simulation does not show the vertex distance between cornea and the glasses or correlation between participant's pupil size and pinhole interval. (A) The photograph shows the visual quality without pinhole. (B) There is peripheral VF constriction with a SPH, although blurring on the central field area was not observed. (C) There is no peripheral VF constriction; however, blurring in the overlapping area is observed with MPH of 3-mm size. (D) The overlapping image is not shown, but part of the central VF was blocked by the opaque pinhole edge with multiple pinholes of 2-mm size.
VF = visual field, SPH = single-pinhole, MPH = multiple-pinhole.

DOF and accommodative amplitude significantly increased while wearing both types of pinhole glasses because of the pinhole effect with the same aperture size of holes. DOF increased slightly with MPH glasses over SPH glasses, although the difference was not significant (
Fig. 3A). The reason for this finding might be the slightly better luminance with MPH glasses compared with SPH glasses because DOF depends on several factors including luminance, contrast, spatial frequency, visual target, VA, and pupil size (
1415). The small aperture of pinhole glasses requires less accommodative power for the same stimulus (
16). Thus, pinhole glasses can generate a larger amplitude of accommodation for a given stimulus compared with baseline. Because both types of pinhole glasses had the same aperture sizes, the results for amplitude of accommodation showed no significant difference between glasses types (
Fig. 3B).
The only difference between MPH and SPH glasses was the number of pinholes.
MPHs. Thus, we concluded that VF changes were induced by the number and location of pinholes. Central incident rays pass through the SPH aperture, but rays from the periphery are blocked by the opaque lenses of SPH glasses. This blocked about 15° of the peripheral area of the central 30° (
Figs. 4B and
5B), and VFI, MD, and PSD were markedly reduced. However, 125 incident rays of MPH glasses passed through the MPHs across the lens. Therefore, VFI, MD, and PSD were slightly less reduced compared to SPH, and the peripheral VF was preserved (
Table 2,
Fig. 4C).
CS and stereopsis while wearing both pinhole glasses decreased significantly compared with baseline due to decreased luminance behind the pinhole glasses. CS decreased significantly with both types of pinhole glasses at all four spatial frequencies. The decrease in CS was more prominent with increasing frequency. Because a decrease in luminance generally causes a decrease in CS (
1718), a small aperture with the lowest luminance with SPH glasses decreased CS with a greater effect at increasing frequency compared with MPH glasses (
819). The reason for the stereopsis results might also be that luminance affects stereopsis directly and proportionately (
2021). Stereopsis with both types of pinhole glasses showed a significant decline compared with baseline. However, differences in stereopsis between the types of pinhole glasses were not significant, because difference in luminance was not definite, and MPH glasses caused a blurring effect with overlapping images (
Fig. 5C). As a result, MPH glasses might have counteracted the positive effect of luminance on stereopsis.
Reading speed with SPH glasses was the slowest among the three conditions. Eye movement is important in the reading process (
22), and reading speed is hindered without proper eye movement (
23). In addition, healthy VF is necessary for effective reading, as indicated by the slower reading speed of glaucoma patients with bilateral VF loss than normal controls (
24). Wearing MPH or SPH glasses caused a peripheral VF disturbance or constriction (
Fig. 4); in particular, SPH glasses permitted only a central 15° VF. Hence, participants wearing pinhole glasses read books with their heads turning rather than using eye movement, and they could not quickly scan lines and pages.
Despite improvement in uncorrected near VA, DOF, and accommodative amplitude, ocular symptoms of tired eyes, eye strain, hot/burning sensation, ocular discomfort, difficulty focusing, difficulty concentrating, blurred vision, and double vision were significantly worse after reading with either type of pinhole glasses compared with baseline. In addition, although peripheral VF was preserved, MPH glasses generally resulted in more severe ocular symptoms than SPH glasses except for difficulty in focusing (
Table 5). We propose that the reasons for these results are: 1) decreased luminance inducing decreased CS and stereopsis causing participants to experience ocular discomfort and fatigue; 2) excessive effort to find the pinhole or fix the pinhole perpendicular to the visual axis; 3) cramping due to peripheral field constriction or blockage from the black plastic plate of the glasses; or 4) discomfort from after-images such as honeycomb images, horizontal grating, and double or triple vision. Advertisements state that MPH glasses reduce eye strain and ocular fatigue and improve visual quality, but our results indicate that those claims might not be true.
Our study has some limitations. All participants underwent the same ophthalmic examinations while wearing MPH or SPH glasses one week apart. Examinations were tests with no learning effects except for the VF test; however, the order of exams using MPH and SPH glasses was randomly chosen. Therefore, we believe that the examination order did not affect the validity of the results. Secondly, although the severity of dry eye could affect ocular discomfort, we did not assess it before ocular examinations. If there was significant difference in the severity at the one week interval, it could have produced an error in the analysis of results. Another limitation is that our study was performed with fixed settings for the MPH glasses with 125 pinholes of 0.9-mm fixed apertures with a 3-mm horizontal and vertical/3.5-mm diagonal arrangement. Even though this design is the most popular and widely used, differences in the number, size, or arrangement of pinholes could have different effects on luminance, image overlap, and final outcomes.
In conclusion, MPH and SPH glasses had positive effects on uncorrected distant and near VA, DOF, and accommodative amplitude due to the pinhole effect. However, they also had negative effects on visual function including VF, CS, stereopsis, reading speed, and ocular symptoms. Due to the increased luminance and preserved peripheral VF with MPH glasses, VF parameters and reading speed were better with MPH than with SPH glasses. In contrast to advertised claims, MPH glasses induced ocular discomfort after reading and greater visual disturbances than SPH glasses and baseline. Through future studies on ocular functional changes that depend on the arrangement, number, and size of pinholes, MPHs, we might be able to create a customized pinhole device that maximizes ocular function and minimizes ocular discomfort.












 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download